Abstract
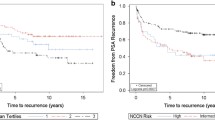
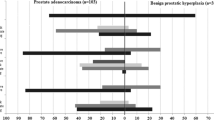
Cadherins seem to play and important role in prostate cancer (PCa) progression. E-cadherin loss of expression has been associated with poor prognosis; P-cadherin’s role is still elusive. Although pT3 PCa is often considered “high-risk cancer,” it does not exhibit an uniformly poor prognosis. Herein, we assessed the prognostic value and survival impact of E-cadherin and P-cadherin immunoexpression in pT3 PCa. Radical prostatectomy (RP) specimens from 102 pT3 PCa patients treated between 1991 and 2014 in a single institution were designated for E-cadherin and P-cadherin immunoexpression analysis. A representative block from each specimen was selected for tissue micro-array (TMA) construction, using 3 cores per case. E-cadherin immunoexpression was assessed via a digital image analysis system. For P-cadherin, scoring criteria for HER2 in gastric cancer were used. Clinical records of all patients were reviewed for baseline clinical/pathologic characteristics and follow-up data. E-cadherin-low PCa patients displayed worse disease-specific survival (DSS), although not reaching statistical significance (HR 2.65, 95%CI 0.81–7.88). However, considering the pT3b group only, those with low E-cadherin immunoexpression displayed significantly worse overall-survival (OS) and DSS (HR 3.69, 95%CI 1.18–11.50; HR 5.90, 95%CI 1.40–24.81). No significant differences in survival were found for P-cadherin differential immunoexpression. Furthermore, an association between E-cadherin and P-cadherin immunoexpression (p = 0.019) was found, as among E-cadherin-low PCa, 96.6% were P-cadherin negative. We demonstrated that low E-cadherin immunoexpression discriminates among pT3b PCa patients those with poorer survival and which might benefit from specific therapy. The role of P-cadherin in PCa seems context-dependent deserving further investigation.




Similar content being viewed by others
References
Attard G, Parker C, Eeles RA, Schröder F, Tomlins SA, Tannock I, Drake CG, de Bono JS (2016) Prostate cancer. Lancet 387(10013):70–82. https://doi.org/10.1016/S0140-6736(14)61947-4
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67(1):7–30. https://doi.org/10.3322/caac.21387
Etzioni R, Penson DF, Legler JM, di Tommaso D, Boer R, Gann PH, Feuer EJ (2002) Overdiagnosis due to prostate-specific antigen screening: lessons from U.S. prostate cancer incidence trends. J Natl Cancer Inst 94(13):981–990
Potosky AL, Miller BA, Albertsen PC, Kramer BS (1995) The role of increasing detection in the rising incidence of prostate cancer. JAMA 273(7):548–552
Stephenson RA, Smart CR, Mineau GP, James BC, Janerich DT, Dibble RL (1996) The fall in incidence of prostate carcinoma. On the down side of a prostate specific antigen induced peak in incidence—data from the Utah Cancer registry. Cancer 77(7):1342–1348. https://doi.org/10.1002/(SICI)1097-0142(19960401)77:7<1342::AID-CNCR18>3.0.CO;2-1
Tsaur I, Noack A, Makarevic J, Oppermann E, Waaga-Gasser AM, Gasser M, Borgmann H, Huesch T, Gust KM, Reiter M, Schilling D, Bartsch G, Haferkamp A, Blaheta RA (2015) CCL2 chemokine as a potential biomarker for prostate cancer: a pilot study. Cancer Res Treat 47(2):306–312. https://doi.org/10.4143/crt.2014.015
