Abstract
Muscle changes of critical illness are attributed to systemic inflammatory responses and disuse atrophy. GTS-21 (3-(2,4-dimethoxy-benzylidene)anabaseine), also known as DMBX-A) is a synthetic derivative of the natural product anabaseine that acts as an agonist at α7-acetylcholine receptors (α7nAChRs). Hypothesis tested was that modulation of inflammation by agonist GTS-21 (10 mg/kg b.i.d. intraperitoneally) will attenuate body weight (BW) and muscle changes. Systemic sham inflammation was produced in 125 rats by Cornyebacterium parvum (C.p.) or saline injection on days 0/4/8. Seventy-four rats had one immobilized-limb producing disuse atrophy. GTS-21 effects on BW, tibialis muscle mass (TMM), and function were assessed on day 12. Systemically, methemoglobin levels increased 26-fold with C.p. (p < 0.001) and decreased significantly (p < 0.033) with GTS-21. Control BW increased (+ 30 ± 9 g, mean ± SD) at day 12, but decreased with C.p. and superimposed disuse (p = 0.005). GTS-21 attenuated BW loss in C.p. (p = 0.005). Compared to controls, TMM decreased with C.p. (0.43 ± 0.06 g to 0.26 ± 0.03 g) and with superimposed disuse (0.18 ± 0.04 g); GTS-21 ameliorated TMM loss to 0.32 ± 0.04 (no disuse, p = 0.028) and to 0.22 ± 0.03 (with disuse, p = 0.004). Tetanic tensions decreased with C.p. or disuse and GTS-21 attenuated tension decrease in animals with disuse (p = 0.006) and in animals with C.p. and disuse (p = 0.029). C.p.-induced 11-fold increased muscle α7nAChR expression was decreased by > 60% with GTS-21 treatment. In conclusion, GTS-21 modulates systemic inflammation, evidenced by both decreased methemoglobin levels and decrease of α7nAChR expression, and mitigates inflammation-mediated loss of BW, TMM, fiber size, and function.
Similar content being viewed by others
Introduction
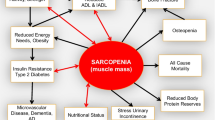
Critical illness, particularly when associated with immobilization in bed or decreased mobility, leads to muscle wasting and muscle weakness (MW) [9, 12, 13, 42, 57] occurring in 32–100% of hospital patients [37, 39, 58]. This pathological entity has varying names including critical illness polyneuropathy, critical illness myopathy, and/or critical illness polyneuromyopathy [58, 64]. The short-term complications of MW include dependence on respirators with a higher risk for ventilator-associated pneumonia, deep vein thrombosis, with pulmonary embolism and/or decubitus ulcers. The inflammation-associated MW can be further compounded by disuse atrophy because of immobilization in bed, application of bandages and plaster casts, and/or decreased motor activity due to illness [22, 23]. The functional neuromuscular disability after critical illness can persist even at 5 years after the initial insult [20, 21, 53]. Current therapeutic maneuvers used for prevention of MW, including better nutrition, physical therapy, and anabolic drug therapy (oxandralone, insulin, metformin, etc.), do not completely reverse the muscle changes and disability during and after their hospitalization [4, 49]. Despite all or some of these interventions, MW continues to occur in critical illness. Early mobilization within 72 h seems to be the only effective intervention so far [55, 56]. Early mobilization, however, is not possible in all critically ill patients because of factors related to the disease itself.
A concomitant pathologic feature of critical illness is the presence of systemic inflammatory responses with cytokine release leading to increased protein breakdown and decreased protein synthesis [9, 38, 65, 66]. A pathognomic biochemical feature in MW conditions is the presence of a denervation-like state, evidenced by the upregulation of the fetal (a.k.a. immature) nicotinic acetylcholine receptors (nAChRs) isoform on the muscle membrane [45].
