Abstract
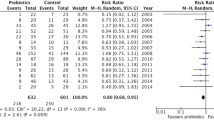
Probiotics may benefit in cystic fibrosis (CF) as gut dysbiosis is associated with gastrointestinal symptoms and exacerbation of respiratory symptoms in CF. We conducted a systematic review of randomized controlled trials (RCTs) and non-RCTs of probiotic supplementation in children with CF, using the Cochrane methodology, preferred reporting items for systematic reviews (PRISMA) statement, and meta-analysis of observational studies in epidemiology (MOOSE) guidelines. Primary outcomes were pulmonary exacerbations, duration of hospitalization and antibiotics, and all-cause mortality. Secondary outcomes included gastrointestinal symptoms, markers of gut inflammation, and intestinal microbial balance. A total of nine studies (RCTs, 6, non-RCTs, 3; N = 275) with some methodological weaknesses were included in the review. The pooled estimate showed significant reduction in the rate of pulmonary exacerbation (fixed effects model, two parallel group RCTs and one cross-over trial: relative risk (RR) 0.25, (95 % confidence interval (95 % CI) 0.15,0.41); p < 0.00001; level of evidence: low) and decrease in fecal calprotectin (FCLP) levels (fixed effect model, three RCTs: mean difference (MD) −16.71, 95 % CI −27.30,−6.13); p = 0.002; level of evidence: low) after probiotic supplementation. Probiotic supplementation significantly improved gastrointestinal symptoms (one RCT, one non-RCT) and gut microbial balance (decreased Proteobacteria, increased Firmicutes, and Bacteroides in one RCT, one non-RCT).
Conclusion: Limited low-quality evidence exists on the effects of probiotics in children with CF. Well-designed adequately powered RCTs assessing clinically meaningful outcomes are required to study this important issue.
What is Known: • Gut dysbiosis is frequent in children with cystic fibrosis due to frequent exposure to pathogens and antibiotics. • Probiotics decrease gut dysbiosis and improve gut maturity and function. |
What is New: • This comprehensive systematic review shows that current evidence on the safety and efficacy of probiotics in children with cystic fibrosis is limited and of low quality. • Well-designed and adequately powered trials assessing clinically important outcomes are required considering the health burden of cystic fibrosis and the potential benefits of probiotics. |




Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CF:
-
Cystic fibrosis
- FCLP:
-
Fecal calprotectin
- FEV:
-
Forced expiratory volume
- GI:
-
Gastrointestinal
- LGG:
-
Lactobacillus GG
- RCT:
-
Randomized controlled trial
- RNO:
-
Rectal nitric oxide
- ORS:
-
Oral rehydration solution
References
AlFaleh K, Anabrees J (2014) Probiotics for prevention of necrotizing enterocolitis in preterm infants. The Cochrane database. Syst Rev 4:Cd005496. doi:10.1002/14651858.CD005496.pub4
Bermudez-Brito M, Plaza-Diaz J, Munoz-Quezada S, Gomez-Llorente C, Gil A (2012) Probiotic mechanisms of action. Ann Nutr Metab 61(2):160–174
Borowitz D, Gelfond D (2013) Intestinal complications of cystic fibrosis. Curr Opin Pulm Med 19(6):676–680
Boyle RJ, Bath-Hextall FJ, Leonardi-Bee J, Murrell DF, Tang ML (2008) Probiotics for treating eczema. Cochrane Database Syst Rev (4):Cd006135. doi:10.1002/14651858.CD006135.pub2
Bruzzese E, Raia V, Gaudiello G, Polito G, Buccigrossi V, Formicola V, Guarino A (2004) Intestinal inflammation is a frequent feature of cystic fibrosis and is reduced by probiotic administration. Aliment Pharmacol Ther 20(7):813–819
Bruzzese E, Raia V, Spagnuolo MI, Volpicelli M, De Marco G, Maiuri L, Guarino A (2007) Effect of lactobacillus GG supplementation on pulmonary exacerbations in patients with cystic fibrosis: a pilot study. Clin Nutr (Edinburgh, Scotland) 26(3):322–328