Barqawi AB, Krughoff KJ, Eid K (2012) Current challenges in prostate cancer management and the rationale behind targeted focal therapy. Adv Urol 2012:862639–862637. https://doi.org/10.1155/2012/862639
Miller GJ, Torkko KC (2001) Natural history of prostate cancer--epidemiologic considerations. Epidemiol Rev 23(1):14–18
Adolfsson J, Rönström L, Carstensen J, Löwhagen T, Hedlund PO (1990) The natural course of low grade, non-metastatic prostatic carcinoma. Br J Urol 65(6):611–614
Bostwick DG, Graham SD, Napalkov P, Abrahamsson PA, di Sant'agnese PA, Algaba F, Hoisaeter PA, Lee F, Littrup P, Mostofi FK (1993) Staging of early prostate cancer: a proposed tumor volume-based prognostic index. Urology 41(5):403–411
Johansson JE, Andrén O, Andersson SO, Dickman PW, Holmberg L, Magnuson A, Adami HO (2004) Natural history of early, localized prostate cancer. JAMA 291(22):2713–2719. https://doi.org/10.1001/jama.291.22.2713
Bauer JJ, Connelly RR, Seterhenn IA, Deausen J, Srivastava S, McLeod DG, Moul JW (1998) Biostatistical modeling using traditional preoperative and pathological prognostic variables in the selection of men at high risk for disease recurrence after radical prostatectomy for prostate cancer. J Urol 159(3):929–933
Drivalos A, Chrisofos M, Efstathiou E, Kapranou A, Kollaitis G, Koutlis G, Antoniou N, Karanastasis D, Dimopoulos MA, Bamias A (2016) Expression of α5-integrin, α7-integrin, Ε-cadherin, and N-cadherin in localized prostate cancer. Urol Oncol 34(4):165.e111–165.e168. https://doi.org/10.1016/j.urolonc.2015.10.016
Edge SB, Compton CC (2010) The American joint committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–1474. https://doi.org/10.1245/s10434-010-0985-4
Van Poppel H, Joniau S (2008) An analysis of radical prostatectomy in advanced stage and high-grade prostate cancer. Eur Urol 53(2):253–259. https://doi.org/10.1016/j.eururo.2007.10.009
Yossepowitch O, Eggener SE, Bianco FJ, Carver BS, Serio A, Scardino PT, Eastham JA (2007) Radical prostatectomy for clinically localized, high risk prostate cancer: critical analysis of risk assessment methods. J Urol 178(2):493–499; discussion 499. https://doi.org/10.1016/j.juro.2007.03.105
Deng QK, Lei YG, Lin YL, Ma JG, Li WP (2016) Prognostic value of protocadherin10 (PCDH10) methylation in serum of prostate cancer patients. Med Sci Monit 22:516–521
Soler AP, Harner GD, Knudsen KA, McBrearty FX, Grujic E, Salazar H, Han AC, Keshgegian AA (1997) Expression of P-cadherin identifies prostate-specific-antigen-negative cells in epithelial tissues of male sexual accessory organs and in prostatic carcinomas. Implications for prostate cancer biology. Am J Pathol 151(2):471–478
Berx G, Van Roy F (2001) The E-cadherin/catenin complex: an important gatekeeper in breast cancer tumorigenesis and malignant progression. Breast Cancer Res 3(5):289–293
Liu YN, Liu Y, Lee HJ, Hsu YH, Chen JH (2008) Activated androgen receptor downregulates E-cadherin gene expression and promotes tumor metastasis. Mol Cell Biol 28(23):7096–7108. https://doi.org/10.1128/MCB.00449-08
Van Aken E, De Wever O, Correia da Rocha AS, Mareel M (2001) Defective E-cadherin/catenin complexes in human cancer. Virchows Arch 439(6):725–751
Mareel M, Oliveira MJ, Madani I (2009) Cancer invasion and metastasis: interacting ecosystems. Virchows Arch 454(6):599–622. https://doi.org/10.1007/s00428-009-0784-0