Most recently, the de novo expression of another isoform, the α7-acetylcholine receptors (α7nAChR) (consisting of five homomeric α7 subunits only) has been described in muscle wasting conditions [32, 41, 43, 60]. The expression of α7nAChRs in normal mature muscle is minimal. In contrast to muscle expression of α7nAChRs only in pathologic states, the α7nAChRs are constitutively expressed in macrophages and other circulating leucocytes [25, 40, 44, 62]. During inflammation, however, these α7nAChRs are further upregulated in vitro in macrophages [30] and in vivo in burned patients [51]. Several studies have documented anti-inflammatory properties when α7nAChRs are stimulated by agonists. Exogenous nicotine and endogenous acetylcholine or choline have been the prototypical α7nAChRs agonists, but all of them have non-specific effects on other receptors too. The systemic administration of GTS-21, a highly selective α7nAChR agonist [28, 61], in vivo decreased cytokine release and/or inflammation [26] and resulted in improved function in inflamed pathologic organs (e.g., lungs [35]) or survival [30, 31]. GTS-21 (which is the laboratory name of 3-(2,4-dimethoxy-benzylidene)anabaseine) also known as DMBX-A is a synthetic derivative of the natural toxin anabaseine produced by nemertines [27]. It binds to both the α4β2 and α7 subtypes, but activates only the α7 to any significant extent [2, 48]. It has been clinically tested to decrease systemic inflammatory responses in a phase II clinical trial [34], as well as in schizophrenic, Alzheimer’s disease and attention-deficit hyperactivity disorder subjects [11, 29, 33, 50]. Disuse atrophy per se leads to inflammation and de novo expression of α7nAChRs in the wasting muscles, despite absence of systemic inflammation [32, 41]. The ability of the α7nAChR agonist GTS-21 to mitigate bacteria-induced systemic inflammatory responses and the skeletal muscle changes associated with it have not yet been tested.
We have previously described a model of systemic inflammation or disuse alone, and their combination (double-hit model) in rats mimicking critical illness induced muscle disuse atrophy [9, 12, 57]. In this model, systemic inflammation was produced by injection of Corynebacterium parvum (C.p.) [1, 8, 10, 46] and disuse of one leg was produced by pinning [9, 12, 57]. The advantages of this model are (1) systemic inflammation can be maintained over a longer time period [1, 63] without inducing sepsis with a much higher mortality like other models (e.g., endotoxemia or caecal ligation) [3, 52] and (2) the nerve-muscle composition stays intact in comparison to denervation models mimicking an intensive care patient much better. The inflammation produced by C.p. was evidenced by increased methemoglobin (MetHb) levels (a surrogate for increased nitric oxide-levels), as well as increased α1-acid glycoprotein levels (an acute phase reactant protein) and decreased platelet and erythrocyte counts [9, 63]. Thus, there is a priori evidence that systemic inflammation and/or muscle wasting (disuse, sepsis and denervation) upregulate α7nAChRs both in muscle and leucocytes [30, 32, 41, 59]. Based on this evidence, the hypothesis tested in this study was that these upregulated α7nAChRs could be used to decrease systemic and local muscle inflammation and therefore reverse the systemic inflammation- and/or disuse-induced muscle changes in the previously described rat model [9, 57].
Materials and methods
Animal model and study design
After approval by the institutional review board (Subcommittee on Research Animal Care, Committee on Research, Massachusetts General Hospital, #2010N000168), 125 male Sprague-Dawley rats (Taconic Farms Inc., Germantown, NY, USA, 151–175 g) were acclimated to the standard conditions of our animal facility with free access to chow and water for ≥7 days. The previously described model, consisting of four groups, was used [9]: (1) sham-immobilization with saline (sham-inflammation), (2) immobilization with saline, (3) sham-immobilization with C.p. (inflammation), and (4) immobilization with C.p.. Systemic inflammation was induced by intravenous injection of 56 mg/kg whole cell preparation of heat-inactivated C.p. (Roche, Penzberg, Germany) via dorsalis penis vein during anesthesia at days 0, 4, and 8 as described previously [1, 8,9,10, 46, 57]. We use methemoglobin measurements as surrogate marker for the severity of inflammation, since methemoglobin correlates with the upregulated nitric oxide concentration and acute phase proteins [1, 9, 10, 57, 63]. Substitute animals (n = 17) had to be added to the inflammation groups because of higher mortality (Fig. 1). Injection of 0.9% normal saline solution (sham-inflammation) served as control.
To induce disuse atrophy of one hind limb was immobilized for a period of 12 days by pinning of knee and ankle joints at 90° using 1.0-mm Kirschner wires (immobilization). After a skin incision at each joint, the calcaneus, tibia, and femur were drilled and the joints were pinned with the knee in flexion and ankle in dorsiflexion [9, 12, 57]. Sham-immobilization was achieved by insertion of the Kirschner wires into the bone, and the wire removed immediately thereafter (sham-immobilization). The contralateral leg of the immobilized and sham-immobilized animals on which no surgery was performed in saline groups were used to provide naïve control values.
