Abstract
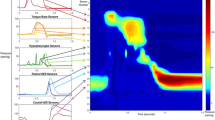
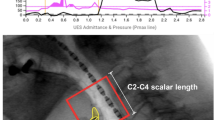
Pressure-flow analysis allows assessing esophageal bolus transport in relation to esophageal pressures. This study aimed to characterize pressure-flow metrics in relation to dysphagia in paediatric patients. We analysed esophageal pressure-impedance recordings of 5 ml liquid and viscous swallows from 35 children (17 M, mean 10.5 ± 0.8 years). Primary indication for referral was gastroesophageal reflux disease (GERD) (9), post-fundoplication dysphagia (5), idiopathic dysphagia (16), trachea-esophageal fistula (2) and other (3). Peristaltic function was assessed using the 20 mmHg iso-contour defect and the timing between bolus pressure and flow was assessed using the Pressure Flow Index, a metric elevated in relation to dysphagia. Patients were stratified in relation to dysphagia and to peristaltic defect size. Dysphagia was characterized by a weaker peristalsis for liquids and higher Pressure Flow Index for viscous. When patients were stratified based on weak or normal peristalsis, dysphagia with weak peristalsis related to a larger iso-contour defect size and dysphagia with normal peristalsis related to higher Pressure Flow Index.
Conclusion: Pressure-flow analysis enables differentiation of patients with dysphagia due to weak peristalsis (poor bolus clearance) from abnormal bolus flow resistance (esophageal outflow obstruction). This new dichotomous categorization of esophageal function may help guide the selection of optimal treatment such as pharmacological or endoscopic therapy.
What is Known: • Pressure-flow analysis (PFA) can detect abnormalities in esophageal motility using integrated analysis of bolus propulsion and bolus flow during swallowing. • AIM analysis has recently been reported to be useful in identifying subtle pre-operative esophageal dysfunction in adult patients who developed post-fundoplication dysphagia as well as in patients with non-obstructive dysphagia. |
What is New: • Pressure-flow parameters can distinguish the cause of dysphagia in paediatric patients. • Combined high-resolution manometry and impedance measurements with pressure-flow analysis can differentiate paediatric patients with dysphagia symptoms in relation to either weak peristalsis (poor bolus clearance) or over-pressurization (abnormal bolus flow resistance). |
How might it impact on clinical practice in the future? • This study supports the use of a novel objective analysis method on recordings that are readily used in paediatric clinical practice. • The pressure-flow approach allows discriminating esophageal dysfunction in relation to dysphagia symptoms in children. This has not been achieved in children with current analysis methods. • The new findings of this study allow a dichotomous categorization of esophageal function, which may help to guide the selection of the most optimal treatment such as pharmacological or endoscopic therapy. |





Similar content being viewed by others
Abbreviations
- AIM:
-
Automated impedance manometry
- EGJ:
-
Esophago-gastric junction
- EPT:
-
Esophageal pressure topography
- GERD:
-
Gastroesophageal reflux disease
- HRM:
-
High-resolution manometry
- HRMI:
-
High-resolution manometry impedance
- IBP:
-
Intrabolus pressure
- IBP slope:
-
Intrabolus pressure slope
- ICD:
-
Iso-contour defect
- IRP:
-
Integrated relaxation pressure
- NS:
-
Not significant
- PFI:
-
Pressure Flow Index
- PNI:
-
Pressure at nadir impedance
- PP:
-
Peak pressure
- TNIPP:
-
Time from nadir impedance to peak pressure
References
Bogte A, Bredenoord A, Oors J et al (2012) Relationship between esophageal contraction patterns and clearance of swallowed liquid and solid boluses in healthy controls and patients with dysphagia. Neurogastroenterol Motil 24:e364–e372
Bredenoord AJ, Fox M, Kahrilas PJ et al (2012) And the international high resolution manometry working group. Chicago Classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Mot 24(suppl1):57–65
Chen C-L, Yi C-H, Liu T-T, Hsu C-S, Omari TI (2013) Characterization of esophageal pressure-flow abnormalities in patients with non-obstructive dysphagia and normal manometry findings. J Gastroenterol Hepatol 28:946–953
Ghosh SK, Pandolfino JE, Zhang Q et al (2006) Quantifying esophageal peristalsis with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol 290:G988–G997
Gyawali CP et al (2013) Evaluation of esophageal motor function in clinical practice. Neurogastroenterol Motil 25:99–133
Kahrilas PJ, Clouse RE, Hogan WJ (1994) American Gastroenterological Association technical review on the clinical use of esophageal manometry. Gastroenterology 107:1865–1884
Lazarescu G, Karamanolis G, Aprile L, De Oliviera R, Dantas R, Sifrim D (2010) Perception of dysphagia: lack of correlation with objective measurements of esophageal function. Neurogastroenterol Motil 22:1292–e337
