Abstract
Although the majority of lung adenocarcinomas show mixed pattern, only the predominant component is taken into account according to the novel classification. We evaluated the proportion of different patterns and their impact on overall survival (OS) and disease-free survival (DFS). Patterns were recorded according to predominance and their proportions were rated and calculated by objective area measuring on digitalized, annotated slides of resected stage I lung adenocarcinomas. Spearman’s rank correlation, Kaplan-Meier models and the log rank test were used for statistical evaluation. Two hundred forty-three stage I adenocarcinoma were included. Lepidic pattern is more frequent in tumours without recurrence (20 vs. 8%), and lepidic predominant tumours have favourable prognosis (OS 90.5%, DFS 89.4%), but proportions above 25% are not associated with improving outcome. Solid and micropapillary patterns are more frequent in patients with recurrence (48 vs. 5% and 13 vs. 4%) and predominance of each one is associated with unfavourable prognosis (OS 64.1%, DFS 56.3% and OS 28.1%, DFS 28.1%, respectively). Above 25%, a growing proportion of solid or micropapillary pattern is not associated with worsening prognosis. In contrast, tumours having micropapillary pattern as secondly predominant form a different intermediate group (OS 51.1%, DFS 57.8%). Our study was based on measured area of each growth pattern on all available slides digitalized. This is the most precise way of determining the size of each component from the material available. We propose using predominant and secondly predominant patterns for prognostic purposes, particularly in tumours having solid or micropapillary patterns.

Similar content being viewed by others
References
Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG (2015) WHO classification of tumours of the lung, pleura, thymus and heart, 4th edn. International Agency for Research on Cancer, Lyon
Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, Chirieac LR, Dacic S, Duhig E, Flieder DB, Geisinger K, Hirsch FR, Ishikawa Y, Kerr KM, Noguchi M, Pelosi G, Powell CA, Tsao MS, Wistuba I, Panel WHO (2015) The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 10:1243–1260. https://doi.org/10.1097/JTO.0000000000000630
Yoshizawa A, Sumiyoshi S, Sonobe M, Kobayashi M, Fujimoto M, Kawakami F, Tsuruyama T, Travis WD, Date H, Haga H (2013) Validation of the IASLC/ATS/ERS lung adenocarcinoma classification for prognosis and association with EGFR and KRAS gene mutations: analysis of 440 Japanese patients. J Thorac Oncol 8:52–61. https://doi.org/10.1097/JTO.0b013e3182769aa8
Ujiie H, Kadota K, Chaft JE, Buitrago D, Sima CS, Lee MC, Huang J, Travis WD, Rizk NP, Rudin CM, Jones DR, Adusumilli PS (2015) Solid predominant histologic subtype in resected stage I lung adenocarcinoma is an independent predictor of early, extrathoracic, multisite recurrence and of poor postrecurrence survival. J Clin Oncol 33:2877–2884. https://doi.org/10.1200/JCO.2015.60.9818
Nitadori J, Bograd AJ, Kadota K, Sima CS, Rizk NP, Morales EA, Rusch VW, Travis WD, Adusumilli PS (2013) Impact of micropapillary histologic subtype in selecting limited resection vs lobectomy for lung adenocarcinoma of 2 cm or smaller. J Natl Cancer Inst 105:1212–1220. https://doi.org/10.1093/jnci/djt166
Lee MC, Buitrago DH, Kadota K, Jones DR, Adusumilli PS (2014) Recent advances and clinical implications of the micropapillary histological subtype in lung adenocarcinomas. Lung Cancer Manag 3:245–253
Zombori T, Furák J, Nyári T, Cserni G, Tiszlavicz L (2018) Evaluation of grading systems in stage I lung adenocarcinomas: a retrospective cohort study. J Clin Pathol 71:135–140. https://doi.org/10.1136/jclinpath-2016-204302