Makrilia N, Kollias A, Manolopoulos L, Syrigos K (2009) Cell adhesion molecules: role and clinical significance in cancer. Cancer Investig 27(10):1023–1037. https://doi.org/10.3109/07357900902769749
Bae KM, Parker NN, Dai Y, Vieweg J, Siemann DW (2011) E-cadherin plasticity in prostate cancer stem cell invasion. Am J Cancer Res 1(1):71–84
Onder TT, Gupta PB, Mani SA, Yang J, Lander ES, Weinberg RA (2008) Loss of E-cadherin promotes metastasis via multiple downstream transcriptional pathways. Cancer Res 68(10):3645–3654. https://doi.org/10.1158/0008-5472.CAN-07-2938
Lazari P, Poulias H, Gakiopoulou H, Thomopoulou GH, Barbatis C, Lazaris AC (2013) Differential immunohistochemical expression of CD44s, E-cadherin and β-catenin among hyperplastic and neoplastic lesions of the prostate gland. Urol Int 90(1):109–116. https://doi.org/10.1159/000345057
Pontes J, Srougi M, Borra PM, Dall’ Oglio MF, Ribeiro-Filho LA, Leite KR (2010) E-cadherin and beta-catenin loss of expression related to bone metastasis in prostate cancer. Appl Immunohistochem Mol Morphol 18(2):179–184. https://doi.org/10.1097/PAI.0b013e3181640bca
Uchikado Y, Okumura H, Ishigami S, Setoyama T, Matsumoto M, Owaki T, Kita Y, Natsugoe S (2011) Increased slug and decreased E-cadherin expression is related to poor prognosis in patients with gastric cancer. Gastric Cancer 14(1):41–49. https://doi.org/10.1007/s10120-011-0004-x
Hulpiau P, van Roy F (2009) Molecular evolution of the cadherin superfamily. Int J Biochem Cell Biol 41(2):349–369. https://doi.org/10.1016/j.biocel.2008.09.027
Albergaria A, Ribeiro AS, Vieira AF, Sousa B, Nobre AR, Seruca R, Schmitt F, Paredes J (2011) P-cadherin role in normal breast development and cancer. Int J Dev Biol 55(7–9):811–822. https://doi.org/10.1387/ijdb.113382aa
Vieira AF, Paredes J (2015) P-cadherin and the journey to cancer metastasis. Mol Cancer 14:178. https://doi.org/10.1186/s12943-015-0448-4
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, Mason M, Matveev V, Wiegel T, Zattoni F, Mottet N, EAo U (2014) EAU guidelines on prostate cancer. Part II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol 65(2):467–479. https://doi.org/10.1016/j.eururo.2013.11.002
Tang LH, Berlin J, Branton P, Burgart LJ, Carter DK, Compton CC, Fitzgibbons P, Frankel WL, Jessup J, Kakar S, Minsky B, Nakhleh R, Washington K (2013) Protocol for the examination of specimens from patients with carcinoma of the stomach. Gastrointestinal - Stomach, vol Stomach 3.2.0.1. College of American Pathologists (CAP). Based on AJCC/UICC TNM, 7th edition. http://www.cap.org/cancerprotocols. Accessed 1 Oct 2017
Abdelrahman AE, Arafa SA, Ahmed RA (2017) Prognostic value of Twist-1, E-cadherin and EZH2 in prostate Cancer: an Immunohistochemical study. Turk Patoloji Derg 1(1):198–210. https://doi.org/10.5146/tjpath.2016.01392
Howlader N, Noone A, Krapcho M, Miller D, Bishop K, Kosary C, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis D, Chen H, Feuer E, Cronin K (2017) SEER Cancer Statistics Review, 1975–2014, National Cancer Institute. https://seer.cancer.gov/csr/1975_2014/, based on November 2016 SEER data submission, posted to the SEER web site, April 2017. Bethesda, MD
