Abstract
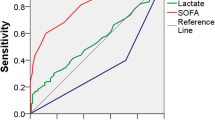
In 2016, in order to identify adult patients with sepsis who are likely to have poor outcomes, the Third International Consensus Definitions Task Force introduced a new bedside index, called the quick Sepsis-related Organ Failure Assessment (qSOFA) score. However, these new criteria have not been validated in the pediatric population. In this study, we sought to assess the qSOFA score for children with sepsis, who are being treated outside the pediatric intensive care units. The qSOFA criteria were revised and applied to a study population of 89 pediatric patients with sepsis, admitted in a pediatric tertiary referral center from 2006 to 2016. The analysis of prognostic performance of qSOFA score for the prediction of severe sepsis showed a sensitivity of 46% (95% CI, 27–67%), a specificity of 74% (95% CI, 62–85%), a positive predictive value of 43% (95% CI, 34–52%), and a negative predictive value of 77% (95% CI, 71–82%). The area under ROC curve for qSOFA score ≥ 2 was 0.602 (95% CI 0.492–0.705).
Conclusion: The qSOFA score showed a low accuracy to identify children in the pediatric ward at risk for severe sepsis. Clinical tools are needed to facilitate the diagnosis of impending organ dysfunction in pediatric infection outside of the ICU.
What is Known: • One of the major challenges for clinicians is to identify and recognize children with sepsis and impending organ dysfunction, in the emergency and in the pediatric department. • In 2016, members of the Sepsis-3 task force proposed qSOFA, an empirically derived score using simple clinical criteria, to assist clinicians in identifying adult patients with sepsis at risk for poor outcome. | |
What is New: • qSOFA demonstrated insufficient clinical value to be recommended as a screening tool for pediatric sepsis outside ICU. • D-dimer level and blood glucose may be useful biomarkers to identify children at risk for severe sepsis. |



Similar content being viewed by others
Abbreviations
- BP:
-
Blood pressure
- ICU:
-
Intensive care units
- IQR:
-
Interquartile range
- NPV:
-
Negative predictive values
- PPV:
-
Positive predictive values
- PICU:
-
Pediatric intensive care units
- qSOFA:
-
Quick Sepsis-related Organ Failure Assessment
- PSCC:
-
Pediatric Sepsis Consensus Congress
- ROC:
-
Receiver operating characteristic
- SD:
-
Standard deviation
- SE:
-
Sensibility
- SIRS:
-
Systemic inflammatory response syndrome
- SOFA:
-
Sequential [Sepsis-related] Organ Failure Assessment
- SP:
-
Specificity
- SS:
-
Severe sepsis
References
Agyeman PK, Schlapbach LJ, Giannoni E, Stocker M, Posfay-Barbe KM, Heininger U, Schindler M, Korten I, Konetzny G, Niederer-Loher A, Kahlert CR (2017) Epidemiology of blood culture-proven bacterial sepsis in children in Switzerland: a population-based cohort study. Lancet Child Adolesc Health 1:124–133
Asakura H, Ontachi Y, Mizutani T, Kato M, Ito T, Saito M, Morishita E, Yamazaki M, Suga Y, Miyamoto KI, Nakao S (2001) Depressed plasma activity of plasminogen or alpha2 plasmin inhibitor is not due to consumption coagulopathy in septic patients with disseminated intravascular coagulation. Blood Coagul Fibrinolysis 12:275–281
Barron R, Freebairn R (2010) Electrolyte disorders in the critically ill. Anaesth Intensive Care Med 11:523–528
Biban P, Gaffuri M, Spaggiari S, Zaglia F, Serra A, Santuz P (2012) Early recognition and management of septic shock in children. Pediatr Rep 4:e13
Branco RG, Tasker RC (2007) Glycemic level in mechanically ventilated children with bronchiolitis. Pediatr Crit Care Med 8:546–550
Churpek MM, Snyder A, Han X, Sokol S, Pettit N, Howell MD, Edelson DP (2017) Quick sepsis-related organ failure assessment, systemic inflammatory response syndrome, and early warning scores for detecting clinical deterioration in infected patients outside the intensive care unit. Am J Respir Crit Care Med 195:906–911
Dhainaut JF, Shorr AF, Macias WL, Kollef MJ, Levi M, Reinhart K, Nelson DR (2005) Dynamic evolution of coagulopathy in the first day of severe sepsis: relationship with mortality and organ failure. Crit Care Med 33:341–348
Fleischmann-Struzek C, Goldfarb DM, Schlattmann P, Schlapbach LJ, Reinhart K, Kissoon N (2018) The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir Med 6:223–230
Freund Y, Lemachatti N, Krastinova E, Van Laer M, Claessens YE, Avondo A, Occelli C, Feral-Pierssens AL, Truchot J, Ortega M, Carneiro B (2017) Prognostic accuracy of Sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. JAMA 317:301–308
Goldstein B, Giroir B, Randolph A (2005) International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 6:2–8
Goldstein B, Giroir B, Randolph A (2005) Letters to the editor. Pediatr Crit Care Med 6:500–501
Green J, Doughty L, Kaplan SS, Sasser H, Carcillo JA (2002) The tissue factor and plasminogen activator inhibitor type-1 response in pediatric sepsis-induced multiple organ failure. Thromb Haemost 87:218–223
Hall NJ, Peters M, Eaton S, Pierro A (2004) Hyperglycemia is associated with increased morbidity and mortality rates in neonates with necrotizing enterocolitis. J Pediatr Surg 9:898–901