Mäkinen JM, Laitakari K, Johnson S, Mäkitaro R, Bloigu R, Lappi-Blanco E, Kaarteenaho R (2015) Nonpredominant lepidic pattern correlates with better outcome in invasive lung adenocarcinoma. Lung Cancer 90:568–574. https://doi.org/10.1016/j.lungcan.2015.10.014
Cai YR, Dong YJ, Wu HB, Liu ZC, Zhou LJ, Su D, Chen XJ, Zhang L, Zhao YL (2016) Micropapillary: a component more likely to harbour heterogeneous EGFR mutations in lung adenocarcinomas. Sci Rep 6(23755). https://doi.org/10.1038/srep23755
Kamiya K, Hayashi Y, Douguchi J, Hashiguchi A, Yamada T, Izumi Y, Watanabe M, Kawamura M, Horinouchi H, Shimada N, Kobayashi K, Sakamoto M (2008) Histopathological features and prognostic significance of the micropapillary pattern in lung adenocarcinoma. Mod Pathol 21:992–1001. https://doi.org/10.1038/modpathol.2008.79
Nagano T, Kim YH, Goto K, Kubota K, Ohmatsu H, Niho S, Yoh K, Naito Y, Saijo N, Nishiwaki Y (2009) Re-challenge chemotherapy for relapsed non-small-cell lung cancer. Lung Cancer 69:315–318. https://doi.org/10.1016/j.lungcan.2009.11.016
Cha MJ, Lee HY, Lee KS, Jeong JY, Han J, Shim YM, Hwang HS (2014) Micropapillary and solid subtypes of invasive lung adenocarcinoma: clinical predictors of histopathology and outcome. J Thorac Cardiovasc Surg 147:921–928. https://doi.org/10.1016/j.jtcvs.2013.09.045
Matsuoka Y, Yurugi Y, Takagi Y, Wakahara M, Kubouchi Y, Sakabe T, Haruki T, Araki K, Taniguchi Y, Nakamura H, Umekita Y (2016) Prognostic significance of solid and micropapillary components in invasive lung adenocarcinomas measuring ≤ 3 cm. Anticancer Res 36:4923–4930
Miyoshi T, Satoh Y, Okumura S, Nakagawa K, Shirakusa T, Tsuchiya E, Ishikawa Y (2003) Early-stage lung adenocarcinomas with a micropapillary pattern, a distinct pathologic marker for a significantly poor prognosis. Am J Surg Pathol 27:101–109
Sánchez-Mora N, Presmanes MC, Monroy V, Moreno N, Lara-Martínez JM, Aladro MH, Alvarez-Fernández E (2008) Micropapillary lung adenocarcinoma: a distinctive histologic subtype with prognostic significance. Case series. Hum Pathol 39:324–330. https://doi.org/10.1016/j.humpath.2007.05.029
Yeh YC, Wu YC, Chen CY, Wang LS, Hsu WH, Chou TY (2012) Stromal invasion and micropapillary pattern in 212 consecutive surgically resected stage I lung adenocarcinomas: histopathological categories for prognosis prediction. J Clin Pathol 65:910–918
Tsubokawa N, Mimae T, Sasada S, Yoshiya T, Mimura T, Murakami S, Ito H, Miyata Y, Nakayama H, Okada M (2015) Negative prognostic influence of micropapillary pattern in stage IA lung adenocarcinoma. Eur J Cardiothorac Surg 49:293–299. https://doi.org/10.1093/ejcts/ezv058
Yanagawa N, Shiono S, Abiko M, Katahira M, Osakabe M, Ogata SY (2016) The clinical impact of solid and micropapillary patterns in resected lung adenocarcinoma. J Thorac Oncol 11:1976–1983. https://doi.org/10.1016/j.jtho.2016.06.014
Roh MS, Lee JI, Choi PJ, Hong YS (2004) Relationship between micropapillary component and micrometastasis in the regional lymph nodes of patients with stage I lung adenocarcinoma. Histopathology 45:580–586
Sumiyoshi S, Yoshizawa A, Sonobe M, Kobayashi M, Fujimoto M, Tsuruyama T, Date H, Haga H (2013) Pulmonary adenocarcinomas with micropapillary component significantly correlate with recurrence, but can be well controlled with EGFR tyrosine kinase inhibitors in the early stages. Lung Cancer 81:53–59. https://doi.org/10.1016/j.lungcan.2013.04.003
Zhao ZR, Xi SY, Li W, Situ DR, Chen KM, Yang H, Su XD, Lin YB, Long H (2015) Prognostic impact of pattern-based grading system by the new IASLC/ATS/ERS classification in Asian patients with stage I lung adenocarcinoma. Lung Cancer 90:604–609. https://doi.org/10.1016/j.lungcan.2015.10.026
Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK, Gershenwald JE, Compton CC, Hess KR, Sullivan DC, Jessup JM, Brierley JD, Gaspar LE, Schilsky RL, Balch CM, Winchester DP, Asare EA, Madera M, Gress DM, Meyer LR (2017) AJCC cancer staging manual, 8th edn. Springer, New York
Jiang W, Xi J, Xu S, Lu S, Wang Q (2015) Analysis of the effect of different pathological subtypes to prognosis in stage I pulmonary adenocarcinoma. Zhonghua Wai Ke Za Zhi 53:737–741 [abstract only]
Makimoto Y, Nabeshima K, Iwasaki H, Miyoshi T, Enatsu S, Shiraishi T, Iwasaki A, Shirakusa T, Kikuchi M (2005) Micropapillary pattern: a distinct pathological marker to subclassify tumours with a significantly poor prognosis within small peripheral lung adenocarcinoma (≤ 20 mm) with mixed bronchioloalveolar and invasive subtypes (Noguchi’s type C tumours). Histopathology 46:677–684
Koga K, Hamasaki M, Kato F, Aoki M, Hayashi H, Iwasaki A, Kataoka H, Nabeshima K (2013) Association of c-Met phosphorylation with micropapillary pattern and small cluster invasion in pT1-size lung adenocarcinoma. Lung Cancer 82:413–419. https://doi.org/10.1016/j.lungcan.2013.09.005
Zhang J, Liang Z, Gao J, Luo Y, Liu T (2011) Pulmonary adenocarcinoma with a micropapillary pattern: a clinicopathological, immunophenotypic and molecular analysis. Histopathology 59:1204–1214. https://doi.org/10.1111/j.1365-2559.2011.04050.x
Pelosi G, Pellegrinelli A, Fabbri A, Tamborini E, Perrone F, Settanni G, Busico A, Picciani B, Testi MA, Militti L, Maisonneuve P, Valeri B, Sonzogni A, Proto C, Garassino M, De Braud F, Pastorino U (2016) Deciphering intra-tumour heterogeneity of lung adenocarcinoma confirms that dominant, branching, and private gene mutations occur within individual tumour nodules. Virchows Arch 468:651–662. https://doi.org/10.1007/s00428-016-1931-z
Yatabe Y, Kosaka T, Takahashi T, Mitsudomi T (2005) EGFR mutation is specific for terminal respiratory unit type adenocarcinoma. Am J Surg Pathol 29:633–639
Girard N, Sima CS, Jackman DM, Sequist LV, Chen H, Yang JC, Ji H, Waltman B, Rosell R, Taron M, Zakowski MF, Ladanyi M, Riely G, Pao W (2012) Nomogram to predict the presence of EGFR activating mutation in lung adenocarcinoma. Eur Respir J 39:366–372. https://doi.org/10.1183/09031936.00010111
Yoshida A, Tsuta K, Nakamura H, Kohno T, Takahashi F, Asamura H, Sekine I, Fukayama M, Shibata T, Furuta K, Tsuda H (2011) Comprehensive histologic analysis of ALK-rearranged lung carcinomas. Am J Surg Pathol 35:1226–1234. https://doi.org/10.1097/PAS.0b013e3182233e06
Sumiyoshi S, Yoshizawa A, Sonobe M, Kobayashi M, Sato M, Fujimoto M, Tsuruyama T, Date H, Haga H (2014) Non-terminal respiratory unit type lung adenocarcinoma has three distinct subtypes and is associated with poor prognosis. Lung Cancer 84:281–288. https://doi.org/10.1016/j.lungcan.2014.03.013
Warth A, Stenzinge r A, von BrĂĽnneck AC, Goeppert B, Cortis J, Petersen I, Hoffmann H, Schnabel PA, Weichert W (2012) Interobserver variability in the application of the novel IASLC/ATS/ERS classification for pulmonary adenocarcinomas. Eur Respir J 40:1221–1227. https://doi.org/10.1183/09031936.00219211
Thunnissen E, Beasley MB, Borczuk AC, Brambilla E, Chirieac LR, Dacic S, Flieder D, Gazdar A, Geisinger K, Hasleton P, Ishikawa Y, Kerr KM, Lantejoul S, Matsuno Y, Minami Y, Moreira AL, Motoi N, Nicholson AG, Noguchi M, Nonaka D, Pelosi G, Petersen I, Rekhtman N, Roggli V, Travis WD, Tsao MS, Wistuba I, Xu H, Yatabe Y, Zakowski M, Witte B, Kuik DJ (2012) Reproducibility of histopathological subtypes and invasion in pulmonary adenocarcinoma. An international interobserver study. Mod Pathol 25:1574–1583. https://doi.org/10.1038/modpathol.2012.106
