Abstract
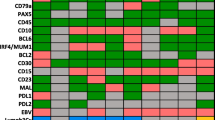
Mucosa-associated lymphoid tissue (MALT) lymphoma mainly consists of three types of tumor B cells, small (centrocyte-like), scattered large transformed, and intraepithelial. However, it is difficult to differentiate tumor B cells from reactive B cells at the cellular level. We examined five cases of API2-MALT1 fusion-positive MALT lymphoma of the lung. A single paraffin section for each case was subjected to sequential retrieval of whole-slide imaging (WSI) data of hematoxylin and eosin (HE) staining, immunofluorescence staining for CD79a, and fluorescence in situ hybridization (FISH) for the MALT1 split. We counted the number of MALT1 split-positive or MALT1 split-negative cells among CD79a-positive cells. The MALT1 split was detected in 59, 46, and 76 % of small, large, and intraepithelial B cells, respectively. A review of the HE-WSI data showed that cytomorphological distinction between the MALT1 split-positive and MALT1 split-negative B cells was virtually impossible. None of CD79a-negative lymphoid cells, epithelial cells, and microvascular endothelial cells was positive for MALT1 splits. As API2-MALT1 fusion is an early and critical event in the lymphomatogenesis, our findings are best interpreted as that a considerable number of B cells, either small, large, or intraepithelial, are reactive cells and that it is difficult to distinguish cytomorphologically between tumor B cells and reactive B cells. These findings suggest that the tumor architecture may be the central factor for making a correct histopathological diagnosis of MALT lymphoma. The sequential WSI of HE staining, immunofluorescence staining, and FISH as described here is a useful tool for pathological analysis at the cellular level.





Similar content being viewed by others
References
Adam P, Czapiewski P, Colak S, et al. (2014) Prevalence of Achromobacter xylosoxidans in pulmonary mucosa-associated lymphoid tissue lymphoma in different regions of Europe. Br J Haematol 164:804–810
Bob R, Falini B, Marafioti T, Paterson JC, Pileri S, Stein H (2013) Nodal reactive and neoplastic proliferation of monocytoid and marginal zone B cells: an immunoarchitectural and molecular study highlighting the relevance of IRTA1 and T-bet as positive markers. Histopathology 63:482–498
Feldman AL, Arber DA, Pittaluga S, et al. (2008) Clonally related follicular lymphomas and histiocytic/dendritic cell sarcomas: evidence for transdifferentiation of the follicular lymphoma clone. Blood 111:5433–5439
Gerdes MJ, Sevinsky CJ, Sood A, et al. (2013) Highly multiplexed single-cell analysis of formalin-fixed, paraffin-embedded cancer tissue. Proc Natl Acad Sci U S A 110:11982–11987
Hollman-Hewgley D, Lazare M, et al. (2014) A single slide multiplex assay for the evaluation of classical Hodgkin lymphoma. Am J Surg Pathol 38:1193–1202
Inagaki H (2007) Mucosa-associated lymphoid tissue lymphoma: molecular pathogenesis and clinicopathological significance. Pathol Int 57:474–484
Inagaki H, Okabe M, Seto M, Nakamura S, Ueda R, Eimoto T (2001) API2-MALT1 fusion transcripts involved in mucosa-associated lymphoid tissue lymphoma: multiplex RT-PCR detection using formalin-fixed paraffin-embedded specimens. Am J Pathol 158:699–706
Inagaki H, Li C, Okabe M, et al. (2005) Detection of API2-MALT1 fusion transcripts in cytologic specimens of patients with pulmonary mucosa-associated lymphoid tissue lymphoma. Int J Hematol 82:59–62
Isaacson PG, Spencer J (1987) Malignant lymphoma of mucosa-associated lymphoid tissue. Histopathology 11:445–462
Isaacson PG, Chott A, Nakamura S, et al. (2008) World Health Organization classification of tumours. Pathology and genetics: tumours of haemopoietic and lymphoid tissues, 4th edn. In: Swerdlow SH, Campo E, Harris NL, et al. (eds) Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma). IARC Press, Lyon, pp. 214–217