The four groups were further divided into two subgroups, depending on the pharmacological therapy received: (A) saline as placebo or (B) 10 mg/kg GTS-21, administered i.p. twice a day. GTS-21 was provided by William Kem (University of Florida, Gainesville, FL., chemical purity > 99%). GTS-21, due to its weak light sensitivity, was prepared with sterile saline 0.9% in a dark room using only yellow light. The preparation was adjusted to a pH of 7.35, stored in syringes in the darkroom, transported in a light protected container to the animal room, and injected with lights switched off using a small yellow lamp as illumination.
The combination of perturbations described above resulted in the eight groups (Fig. 1). For the immobilization procedure and injections of C.p./saline on days 0, 4, and 8, the animals were anesthetized with isoflurane in a Plexiglas chamber. After induction of anesthesia, the head of the animal was placed in a chamber with a continuous flow of isoflurane while the animal was breathing spontaneously. At day 12 after the perturbations (induction of inflammation, immobilization or sham procedures), the Kirschner wires were removed (from the immobilized animals) and neuromuscular function studies performed in all animals. For the neuromuscular functional studies at day 12, anesthesia was induced with pentobarbital i.p., and maintained with empirical doses of 10–20 mg/kg given every 10–20 min based on withdrawal response to toe clamping. After loss of consciousness, the rats were tracheotomized and mechanically ventilated with air. The jugular vein was cannulated as access for administration of fluids. A cannula in the carotid artery was used to measure arterial blood pressure and for blood for gas analyses.
Neuromuscular function test
Before the neuromuscular experiments, ventilation was adjusted to maintain a PaCO2 between 35 and 45 mmHg, PaO2 of > 90 mmHg, and pH between 7.36 and 7.44. Whenever necessary, base deficit was corrected with 1 mM sodium bicarbonate to values between − 3 and 3 mM. Blood glucose levels were controlled between 80 and 130 mg/dl. Heart rate and mean arterial pressure were continuously monitored to ensure stable hemodynamic conditions throughout the experiment. Rectal temperature was controlled between 36.8 and 37.2 °C by adjusting the heat generated from the experiment table and with a heat lamp, if needed. Nerve-induced neuromuscular function was assessed by evoked mechanomyography [9, 12, 57]. The functional measures included single twitch tension and peak tetanic tension at 50 Hz stimulation. Following these functional studies, the animals were euthanized by exsanguination after high dose of pentobarbital (200 mg/kg).
Ex vivo analyses
α7nAChR expression
The cranial tibialis muscle on each side was dissected out, weighed, snap frozen in liquid nitrogen, and stored airtight at − 80 °C for western blot analysis. For western blot of α7nAChRs expression, each tibialis muscle was homogenized in homogenization buffer (Sigma-Aldrich Chemie GmbH, Munich, Germany) containing protease inhibitor (Sigma) as described previously [41], using a tissue lyser (TissueLyser LT, QIAGEN, Hilden, Germany). The samples were centrifuged, and aliquots of the supernatant containing equal amounts of protein (by Bradford Assay) were subjected to TGX Stain-Free™ Gels (Bio-Rad Laboratories GmbH, Munich, Germany), and then immunoblotting was performed [30]. Equal amounts of protein (40 μg) per lane were subjected to NuPAGE and then blotted onto PVDF membrane (Bio-Rad Laboratories GmbH, Munich, Germany). The membrane was blocked by Roti®-Block (Carl Roth GmbH + Co. KG, Karlsruhe, Germany). Anti-α7AChR (dilution 1:2.500, ab24644, Abcam, Cambridge, UK) was used as primary antibody. The membranes were incubated in horseradish peroxidase-conjugated goat anti-rat secondary antibody (NA935V, GE Healthcare, Amersham, UK) for 60 min (dilution 1:10.000). The specific proteins were detected by Bio-Rad Molecular Imager® ChemiDoc™ XRS+ (Bio-Rad Laboratories GmbH, Munich, Germany) and analyzed with ImageLab (Bio-Rad Laboratories GmbH, Munich, Germany) using total protein normalization using stain-free technology [14,15,16, 54].