Bruzzese E, Callegari ML, Raia V, Viscovo S, Scotto R, Ferrari S, Morelli L, Buccigrossi V, Lo Vecchio A, Ruberto E, Guarino A (2014) Disrupted intestinal microbiota and intestinal inflammation in children with cystic fibrosis and its restoration with Lactobacillus GG: a randomised clinical trial. PLoS One 9(2):e87796. doi:10.1371/journal.pone.0087796
Bunn SK, Bisset WM, Main MJ, Gray ES, Olson S, Golden BE (2001) Fecal calprotectin: validation as a noninvasive measure of bowel inflammation in childhood inflammatory bowel disease. J Pediatr Gastroenterol Nutr 33(1):14–22
Canani RB, Cirillo P, Bruzzese E, Graf M, Terrin G, Gaudiello G, De Curtis M, Cucchiara S, Guarino A (2002) Nitric oxide production in rectal dialysate is a marker of disease activity and location in children with inflammatory bowel disease. Am J Gastroenterol 97(6):1574–1576. doi:10.1111/j.1572-0241.2002.05757.x
Canani RB, Terrin G, Rapacciuolo L, Miele E, Siani MC, Puzone C, Cosenza L, Staiano A, Troncone R (2008) Faecal calprotectin as reliable non-invasive marker to assess the severity of mucosal inflammation in children with inflammatory bowel disease. Dig Liver Dis 40(7):547–553. doi:10.1016/j.dld.2008.01.017
Chapman CM, Gibson GR, Rowland I (2011) Health benefits of probiotics: are mixtures more effective than single strains? Eur J Nutr 50(1):1–17
Croft NM, Marshall TG, Ferguson A (1995) Gut inflammation in children with cystic fibrosis on high-dose enzyme supplements. Lancet 346(8985):1265–1267
Cystic Fibrosis Foundation (1994) Mycrobiology and infectious disease in cystic fibrosis. Consensus conferences: concept in care. Bethesda Vol V, sect
Dagli E, Warner JA, Besley CR, Warner JO (1992) Raised serum soluble interleukin-2 receptor concentrations in cystic fibrosis patients with and without evidence of lung disease. Arch Dis Child 67(4):479–481
De Vos M, Louis EJ, Jahnsen J, Vandervoort JG, Noman M, Dewit O, D’Haens GR, Franchimont D, Baert FJ, Torp RA, Henriksen M, Potvin PM, Van Hootegem PP, Hindryckx PM, Moreels TG, Collard A, Karlsen LN, Kittang E, Lambrecht G, Grimstad T, Koch J, Lygren I, Coche JC, Mana F, Van Gossum A, Belaiche J, Cool MR, Fontaine F, Maisin JM, Muls V, Neuville B, Staessen DA, Van Assche GA, de Lange T, Solberg IC, Vander Cruyssen BJ, Vermeire SA (2013) Consecutive fecal calprotectin measurements to predict relapse in patients with ulcerative colitis receiving infliximab maintenance therapy. Inflamm Bowel Dis 19(10):2111–2117
del Campo R, Garriga M, Perez-Aragon A, Guallarte P, Lamas A, Maiz L, Bayon C, Roy G, Canton R, Zamora J, Baquero F, Suarez L (2014) Improvement of digestive health and reduction in proteobacterial populations in the gut microbiota of cystic fibrosis patients using a Lactobacillus reuteri probiotic preparation: a double blind prospective study. J Cyst Fibros 13(6):716–722
Di Benedetto LRV, Pastore A, Albano F, Spagnuolo MI, DeVizia B, Guarino A (1998) Lactobacillus casei strain GG as adjunctive treatment to children with cystic fibrosis. J Pediatr Gastroenterol Nutr 26(5):542
Di Nardo G, Oliva S, Menichella A, Pistelli R, De Biase RV, Patriarchi F, Cucchiara S, Stronati L (2014) Lactobacillus reuteri ATCC55730 in cystic fibrosis. J Pediatr Gastroenterol Nutr 58(1):81–86
Duytschaever G, Huys G, Bekaert M, Boulanger L, De Boeck K, Vandamme P (2011) Cross-sectional and longitudinal comparisons of the predominant fecal microbiota compositions of a group of pediatric patients with cystic fibrosis and their healthy siblings. Appl Environ Microbiol 77(22):8015–8024
Duytschaever G, Huys G, Bekaert M, Boulanger L, De Boeck K, Vandamme P (2013) Dysbiosis of Bifidobacteria and Clostridium cluster XIVa in the cystic fibrosis fecal microbiota. J Cystic Fibros 12(3):206–215
Eren Z, Gurol Y, Sonmezoglu M, Eren HS, Celik G, Kantarci G (2014) Saccharomyces cerevisiae fungemia in an elderly patient following probiotic treatment. Mikrobiyoloji bulteni 48(2):351–355
Fagerberg UL, Loof L, Merzoug RD, Hansson LO, Finkel Y (2003) Fecal calprotectin levels in healthy children studied with an improved assay. J Pediatr Gastroenterol Nutr 37(4):468–472