Loots C, van Herwaarden MY, Benninga MA, VanderZee DC, van Wijk MP, Omari TI (2013) Gastroesophageal reflux, esophageal function, gastric emptying, and the relationship to dysphagia before and after antireflux surgery in children. J Pediatr 162(3):566–573
Lundquist A, Olsson R, Ekberg O (1998) Clinical and radiological evaluation reveals high prevalence of abnormalities in young adults with dysphagia. Dysphagia 13:202–207
Massey BT, Dodds WJ, Hogan WJ et al (1991) Abnormal esophageal motility. An analysis of concurrent radiographic and manometric findings. Gastroenterology 101:344–354
Myers JC, Nguyen NQ, Jamieson GG et al (2012) Susceptibility to dysphagia after fundoplication revealed by novel automated impedance manometry analysis. Neurogastroenterol Mot 24(9):812–e393
Nguyen NQ, Ching K, Tippett M, Smout AJPM, Holloway RH (2010) Impact of nadir lower oesophageal sphincter pressure on bolus clearance assessed by combined manometry and multi-channel intra-luminal impedance measurement. Neurogastroenterol Motil 22:50–55
Nguyen NQ, Holloway RH, Smout AJ, Omari TI (2013) Automated impedance-manometry analysis detects esophageal motor dysfunction in patients who have non-obstructive dysphagia with normal manometry. Neurogastroenterol Motil 25(3):238–245
Nguyen NQ, Rigda R, Tippett M et al (2005) Assessment of oesophageal motor function using combined perfusion manometry and multi-channel intra-luminal impedance measurement in normal subjects. Neurogastroenterol Motil 17:458–465
Nguyen NQ, Tippett M, Smout AJPM, Holloway RH (2006) Relationship between pressure wave amplitude and esophageal bolus clearance assessed by combined manometry and multichannel intraluminal impedance measurement. Am J Gastroenterol 101:2476–2484
Omari TI, Dejaeger E, van Beckevoort D et al (2011) A method to objectively assess swallow function in adults with suspected aspiration. Gastroenterology 140:1454–1463
Omari T, Tack J, Rommel N (2014) Impedance as an adjunct to manometric testing: what it has failed to do and what it may tell us in the future. Eur J Gastroenterol 2(5):355–366
Omari TI, Wauters L, Rommel N, Kritas S, Myers JC (2013) Oesophageal pressure-flow metrics in relation to bolus volume, bolus consistency, and bolus perception. United Eur Gastroenterol J 1(4):249–258
Ott DJ, Richter JE, Chen YM et al (1987) Esophageal radiography and manometry: correlation in 172 patients with dysphagia. Am J Roentgenol 149:307–311
Pandolfino JE, Ghosh SK, Zhang Q et al (2006) Quantifying EGJ morphology and relaxation with high-resolution manometry; a study of 75 asymptomatic volunteers. Am J Gastrointest Liver Physiol 290:G1033–G1040
Roman S, Lin Z, Kwiatek MA, Pandolfino JE, Kahrilas PJ (2011) Weak peristalsis in esophageal pressure topography: classification and association with dysphagia. Am J Gastroenteral 106:349–356
Rommel N, Selleslagh M, Haesendonck N, Hellemans M, Kritas S, Omari T, Hoffman I, Tack J (2014) Clinical challenges of esophageal high resolution manometry in pediatrics: acquisition and analysis. Gastroenterology 146(5):S1–S419
Rommel N, Van Oudenhove L, Tack J, Omari TI (2014) Automated impedance manometry analysis as a method to assess esophageal function. Neurogastroenterol Motil 1–10
Singendonck M et al (2014) Applying the Chicago Classification criteria of esophageal motility to a pediatric cohort: effects of patient age and size. Neurogastroenterol Motil 26(9):1333–1341
Authors’ contribution
Nathalie Rommel is responsible for the study concept and design, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript, statistical analysis and study supervision. Taher I. Omari is responsible for the study concept and design, analysis and interpretation of data, drafting of the manuscript, critical revision and study supervision. Margot Selleslagh is responsible for the analysis of data and critical revision of the manuscript. Stamatiki Kritas is responsible for the analysis of data and critical revision of the manuscript. Charles Cock is responsible for the critical revision of the manuscript. Rachel Rosan is responsible for the data acquisition and critical revision of the manuscript. Leonel Rodriguez is responsible for the data acquisition and critical revision of the manuscript. Samuel Nurko is responsible for the study concept and design, acquisition, analysis and interpretation of data, critical revision and study supervision.
Conflict of interest
T Omari and N Rommel have AIM technology patent to disclose. None of the other authors have any conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Peter de Winter
Rights and permissions
About this article
Cite this article
Rommel, N., Omari, T.I., Selleslagh, M. et al. High-resolution manometry combined with impedance measurements discriminates the cause of dysphagia in children. Eur J Pediatr 174, 1629–1637 (2015). https://doi.org/10.1007/s00431-015-2582-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-015-2582-9