Immunohistochemistry
After dissection of TA, muscles were snap-frozen in melting isopentane to prevent freeze artifacts. Fixed with OCT (Surgipath FSC 22 Clear, Leica, Wetzlar, Germany) muscles were cut using a cryotome (Kryostat HM 560-V, Thermo Scientific GmbH, Schwerte, Germany) in 10 μm and mounted on glass slides (Superfrost Plus, Thermo Scientific GmbH, Schwerte Germany). Section were stored at − 80 °C until staining. Before staining, sections were fixed for 5 min in acetone-isopropanol 1:1 solution − 20°. Prior to staining, unspecific antibody binding was blocked by 10% bovine serum albumin in phosphate buffered saline/Tween20 (PBS/T) with pH 7.4 for 60 min. Subsequently, specific epitopes were detected by using the following primary antibodies: myosin heavy chain slow (M8421, Sigma, Germany) and myosin heavy chain fast (M4276, Sigma, Germany). Therefore, the antibodies were diluted 1:1000 in PBS/T buffer and incubated over night at 4 °C. Goat-anti-mouse antibody (1070-05, SouthernBiotech, Birmingham, USA) was used as secondary antibody diluted in PBS/T 1:5000 for 1 h at room temperature. This was followed by DAB-staining with DAKO Liquid DAB+ Substrate chromogen System (K3467, DAKO, Glostrup, Denmark) with DAB+ Chromogen (3,3′daiminobenzidine in chromogen solution) using 30 droplets DAB in 10-ml substrate buffer, staining for 5 min. Two minutes with Mayer’s hematoxylin (Roth, Germany) was used for counterstaining thereafter. Finally, sections were rinsed in aqua dest., dehydrated in ascending ethanol dilutions (70, 96, and 100% for 5 min each), dipped in xylol and covered with Dako Mounting Medium (Dako, CA, USA).
Morphometric measurement
All histological analyses were executed blinded as well as in a random order. Additionally, measurements were done twice by two independent researchers. Histological images were acquired using Axio Imager microscope (Zeiss, GER) and calibrated AxioVision SE64 Rel. 4.9 software tool (Zeiss, Germany). To quantify the total mean of muscle fiber cross section area (μm2), 20 fibers of three different sections were analyzed in the H&E as well as myosin heavy chain (slow/fast) stains. Mean fiber areas were quantified manually by using AxioVision measurement tool and computed by Excel 2016 (Microsoft, USA).
Statistical analyses
Three hypotheses were tested for the variables that were recorded in each group: (1) effect of therapy, (2) effect of inflammation, and (3) effect of mobility. For this purpose, data were subjected to univariate analyses of variance with the factors (1) therapy (placebo vs. GTS-21), (2) inflammation (saline vs. C.p.), and (3) mobility (sham-immobilization vs. immobilization), as well as all possible interaction terms. If the respective main effect or interaction term proved to be significant, post hoc analyses were hierarchically performed. The probability error was set at 0.05. Due to the positively skewed distribution, the arbitrary values of α7nAChRs expression were transformed into logarithmic scale. Statistical analyses were performed using IBM SPSS Statistics 25.0 (SPSS, Chicago, IL), figures were created with STATA 14 (Stata Corp LP, College Station, TX).
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Results
The different perturbations in the four groups were performed in rats totaling 125. However, only 92 were used in the final analyses because of mortality before and on day 12 during neuromuscular function tests (Fig. 1).
Systemic effects on MetHb levels and body weight and response to GTS-21
The MetHb levels as a fraction of total hemoglobin (percent) were almost undetectable in all saline groups (0.3 ± 0.1%) regardless of presence or absence of immobilization. Consequently, GTS-21 had no influence on MetHb levels in saline groups. MetHb increased 26-fold on average in C.p. animals (p < 0.001) with a 32-fold increase when compared to placebo subgroups. GTS-21 significantly decreased the elevated MetHb levels seen in C.p. treated with saline to 19-fold (p = 0.049, Fig. 2). Immobilization did not affect MetHb levels.
Blood methemoglobin (MetHb) levels in rats with each perturbation on day 12 [fold change compared to saline groups]. MetHb fraction of total hemoglobin was significantly increased by C.p. (26-fold average increase, p < 0.001) and significantly reduced in all GTS-21 groups (p = 0.033). Post hoc analysis revealed a 40% decrease in C.p.-injected animals by therapy (from 32-fold with placebo to 19-fold with GTS-21, filled triangles, p = 0.049). Immobilization did not influence MetHb levels significantly. Sham = Sham-immobilization, Immob = immobilization/superimposed disuse, C.p. = systemic inflammation with Corynebacterium parvum, Saline = sham-inflammation with saline, GTS =GTS-21 = DMBX-A = 3-[(3E)-3-[(2,4-dimethoxyphenyl)methylidene]-5,6-dihydro-4H-pyridin-2-yl]pyridine, bid = bis in die =twice a day.