Fallahi G, Motamed F, Yousefi A, Shafieyoun A, Najafi M, Khodadad A, Farhmand F, Ahmadvand A, Rezaei N (2013) The effect of probiotics on fecal calprotectin in patients with cystic fibrosis. Turk J Pediatr 55(5):475–478
Franko B, Vaillant M, Recule C, Vautrin E, Brion JP, Pavese P (2013) Lactobacillus paracasei endocarditis in a consumer of probiotics. Medecine et maladies infectieuses 43(4):171–173
Garcia-Sanchez V, Iglesias-Flores E, Gonzalez R, Gisbert JP, Gallardo-Valverde JM, Gonzalez-Galilea A, Naranjo-Rodriguez A, de Dios-Vega JF, Muntane J, Gomez-Camacho F (2010) Does fecal calprotectin predict relapse in patients with Crohn’s disease and ulcerative colitis? J Crohn’s Colitis 4(2):144–152
M. Garriga AdB, M. Burreros, P. Guallarte, A. Perez-Aragon, A. Lamas, del Campo R., L. Suarez (2013) Probiotic intake improves the gastrointestinal health of cystic fibrosis patients. Paper presented at the J Cyst Fibros
Ghadimi D, Vrese M, Heller KJ, Schrezenmeir J (2010) Effect of natural commensal-origin DNA on toll-like receptor 9 (TLR9) signaling cascade, chemokine IL-8 expression, and barrier integritiy of polarized intestinal epithelial cells. Inflamm Bowel Dis 16(3):410–427
Gillanders LEJ, Gilpin D, Schneiders T, Tunney MT (2011) The airway microbiome in cystic fibrosis: challenges for therapy. Therapy 8(645e):60
Gionchetti P, Rizzello F, Venturi A, Brigidi P, Matteuzzi D, Bazzocchi G, Poggioli G, Miglioli M, Campieri M (2000) Oral bacteriotherapy as maintenance treatment in patients with chronic pouchitis: a double-blind, placebo-controlled trial. Gastroenterology 119(2):305–309
Grimoud J, Durand H, de Souza S, Monsan P, Ouarne F, Theodorou V, Roques C (2010) In vitro screening of probiotics and synbiotics according to anti-inflammatory and anti-proliferative effects. Int J Food Microbiol 144(1):42–50
Guarino A (2015) Effects of LGG administration in children with cystic fibrosis: a randomized controlled trial. Effects of LGG administration in children with cystic fibrosis: a randomized controlled trial: Federico II University
Guslandi M, Mezzi G, Sorghi M, Testoni PA (2000) Saccharomyces boulardii in maintenance treatment of Crohn’s disease. Dig Dis Sci 45(7):1462–1464
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical research ed) 336(7650):924–926
Hawrelak JA, Myers SP (2004) The causes of intestinal dysbiosis: a review. Altern med review 9(2):180–197
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical researched) 343:d5928. doi:10.1136/bmj.d5928
Hoen AG, Li J, Moulton LA, O’Toole GA, Housman ML, Koestler DC, Guill MF, Moore JH, Hibberd PL, Morrison HG, Sogin ML, Karagas MR, Madan JC (2015) Associations between gut microbial colonization in early life and respiratory outcomes in cystic fibrosis. J Pediatr 167(1):138–147 e131-133
Iannitti T, Palmieri B (2010) Therapeutical use of probiotic formulations in clinical practice. Clin Nutr (Edinburgh, Scotland) 29(6):701–725
Infante Pina D, Redecillas Ferreiro S, Torrent Vernetta A, Segarra Canton O, Maldonado Smith M, Gartner Tizziano L, Hidalgo Albert E (2008) Improvement of intestinal function in cystic fibrosis patients using probiotics. Anales de Pediatria (Barcelona, Spain: 2003) 69(6):501–505
Isolauri E, Salminen S, Ouwehand AC (2004) Microbial-gut interactions in health and disease. Probiotics. Best Pract Res Clin Gastroenterol 18(2):299–313. doi:10.1016/j.bpg.2003.10.006
Jafari SA, Mehdizadeh-Hakkak A, Kianifar HR, Hebrani P, Ahanchian H, Abbasnejad E (2013) Effects of probiotics on quality of life in children with cystic fibrosis; a randomized controlled trial. Iran J Pediatr 23(6):669–674
Jensen H, Dromtorp SM, Axelsson L, Grimmer S (2014) Immunomodulation of monocytes by probiotic and selected lactic acid bacteria. Probiotics Antimicrob Proteins. doi:10.1007/s12602-014-9174-2