Khilnani P, Singhi S, Lodha R, Santhanam I, Sachdev A, Chugh K, Jaishree M, Ranjit S, Ramachandran B, Ali U, Udani S (2010) Pediatric sepsis guidelines: summary for resource-limited countries. Indian J Crit Care Med 14:41–52
Kidokoro A, Iba T, Fukunaga M, Yagi Y (1996) Alterations in coagulation and fibrinolysis during sepsis. Shock 5:223–228
Klein GW, Hojsak JM, Schmeidler J, Rapaport R (2008) Hyperglycemia and outcome in the pediatric intensive care unit. J Pediatr 153:379–384
Leteurtre S, Duhamel A, Salleron J, Grandbastien B, Lacroix J, Leclerc F, Groupe Francophone de Réanimation et d’Urgences Pédiatriques (2013) PELOD-2: an update of the pediatric logistic organ dysfunction score. Crit Care Med 41:1761–1773
Levi M, Van der Poll T, Ten Cate H, Van Deventer SJ (1997) The cytokine-mediated imbalance between coagulant and anticoagulant mechanisms in sepsis and endotoxaemia. Eur J Clin Investig 27:3–9
Hu L, Zhu Y, Chen M, Li X, Lu X, Liang Y, Tan H (2016) Development and validation of a disease severity scoring model for pediatric sepsis. Iran J Public Health 45:875
Mace SE (2001) The pediatric patient with acute respiratory failure: clinical diagnosis and pathophysiology. Pediatr Emerg Med Rep 6:21–32
Matics TJ, Sanchez-Pinto LN (2017) Adaptation and validation of a pediatric sequential organ failure assessment score and evaluation of the Sepsis-3 definitions in critically ill children. JAMA Pediatr 171:e172352
McCowen K, Malhotra A, Bistrian B (2001) Stress-induced hyperglycemia. Crit Care Clin 17:107–124
Müller B, Becker KL, Kränzlin M, Schächinger H, Huber PR, Nylen ES, Snider RH, White JC, Schmidt-Gayk H, Zimmerli W, Ritz R (2000) Disordered calcium homeostasis of sepsis: association with calcitonin precursors. Eur J Clin Investig 30:823–831
Patton L, Young V (2017) Effectiveness of provider strategies for the early recognition of clinical deterioration due to sepsis in pediatric patients: a systematic review protocol. JBI Database Syst Rev Implement Rep 15:76–85
Pawar A, Raut A, Kalrao V, Jacob J, Godha I, Thomas R (2016) Etiology and clinical outcomes of neonatal and pediatric sepsis. Arch Pediatr Infect Dis 4:e33602
Raith EP, Udy AA, Bailey M, McGloughlin S, MacIsaac C, Bellomo R, Pilcher DV (2017) Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA 317:290–300
Rhee C, Gohil S, Klompas M (2014) Regulatory mandates for sepsis care reasons for caution. N Engl J Med 370:1673–1676
Schlapbach LJ, Straney L, Bellomo R, MacLaren G, Pilcher D (2018) Prognostic accuracy of age-adapted SOFA, SIRS, PELOD-2, and qSOFA for in-hospital mortality among children with suspected infection admitted to the intensive care unit. Intensive Care Med 44:179–188
Schwameis M, Steiner MM, Schoergenhofer C, Lagler H, Buchtele N, Jilma-Stohlawetz P, Boehm T, Jilma B (2015) D-dimer and histamine in early stage bacteremia: a prospective controlled cohort study. Eur J Inter Med 26:782–786
Scott HF, Deakyne SJ, Woods JM, Bajaj L (2015) The prevalence and diagnostic utility of systemic inflammatory response syndrome vital signs in a pediatric emergency department. Acad Emerg Med 22:381–389
Sharma D, Jelacic J, Chennuri R, Chaiwat O, Chandler W, Vavilala MS (2009) Incidence and risk factors for perioperative hyperglycemia in children with traumatic brain injury. Anesth Analg 108:81–89
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315:801–810
Song SK, Karl IE, Ackerman JL, Hotchkiss RS (1993) Increased intracellular Ca2+: a critical link in the pathophysiology of sepsis? Proc Natl Acad Sci 90:3933–3937
Steele T, Kolamunnage-Dona R, Downey C, Toh CH, Welters I (2013) Assessment and clinical course of hypocalcemia in critical illness. Crit Care 17:R106
Verhoeven JJ, Hokken-Koelega AC, den Brinker M, Hop WC, van Thiel RJ, Bogers AJ, Helbing WA, Joosten KF (2011) Disturbance of glucose homeostasis after pediatric cardiac surgery. Pediatr Cardiol 32:131–138
Weiss SL, Fitzgerald JC, Pappachan J, Wheeler D, Jaramillo-Bustamante JC, Salloo A, Singhi SC, Erickson S, Roy JA, Bush JL, Nadkarni VM (2015) Global epidemiology of pediatric severe sepsis: the sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med 191:1147–1157
Wintergerst KA, Buckingham B, Gandrud L, Wong BJ, Kache S, Wilson DM (2006) Association of hypoglycemia, hyperglycemia, and glucose variability with morbidity and death in the pediatric intensive care unit. Pediatrics 118:173–179
Yates AR, Dyke PC, Taeed R, Hoffman TM, Hayes J, Feltes TF, Cua CL (2006) Hyperglycemia is a marker for poor outcome in the postoperative pediatric cardiac patient. Pediatr Crit Care Med 7:351–355
Author information
Authors and Affiliations
Contributions
All authors had full access to all of the data for this study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This retrospective study was approved by the Regional Ethics Committee of Marche (reference number 2017-0064 OR).
Informed consent
For this type of study, formal consent is not required.
Additional information
Communicated by Nicole Ritz
Rights and permissions
About this article
Cite this article
Zallocco, F., Osimani, P., Carloni, I. et al. Assessment of clinical outcome of children with sepsis outside the intensive care unit. Eur J Pediatr 177, 1775–1783 (2018). https://doi.org/10.1007/s00431-018-3247-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3247-2