Over the 12-day period, the body weights decreased significantly with C.p. alone and with immobilization and GTS-21 mitigated these changes (Fig. 3). Rats receiving saline or GTS-21 alone without C.p. and disuse (Controls) gained body weight significantly (+30 ± 9 g) or GTS-21 (+31 ± 18 g), respectively, compared to Day 0. With C.p. alone, the body weight at day 12 significantly decreased (16 ± 20 g on average, p < 0.001) relative to body weights of saline groups. Compared to saline treatment, GTS-21 prevented the loss of body weight that occurred with inflammation (− 23 ± 17 g vs. − 9 ± 20 g, p = 0.011, Fig. 3).
Body weight changes between days 0 and 12. The change of body weight comparing days 12 vs. 0 was significantly decreased by C.p. (− 16 ± 20 g, p < 0.001). Therapy with 10 mg/kg GTS-21 b.i.d. significantly attenuated body weight loss in the C.p. groups (inflammation × therapy: p = 0.005). Post hoc analysis revealed in C.p. showed a significant improvement by GTS-21 therapy compared to placebo (filled triangles, − 9 ± 20 g vs. − 23 ± 17 g, respectively, p = 0.011). Immobilization effected body weight change in all respective groups (p < 0.001). GTS-21 had a significant effect in post hoc analysis of therapy compared to placebo in C.p. with disuse superimposed (filled circles from − 29 ± 16 g to − 14 ± 10 g, respectively, p = 0.009). Sham = sham-immobilization, Immob = immobilization/superimposed disuse, C.p. = systemic inflammation with Corynebacterium parvum, Saline = sham-inflammation with saline, GTS = GTS-21 = DMBX-A = 3-[(3E)-3-[(2,4-dimethoxyphenyl)methylidene]-5,6-dihydro-4H-pyridin-2-yl]pyridine, bid = bis in die = twice a day
C.P. and/or immobilization-induced muscle changes and response to GTS-21
Maintenance of the immobilization for 12 days (without C.p.) consistently decreased tibialis weight in placebo groups (p < 0.001, Fig. 4a) as well as twitch tension (72 ± 16 vs. 146 ± 7 N, p < 0.0001) and tetanic tension (163 ± 11 vs. 469 ± 41, p < 0.0001). Tibialis muscle mass was also significantly decreased by inflammation (p < 0.001), but even more with their combination (inflammation × immobilization: p < 0.001). Therapy with GTS-21 b.i.d. significantly ameliorated the effects in all respective groups (p = 0.003). Post-hoc analysis in animals with sham-immobilization (p = 0.044), immobilization (p = 0.019), as well as in C.p.-injected animals (p < 0.001) revealed a significant effect of GTS-21 therapy vs. placebo. GTS-21 was able to increase tibialis mass in C.p. groups without (from 0.26 ± 0.03 g to 0.32 ± 0.04 g, p = 0.028) and with disuse superimposed (from 0.18 ± 0.04 g to 0.22 ± 0.03 g, p = 0.004).