Ki Cha B, Mun Jung S, Hwan Choi C, Song ID, Woong Lee H, Joon Kim H, Hyuk J, Kyung Chang S, Kim K, Chung WS, Seo JG (2012) The effect of a multispecies probiotic mixture on the symptoms and fecal microbiota in diarrhea-dominant irritable bowel syndrome: a randomized, double-blind, placebo-controlled trial. J Clin Gastroenterol 46(3):220–227
Kim JY, Kwon JH, Ahn SH, Lee SI, Han YS, Choi YO, Lee SY, Ahn KM, Ji GE (2010) Effect of probiotic mix (Bifidobacterium bifidum, Bifidobacterium lactis, Lactobacillus acidophilus) in the primary prevention of eczema: a double-blind, randomized, placebo-controlled trial. Pediatr. Allerg Immunol 21(2 Pt 2):e386–e393. doi:10.1111/j.1399-3038.2009.00958.x
Lasson A, Stotzer PO, Ohman L, Isaksson S, Sapnara M, Strid H (2015) The intra-individual variability of faecal calprotectin: a prospective study in patients with active ulcerative colitis. J Crohn’s Colitis 9(1):26–32
Li F, Sheng XY (2014) Research advances in the role of fecal calprotectin in intestinal development and diseases among children. Zhongguo dang dai er ke za zhi [Chinese Journal of Contemporary Pediatrics] 16(10):1064–1069
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical researched) 339:b2700. doi:10.1136/bmj.b2700
Lin YP, Thibodeaux CH, Pena JA, Ferry GD, Versalovic J (2008) Probiotic Lactobacillus reuteri suppress proinflammatory cytokines via c-Jun. Inflamm Bowel Dis 14(8):1068–1083
Macfarlane GT, Blackett KL, Nakayama T, Steed H, Macfarlane S (2009) The gut microbiota in inflammatory bowel disease. Current Pharmaceutical Design BMJ Open 15(13):1528–1536
Navas-Lopez VM, Giron B-AJ, Fernandez-Crehuet F, Serrano Nieto MJ, Vicioso Recio MI, Sierra Salinas C (2013) Intestinal inflammation in cystic fibrosis: lack of effectiveness after treatment with mesalamine and probiotics. In: Ann Nutr Metab. Conference absract: 20th International Congress of Nutrition Granada Spain (63):1694–1695
Ng SC, Hart AL, Kamm MA, Stagg AJ, Knight SC (2009) Mechanisms of action of probiotics: recent advances. Inflamm Bowel Dis 15(2):300–310
Olafsdottir E, Aksnes L, Fluge G, Berstad A (2002) Faecal calprotectin levels in infants with infantile colic, healthy infants, children with inflammatory bowel disease, children with recurrent abdominal pain and healthy children. Acta paediatrica (Oslo, Norway: 1992) 91(1):45–50
Ooi CY (2016) Probioticss and the early life effects on intestinal bacteria and inflammation in children with cystic fibrosis (PEARL-CF): Sydney Children’s Hospitals Network. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=370881. Accessed on 16 Aug 2016
Osborn DA, Sinn JK (2007) Probiotics in infants for prevention of allergic disease and food hypersensitivity. Cochrane Database Syst Rev (4):Cd006475. doi:10.1002/14651858.CD006475.pub2
O’Toole PW, Cooney JC (2008) Probiotic bacteria influence the composition and function of the intestinal microbiota. Interdiscip Perspect Infect Dis 2008:175285. doi:10.1155/2008/175285
Preidis GA, Saulnier DM, Blutt SE, Mistretta TA, Riehle KP, Major AM, Venable SF, Finegold MJ, Petrosino JF, Conner ME, Versalovic J (2012) Probiotics stimulate enterocyte migration and microbial diversity in the neonatal mouse intestine. Gastroenterology 26(5):1960–1969
Rogers GB, Carroll MP, Hoffman LR, Walker AW, Fine DA, Bruce KD (2010) Comparing the microbiota of the cystic fibrosis lung and human gut. Gut Microbes 1(2):85–93. doi:10.4161/gmic.1.2.11350
Sánchez-Calvo JM, Garcia-Castillo M, Lamas A, Rodriguez-Baños M, Máiz L, Suárez L, Baquero F, Canton R, del Campo R (2008) Gut microbiota composition in cystic fibrosis patients: molecular approach and classical culture. J Cyst Fibros 7(Suppl. 2):S50
Scotto G (2011) Globalization and infectious diseases: the past and future. Le infezioni in medicina: rivista periodica di eziologia, epidemiologia, diagnostica, clinica e terapia delle patologie infettive 19(1):56–61