Zhang H, Lu C, Lu Y, Yu B, Lv F, Zhu Z (2016) The predictive and prognostic values of factors associated with visceral pleural involvement in resected lung adenocarcinomas. Onco Targets Ther 9:2337–2348. https://doi.org/10.2147/OTT.S100965
Campos-Parra AD, Avilés A, Contreras-Reyes S, Rojas-Marín CE, Sánchez-Reyes R, Borbolla-Escoboza RJ, Arrieta O (2014) Relevance of the novel IASLC/ATS/ERS classification of lung adenocarcinoma in advanced disease. Eur Respir J 43:1439–1447. https://doi.org/10.1183/09031936.00138813
Acknowledgments
We gratefully acknowledge the assistance of Dániel Urbán, Réka Némedi, Zsófia Tornyossy and Noémi Tóth in collecting clinical data of the patients and in the digitalization of slides.
Funding
This study was partially funded by the National Research, Development and Innovation Office grant GINOP-2.3.2-15-2016-00020.
Author information
Authors and Affiliations
Contributions
All authors of the manuscript made substantial contributions to the conception or design of the work; the acquisition, analysis or interpretation of data for the work; drafting the work and/or revising it critically for important intellectual content; final approval of the version submitted for publication; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
More specifically, author contribution is listed as follows:
TZ: Concept, case selection, application and refinement of the methods, evaluation of all cases, analysis of data, preparation of the manuscript, finalisation and approval of the manuscript
TN: Statistical analysis, preparation of the manuscript, finalisation and approval of the manuscript
LT: Case selection, application and refinement of the methods, evaluation of histology slides, finalisation and approval of the manuscript
GC: Development of the methods, supervision, preparation of the manuscript, finalisation and approval of the manuscript
RP: Data collection, finalisation and approval of the manuscript
EC: Data collection, finalisation and approval of the manuscript
TG: Resources, finalisation and approval of the manuscript
AO: Resources, finalisation and approval of the manuscript
BP: Resources, finalisation and approval of the manuscript
JF: Concept, case selection, finalisation and approval of the manuscript
Corresponding author
Ethics declarations
The authors have consulted the journal policy regarding compliance with ethical standards and state that accepted principles of ethical and professional conduct have been followed. The authors include information regarding sources of funding (previous section) and potential conflicts of interest (financial or non-financial) (next section). This retrospective study was approved by the institutional ethical committee of the Albert Szent-Györgyi Clinical Centre of the University of Szeged. The study did not include animals; therefore, issues relating to animal welfare do not apply.
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(DOCX 12.1 kb)
ESM 2
(DOCX 14.6 kb)
ESM 3
(DOCX 11.5 kb)
ESM 4
(DOCX 11.9 kb)
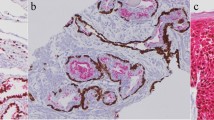
Supplementary Fig. 1
The distinct growth patterns of invasive lung adenocarcinoma: A: lepidic, B: acinar, C: cribriform, D: papillary, E: solid, and F: micropapillary (GIF 825 kb)
High Resolution Image
(TIFF 12815 kb)
Rights and permissions
About this article
Cite this article
Zombori, T., Nyári, T., Tiszlavicz, L. et al. The more the micropapillary pattern in stage I lung adenocarcinoma, the worse the prognosis—a retrospective study on digitalized slides. Virchows Arch 472, 949–958 (2018). https://doi.org/10.1007/s00428-018-2337-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-018-2337-x