Muscle changes (mass and force) with disuse, or inflammation alone and their combination without and with GTS-21. a Tibialis muscle mass. Gray background area indicates the lower and upper limit of tolerance (i.e., mean ± 1.96 × SD of the naïve leg of saline animals). Tibialis muscle mass was significantly decreased by inflammation. (p < 0.001) or immobilization (p < 0.001), but even more with their combination (inflammation × immobilization: p < 0.001). Therapy with GTS-21 b.i.d. significantly ameliorated the effects in all respective groups (p = 0.003). Post hoc analysis in animals with sham-immobilization (empty diamonds, p = 0.044) and immobilization (filled diamonds, p = 0.019) as well as in C.p.-injected animals revealed a significant effect of GTS-21 therapy vs. placebo (filled triangles, p < 0.001). GTS-21 was able to increase tibialis mass in C.p. groups without (empty circles, from 0.26 ± 0.03 g to 0.32 ± 0.04 g, p = 0.028) and with disuse superimposed (filled circles, from 0.18 ± 0.04 g to 0.22 ± 0.03 g, p = 0.004). b Maximum tetanic tension. Colored area in broad blue indicates the lower and upper limit of tolerance (i.e., mean ± 1.96 × SD of the naïve leg of saline animals). Tetanic maximum tensions were significantly decreased by inflammation (p < 0.001) or immobilization (p < 0.001), but even more with their combination (inflammation × immobilization: p < 0.001). Therapy with GTS-21 significantly ameliorated the effects in all respective groups (p = 0.035). Post hoc analysis in animals with immobilization revealed a significant effect of GTS-21 therapy vs. placebo (filled diamonds, p = 0.006). Post hoc analysis in C.p.-injected animals with disuse superimposed revealed a significant effect of GTS-21 therapy vs. placebo (filled circles, 1.35 ± 0.51 N vs. 1.81 ± 0.42 N, p = 0.029). Sham = sham-immobilization, Immob = immobilization/superimposed disuse, C.p. = systemic inflammation with Corynebacterium parvum, Saline = sham-inflammation with saline, GTS = GTS-21 = DMBX-A = 3-[(3E)-3-[(2,4-dimethoxyphenyl)methylidene]-5,6-dihydro-4H-pyridin-2-yl]pyridine, bid = bis in die = twice a day
Although all three main factors tested (therapy, inflammation, mobility) were significant in single twitch, post hoc analysis showed no significant therapy effect (data not shown). Maximum tetanic tensions were significantly decreased by inflammation (p < 0.001) or immobilization (p < 0.001), and even more by their combination (inflammation × immobilization: p < 0.001). Post hoc analysis in animals with immobilization revealed a significant effect of GTS-21 therapy vs. placebo (p = 0.006). Furthermore, GTS-21 significantly ameliorated the negative effects on peak tetanic contraction in all respective groups (p = 0.035) and in the inflammation with immobilization group (1.35 ± 0.51 N vs. 1.81 ± 0.42 N, p = 0.029, Fig. 4b).
H&E staining of muscle tissue demonstrated a significant effect for all factors (inflammation p < 0.001, mobility p < 0.001, and therapy p = 0.010) including the interaction of inflammation and mobility (p = 0.001) on fiber size (Fig. 5a). The muscle fiber type area was influenced significantly by all three factors as well: slow myosin fiber area as well as fast myosin fiber area were significantly decreased by inflammation (p = 0.012, p < 0.001); mobility (p = 0.003, p < 0.001); and therapy (p = 0.004, n.s. for main factor, but mobility × therapy (p = 0.003) and inflammation × therapy (p = 0.029)), respectively. Post hoc analysis in slow muscle fiber area showed a significant increase by GTS-21 vs. placebo in groups with saline (1184 ± 50 μm2 vs. 1013 ± 61 μm2, p = 0.031) and inflammation (1037 ± 46 μm2 vs. 879 ± 56 μm2, p = 0.041, Fig. 5b). In fast fiber area, post-hoc analysis in of GTS-21 therapy vs. placebo revealed a significant increase of fiber size in immobilized animals (1159 ± 235 μm2 vs. 993 ± 294 μm2, p = 0.003) and in C.p. animals with disuse superimposed (1064 ± 58 μm2 vs. 718 ± 89 μm2, p = 0.005, Fig. 5c).