Shoaib A, Dachang W, Xin Y (2015) Determining the role of a probiotic in the restoration of intestinal microbial balance by molecular and cultural techniques. Genet Mol Res: GMR 14(1):1526–1537
Smyth RL, Croft NM, O’Hea U, Marshall TG, Ferguson A (2000) Intestinal inflammation in cystic fibrosis. Arch Dis Child 82(5):394–399
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283(15):2008–2012
Summerton CB, Longlands MG, Wiener K, Shreeve DR (2002) Faecal calprotectin: a marker of inflammation throughout the intestinal tract. Eur J Gastroenterol Hepatol 14(8):841–845
Tena D, Martinez NM, Losa C, Fernandez C, Medina MJ, Saez-Nieto JA (2013) Acute acalculous cholecystitis complicated with peritonitis caused by lactobacillus plantarum. Diagn Microbiol Infect Dis 76(4):510–512
Tena D, Losa C, Medina MJ, Saez-Nieto JA (2014) Peritonitis caused by Bifidobacterium longum: case report and literature review. Anaerobe 27:27–30
Thomas CM, Versalovic J (2010) Probiotics-host communication: modulation of signaling pathways in the intestine. Gut Microbes 1(3):148–163
Thomas CM, Hong T, van Pijkeren JP, Hemarajata P, Trinh DV, Hu W, Britton RA, Kalkum M, Versalovic J (2012) Histamine derived from probiotic Lactobacillus reuteri suppresses TNF via modulation of PKA and ERK signaling. PLoS One 7(2):e31951. doi:10.1371/journal.pone.0031951
Treggiari MM, Rosenfeld M, Mayer-Hamblett N, Retsch-Bogart G, Gibson RL, Williams J, Emerson J, Kronmal RA, Ramsey BW (2009) Early anti-pseudomonal acquisition in young patients with cystic fibrosis: rationale and design of the EPIC clinical trial and observational study. Contemp Clin Trials 30(3):256–268
Varni JW, Burwinkle TM, Seid M (2006) The PedsQL 4.0 as a school population health measure: feasibility, reliability, and validity. Qual Life Res: an International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation 15(2):203–215
Weiss B, Efrati O (2014) The effects of probiotics on sputum bacteria, sputum inflammation and pulmonary infections in patients with cystic fibrosis: a double-blind placebo controlled trial: Sheba Medical Center. https://clinicaltrials.gov/ct2/show/NCT01201434. Accessed on 16 Aug 2016
Weiss B, Bujanover Y, Yahav Y, Vilozni D, Fireman E, Efrati O (2010) Probiotic supplementation affects pulmonary exacerbations in patients with cystic fibrosis: a pilot study. Pediatr Pulmonol 45(6):536–540
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2013). The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Werlin SL, Benuri-Silbiger I, Kerem E, Adler SN, Goldin E, Zimmerman J, Malka N, Cohen L, Armoni S, Yatzkan-Israelit Y, Bergwerk A, Aviram M, Bentur L, Mussaffi H, Bjarnasson I, Wilschanski M (2010) Evidence of intestinal inflammation in patients with cystic fibrosis. J Pediatr Gastroenterol Nutr 51(3):304–308. doi:10.1097/MPG.0b013e3181d1b013
Wong VW, Won GL, Chim AM, Chu WC, Yeung DK, Li KC, Chan HL (2013) Treatment of nonalcoholic steatohepatitis with probiotics. A proof-of-concept study. Ann Hepato 12(2):256–262
Zein EF, Karaa S, Chemaly A, Saidi I, Daou-Chahine W, Rohban R (2008) Lactobacillus rhamnosus septicemia in a diabetic patient associated with probiotic use: a case report. Ann Biol Clin 66(2):195–198
Author’s contribution
AA is responsible for literature review, analysis, and writing the first draft. HB is responsible for literature review and analysis. SR is responsible for synthesis and checking the first and the final versions of the manuscript. SP is responsible for concept, supervision, interpretation of results, and checking the first and the final versions of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Communicated by Beat Steinmann
Rights and permissions
About this article
Cite this article
Ananthan, A., Balasubramanian, H., Rao, S. et al. Probiotic supplementation in children with cystic fibrosis—a systematic review. Eur J Pediatr 175, 1255–1266 (2016). https://doi.org/10.1007/s00431-016-2769-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-016-2769-8