Abstract
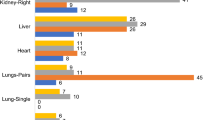
Approximately 2% of those on the organ transplant list in the UK are children. Early identification of donors and referral to organ donation teams (ODT) has proven to increase both the success rate of gaining consent and the number of organs actually retrieved. To evaluate the practice relating to organ donation for children receiving end-of-life care on a paediatric intensive care unit (PICU) measured against the National Guidelines. All children 0–18 who received their end-of-life care and died on the PICU. A retrospective cohort study of organ donation patterns including referral, approach, consent and donation. This involved a review of case notes on PICU between the years 2009 and 2014. One hundred five deaths were identified and 100 notes were examined and data analysed to ascertain if religion, age and length of stay on PICU impacted on practice. Eighty-six children met the early identification criteria for potential donors, 40 (46.5%) children were referred to the ODT and 33 (38.3%) families were approached regarding donation. Twenty-one (24.4%) families consented to donation. Seventeen donations took place with a total of 41 sets of organs/tissues retrieved. Despite the majority of children meeting early identification for potential donors, many were not being referred.
Conclusions: All children on end-of-life care should be referred for potential organ donation. Organ donation needs to be seen as a priority for hospitals as a part of routine end-of-life care to help increase referral rates and give families the opportunity to donate. Many paediatric deaths are not referred for consideration of organ donation, despite guidelines stating that this process should be standard of care. Further optimization of referral rates may aid in increasing the number of organs available for donation.
What is Known: • Shortage of organs continues to be a national problem. • NICE guidelines state that all patients who are on end-of-life care should have the option of organ donation explored. • Required referral both increases the number of donors and organs donated. |
What is New: • The process of identifying and referring children for paediatric organ donation. • Identifies that children are still not being referred for organ donation. • Organ donation is still not a priority for hospitals. |


Similar content being viewed by others
References
Allen J & Hulme W (2014) Potential donor audit: summary report for the 12 month period 1st April 2013-31st March 2014. Available at: http://www.odt.nhs.uk/pdf/pda_report_1314.pdf
Bratton S, Kolovos N, Roach E et al (2006) Pediatric organ transplantation needs: organ donation best practices. Arch Pediatr Adolesc Med 160:468–472
Brierley J (2010) Paediatric organ donation in the UK. Arch Dis Child 95:83–88
Brierley J, Hasan A (2012) Aspects of deceased organ donation in paediatrics. Br J Anaesth 108:92–95
Burris G, Jacobs A (1996) A continuous quality improvement process to increase organ and tissue donation. J Transpl Coord 6(2):88–92. https://doi.org/10.7182/prtr.1.6.2.a075l132ll54516h
Dickerson J, Valadaka A, Levert T et al (2002) Organ donation rates in a neurosurgical intensive care unit. J Neurosurg 97:811–814
General Medical Council. Treatment and care towards the end of life: good practice in decision making. GMC 2010
Godown J, McKane M, Wujcik K, et al. Expanding the donor pool: regional variation in pediatric organ donation rates. Pediatr Transplant, Dec 2016, 20(8) p1093–1097
González-Vílchez F1, Segovia Cubero J2, Almenar L3, Crespo-Leiro MG4, Arizón JM5, Villa A6, Delgado J7, Roig E8, Lage E9, González-Costello J10; Spanish Heart Transplantation Teams. Spanish Heart Transplantation Registry. 26th Official Report of the Spanish Society of Cardiology Working Group on Heart Failure and Heart Transplantation (1984-2014). Rev Esp Cardiol (Engl Ed). 2015 Nov; 68(11):1008–21. doi: https://doi.org/10.1016/j.rec.2015.07.009. Epub 2015 Oct 9
Gortmaker S, Beasley C, Brigham L et al (1996) Organ donor potential and performance: size and nature of the organ donor shortfall. J Crit Care Med 24:432–439
National Institute of Clinical Excellence. Organ donation for transplantation: improving donor identification and consent rates for deceased organ donation. NICE 2011
NHS BLOOD AND TRANSPLANT. Transplant saves lives. 2014 Available at: http://www.organdonation.nhs.uk/newsroom/fact_sheets/transplants_save_lives.asp
Rodrigue J, Cornell D, Howard R (2008) Pediatric organ donation: what factors most influence parents’ donation decisions? Pediatr Crit Care Med 9:80
Shafer T, Wagner D, Chessare J et al (2008) US organ donation breakthrough collaborative increases organ donation. Critical Care Nursing Quarterly 31:190–210
Siminoff L, Gordon N, Hewlett J, Et a (2001) Factors influencing families’ consent for donation of solid organs for transplantation. JAMA 286(1):71–77. https://doi.org/10.1001/jama.286.1.71
Tsai E, Shemie S, COX P et al (2000) Organ donation in children: role of the pediatric intensive care unit. Pediatr Crit Care Med 1(2):156–160. https://doi.org/10.1097/00130478-200010000-00012
West R, Burr G (2002) Why families deny consent to organ donation. Aust Crit Care 15(1):27–32. https://doi.org/10.1016/S1036-7314(02)80041-8
Author information
Authors and Affiliations
Contributions
Laura Carone: Involved in study design, collection and analysis of data, drafting and revising the article and gave final approval of the submitted version
Phoebe Kigozi: Involved in analysis of data, drafting and revising the article and gave final approval of the submitted version.
Shrirang Alurkar: Involved in study design, collection and analysis of data, drafting and revising the article and gave final approval of the submitted version
Harish Vyas: Involved in study design, collection and analysis of data, drafting and revising the article and gave final approval of the submitted version.
All authors contributed to the data collection, analysis and writing of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors state that they do not have a financial relationship with Nottingham University Hospitals NHS Trust.
Additional information
Communicated by Piet Leroy
Rights and permissions
About this article
Cite this article
Carone, L., Alurkar, S., Kigozi, P. et al. Organ and tissue donation in a regional paediatric intensive care unit: evaluation of practice. Eur J Pediatr 177, 709–714 (2018). https://doi.org/10.1007/s00431-017-3084-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-017-3084-8