Ishibashi K, Ito Y, Masaki A, et al. (2015) Warthin-like mucoepidermoid carcinoma: a combined study of fluorescence in situ hybridization and whole-slide imaging. Am J Surg Pathol 39:1479–1487
Korac P, Jones M, Dominis M, et al. (2005) Application of the FICTION technique for the simultaneous detection of immunophenotype and chromosomal abnormalities in routinely fixed, paraffin wax embedded bone marrow trephines. J Clin Pathol 58:1336–1338
Kuper-Hommel MJ, van Krieken JH (2012) Molecular pathogenesis and histologic and clinical features of extranodal marginal zone lymphomas of mucosa-associated lymphoid tissue type. Leuk Lymphoma 53:1032–1045
Laurent C, Guérin M, Frenois FX, et al. (2013) Whole-slide imaging is a robust alternative to traditional fluorescent microscopy for fluorescence in situ hybridization imaging using break-apart DNA probes. Hum Pathol 44:1544–1555
Nie Z, MQ D, McAllister-Lucas LM, et al. (2015) Conversion of the LIMA1 tumour suppressor into an oncogenic LMO-like protein by API2-MALT1 in MALT lymphoma. Nat Commun 6:–5908
O’Malley DP, George TI, Orazi A, Abbondanzo SL (2009) General reactive conditions in lymph node and spleen. Benign and reactive conditions of lymph node and spleen AFIP atlas of nontumor pathology ARP press, Washington DC:97–142
Okabe M, Inagaki H, Ohshima K, et al. (2003) API2-MALT1 fusion defines a distinctive clinicopathologic subtype in pulmonary extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue. Am J Pathol 162:1113–1122
Rosebeck S, Madden L, Jin X, et al. (2011) Cleavage of NIK by the API2-MALT1 fusion oncoprotein leads to noncanonical NF-kappaB activation. Science 331:468–472
Streubel B, Simonitsch-Klupp I, Müllauer L, et al. (2004a) Variable frequencies of MALT lymphoma-associated genetic aberrations in MALT lymphomas of different sites. Leukemia 18:1722–1726
Streubel B, Chott A, Huber D, et al. (2004b) Lymphoma-specific genetic aberrations in microvascular endothelial cells in B-cell lymphomas. N Engl J Med 351:250–259
Vicente-Dueñas C, Fontán L, Gonzalez-Herrero I, et al. (2012) Expression of MALT1 oncogene in hematopoietic stem/progenitor cells recapitulates the pathogenesis of human lymphoma in mice. Proc Natl Acad Sci U S A 109:10534–10539
Wotherspoon AC, Ortiz-Hidalgo C, Falzon MR, et al. (1991) Helicobacter pylori-associated gastritis and primary B-cell gastric lymphoma. Lancet 338:1175–1176
Ye H, Liu H, Attygalle A, et al. (2003) Variable frequencies of t (11;18) (q21 q21) in MALT lymphomas of different sites: significant association with CagA strains of H. pylori in gastric MALT lymphoma. Blood 102:1012–1018
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All research protocols were approved by the institutional review board of Nagoya City University (#113) and conformed to the provisions of the Declaration of Helsinki.
Funding
This study was supported in part by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology (MEXT) of Japan (15K08351 to H. Inagaki).
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Fig. S1
Detection of MALT1 splits in CD79a-negative lymphoid cells (A-C), epithelial cells (D and E), and microvascular endothelial cells (F and G). None of these cells shows MALT1 split. Asterisks indicate lymphoid cells negative for CD79a (B). White arrows indicate fused (unaltered) MALT1 signals (C, E, and G). Cilia of the epithelial cells are indicated by an orange arrow (D). HE stain (A, D, and F), immunostain for CD79a (B), and FISH for MALT1 split (C, E, and G). (PPT 3262 kb)
Rights and permissions
About this article
Cite this article
Fujii, K., Ishibashi, Ki., Kato, J. et al. Cellular-level characterization of B cells infiltrating pulmonary MALT lymphoma tissues. Virchows Arch 469, 575–580 (2016). https://doi.org/10.1007/s00428-016-2012-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-016-2012-z