Epstein JI, Zelefsky MJ, Sjoberg DD, Nelson JB, Egevad L, Magi-Galluzzi C, Vickers AJ, Parwani AV, Reuter VE, Fine SW, Eastham JA, Wiklund P, Han M, Reddy CA, Ciezki JP, Nyberg T, Klein EA (2016) A contemporary prostate cancer grading system: a validated alternative to the Gleason score. Eur Urol 69(3):428–435. https://doi.org/10.1016/j.eururo.2015.06.046
Berney DM, Beltran L, Fisher G, North BV, Greenberg D, Møller H, Soosay G, Scardino P, Cuzick J (2016) Validation of a contemporary prostate cancer grading system using prostate cancer death as outcome. Br J Cancer 114(10):1078–1083. https://doi.org/10.1038/bjc.2016.86
Isbarn H, Huland H, Graefen M (2013) Results of radical prostatectomy in newly diagnosed prostate cancer: long-term survival rates in locally advanced and high-risk cancers. Dtsch Arztebl Int 110(29–30):497–503. https://doi.org/10.3238/arztebl.2013.0497
Jeong BC, Chalfin HJ, Lee SB, Feng Z, Epstein JI, Trock BJ, Partin AW, Humphreys E, Walsh PC, Han M (2015) The relationship between the extent of extraprostatic extension and survival following radical prostatectomy. Eur Urol 67(2):342–346. https://doi.org/10.1016/j.eururo.2014.06.015
Richmond PJ, Karayiannakis AJ, Nagafuchi A, Kaisary AV, Pignatelli M (1997) Aberrant E-cadherin and alpha-catenin expression in prostate cancer: correlation with patient survival. Cancer Res 57(15):3189–3193
Loric S, Paradis V, Gala JL, Berteau P, Bedossa P, Benoit G, Eschwège P (2001) Abnormal E-cadherin expression and prostate cell blood dissemination as markers of biological recurrence in cancer. Eur J Cancer 37(12):1475–1481
van Oort IM, Tomita K, van Bokhoven A, Bussemakers MJ, Kiemeney LA, Karthaus HF, Witjes JA, Schalken JA (2007) The prognostic value of E-cadherin and the cadherin-associated molecules alpha-, beta-, gamma-catenin and p120ctn in prostate cancer specific survival: a long-term follow-up study. Prostate 67(13):1432–1438. https://doi.org/10.1002/pros.20626
Behnsawy HM, Miyake H, Harada K, Fujisawa M (2013) Expression patterns of epithelial-mesenchymal transition markers in localized prostate cancer: significance in clinicopathological outcomes following radical prostatectomy. BJU Int 111(1):30–37. https://doi.org/10.1111/j.1464-410X.2012.11551.x
Whiteland H, Spencer-Harty S, Thomas DH, Davies C, Morgan C, Kynaston H, Bose P, Fenn N, Lewis PD, Bodger O, Jenkins S, Doak SH (2013) Putative prognostic epithelial-to-mesenchymal transition biomarkers for aggressive prostate cancer. Exp Mol Pathol 95(2):220–226. https://doi.org/10.1016/j.yexmp.2013.07.010
Ma D, Zhou Z, Yang B, He Q, Zhang Q, Zhang XH (2015) Association of molecular biomarkers expression with biochemical recurrence in prostate cancer through tissue microarray immunostaining. Oncol Lett 10(4):2185–2191. https://doi.org/10.3892/ol.2015.3556
Paredes J, Figueiredo J, Albergaria A, Oliveira P, Carvalho J, Ribeiro AS, Caldeira J, Costa AM, Simões-Correia J, Oliveira MJ, Pinheiro H, Pinho SS, Mateus R, Reis CA, Leite M, Fernandes MS, Schmitt F, Carneiro F, Figueiredo C, Oliveira C, Seruca R (2012) Epithelial E- and P-cadherins: role and clinical significance in cancer. Biochim Biophys Acta 1826(2):297–311. https://doi.org/10.1016/j.bbcan.2012.05.002
Bussemakers MJ, van Moorselaar RJ, Giroldi LA, Ichikawa T, Isaacs JT, Takeichi M, Debruyne FM, Schalken JA (1992) Decreased expression of E-cadherin in the progression of rat prostatic cancer. Cancer Res 52(10):2916–2922
Umbas R, Isaacs WB, Bringuier PP, Schaafsma HE, Karthaus HF, Oosterhof GO, Debruyne FM, Schalken JA (1994) Decreased E-cadherin expression is associated with poor prognosis in patients with prostate cancer. Cancer Res 54(14):3929–3933
Arenas MI, Romo E, Royuela M, Fraile B, Paniagua R (2000) E-, N- and P-cadherin, and alpha-, beta- and gamma-catenin protein expression in normal, hyperplastic and carcinomatous human prostate. Histochem J 32(11):659–667
Gravdal K, Halvorsen OJ, Haukaas SA, Akslen LA (2007) A switch from E-cadherin to N-cadherin expression indicates epithelial to mesenchymal transition and is of strong and independent importance for the progress of prostate cancer. Clin Cancer Res 13(23):7003–7011. https://doi.org/10.1158/1078-0432.CCR-07-1263
Jarrard DF, Paul R, van Bokhoven A, Nguyen SH, Bova GS, Wheelock MJ, Johnson KR, Schalken J, Bussemakers M, Isaacs WB (1997) P-cadherin is a basal cell-specific epithelial marker that is not expressed in prostate cancer. Clin Cancer Res 3(11):2121–2128
Paredes J, Correia AL, Ribeiro AS, Albergaria A, Milanezi F, Schmitt FC (2007) P-cadherin expression in breast cancer: a review. Breast Cancer Res 9(5):214. https://doi.org/10.1186/bcr1774
Imai K, Hirata S, Irie A, Senju S, Ikuta Y, Yokomine K, Harao M, Inoue M, Tsunoda T, Nakatsuru S, Nakagawa H, Nakamura Y, Baba H, Nishimura Y (2008) Identification of a novel tumor-associated antigen, cadherin 3/P-cadherin, as a possible target for immunotherapy of pancreatic, gastric, and colorectal cancers. Clin Cancer Res 14(20):6487–6495. https://doi.org/10.1158/1078-0432.CCR-08-1086
De Craene B, Berx G (2013) Regulatory networks defining EMT during cancer initiation and progression. Nat Rev Cancer 13(2):97–110. https://doi.org/10.1038/nrc3447
Thiery JP, Acloque H, Huang RY, Nieto MA (2009) Epithelial-mesenchymal transitions in development and disease. Cell 139(5):871–890. https://doi.org/10.1016/j.cell.2009.11.007
Funding
This study was supported by project CI-IPOP-17-2015 (Epigenetic signature of prostate cancer stem cells) funded by the Research Centre of Portuguese Oncology Institute of Porto. JL is supported by an FCT—Fundação para a Ciência e Tecnologia—fellowship (grant number SFRH/BD/132751/2017).
Author information
Authors and Affiliations
Contributions
CF, JL, and RH designed the study; CF, JL, and PL performed technical procedures and acquired pathological and clinical data; CF, JL, CJ and RH analyzed and interpreted data; CF, JL, and LA performed statistical analysis; CF drafted the manuscript; all authors reviewed and approved the final version of the manuscript. All individuals listed as co-authors of the manuscript have significantly contributed to this study.
Corresponding author
Ethics declarations
This study was approved by the institutional ethics committee of Portuguese Oncology Institute Porto (Comissão de Ética para a Saúde do IPO Porto—CES 235/2017).
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ferreira, C., Lobo, J., Antunes, L. et al. Differential expression of E-cadherin and P-cadherin in pT3 prostate cancer: correlation with clinical and pathological features. Virchows Arch 473, 443–452 (2018). https://doi.org/10.1007/s00428-018-2406-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-018-2406-1