Immunohistochemistry of tibialis with disuse or inflammation alone and their combination without and with GTS-21. Values presented as mean ± SE. a H&E staining. H&E area of muscle fiber was significantly decreased by inflammation. (p < 0.001) or immobilization (p < 0.001), but even more with their combination (inflammation × immobilization: p = 0.001). Therapy with GTS-21 b.i.d. significantly ameliorated the effects on muscle fiber size in all respective groups (p = 0.010). Post hoc analysis of GTS-21 therapy vs. placebo revealed a significant effect in C.p.-injected animals revealed a significant effect (filled triangles, 1036 ± 46 μm2 vs. 826 ± 61 μm2, p = 0.011) as well as in immobilized animals (filled diamonds, 991 ± 205 μm2 vs. 781 ± 220 μm2, p = 0.002). GTS-21 was able to increase H&E area in C.p.-injected animals with disuse superimposed vs. placebo (filled circles, 955 ± 56 μm2 vs. 630 ± 87 μm2, p = 0.007). b Slow myosin fiber area. Slow myosin fiber area was significantly decreased by inflammation (p = 0.012) or mobility (p = 0.003). Therapy with GTS-21 b.i.d. significantly ameliorated the effects of pinning and C.p. in all respective groups (p = 0.004). Post hoc analysis in immobilized animals showed a significant increase in slow myosin fiber size with GTS-21 therapy compared to placebo (filled diamonds, p = 0.003). Post hoc analysis in inflammation groups showed a significant increase in slow myosin fiber size with GTS-21 therapy compared to placebo in animals with saline (empty triangles, 1184 ± 5 0 μm2 vs. 1013 ± 61 μm2, p = 0.031) or C.p.-injected (filled triangles, 1037 ± 46 μm2 vs. 879 ± 56 μm2, p = 0.041). GTS-21 was able to increase slow myosin fiber size in saline animals with disuse (×, 1176 ± 70 μm2 vs. 879 ± 75 μm2, p = 0.013). c Fast myosin fiber area. Fast myosin fiber area was significantly decreased by inflammation. (p < 0.001) or mobility (p < 0.001). Main factor therapy was not significant; however, interaction terms of mobility × therapy (p = 0.003) and inflammation × therapy (p = 0.029) were significant. Post hoc analysis of GTS-21 therapy vs. placebo revealed a significant effect in immobilized animals (filled diamonds, 1159 ± 235 μm2 vs. 993 ± 294 μm2, p = 0.003). Post hoc analysis in C.p.-injected animals with disuse superimposed revealed that GTS-21 increased fast myosin fiber area vs. placebo (filled circles, 1064 ± 58 μm2 vs. 718 ± 89 μm2, p = 0.005)
α7nAChR expression was low in rats without C.p. independent of immobilization in placebo-treated animals (0.19 ± 0.19 arbitrary units). In rats with C.p., the α7nAChR expression was significantly increased 11-fold (p < 0.001). GTS-21 significantly ameliorated α7nAChR expression in the C.p. groups by more than 60% (1.6 ± 1.2 vs. 0.6 ± 0.3 arbitrary units, p = 0.028, Fig. 6).
α7nAChR expression in the tibialis muscle (arbitrary units). a Gray background area indicates the lower and upper limit of tolerance (i.e., mean ± 1.96 × SD of the naïve leg of saline animals). Disuse alone with no inflammation did not change α7nAChR expression in muscle. α7nAChR expression was significantly increased 11-fold by C.p. (p < 0.001). Therapy with 10 mg/kg GTS-21 b.i.d. significantly ameliorated the effects in all respective groups (p < 0.001). Post hoc analysis for inflammation revealed a significant effect of therapy in saline groups (empty triangles, 0.2 ± 0.2 in placebo vs. 0.02 ± 0.02 in GTS-21 [arbitrary units], p < 0.001) and C.p. groups (filled triangles, 1.6 ± 1.2 vs. 0.6 ± 0.3, respectively [arbitrary units], p = 0.028). GTS-21 was able to decrease α7nAChR in saline groups without disuse (+, p < 0.001) and with disuse (×, p = 0.008) and C.p. groups with disuse superimposed (filled circles, p = 0.007). b Representative blots of α7nAChR expression in the tibialis muscle. Blots reveal that, similar to denervation, C.p. with and without disuse upregulates α7nAChR expression in muscle. Sham = sham-immobilization, Immob = immobilization/superimposed disuse, C.p. = systemic inflammation with Corynebacterium parvum, saline = sham-inflammation with saline, GTS = GTS-21 = DMBX-A = 3-[(3E)-3-[(2,4-dimethoxyphenyl)methylidene]-5,6-dihydro-4H-pyridin-2-yl]pyridine, bid = bis in die = twice a day
Discussion
Indicative of the presence of systemic inflammation, this study demonstrates that all C.p.-injected groups had significant elevations of MetHb levels because of increased expression of inducible nitric oxides [19, 47]. GTS-21 decreased MetHb levels compared to their respective controls. This study further demonstrates that immobilization alone reduced body weight; however, inflammation alone had a significantly greater effect. The superimposition of immobilization and inflammation further aggravated the body weight loss. In contrast, treating rats having inflammation and immobilization with GTS-21 maintained their body weight relative to day 0. A notable finding is that GTS-21 consistently attenuated tibialis muscle mass loss seen with sham-inflammation alone, immobilization alone, with inflammation alone, and when inflammation was combined with immobilization (Fig. 4a). The most salient finding is that GTS-21 also mitigated the loss of maximal tetanic tension generating capacity (functional capacity) in the animals with immobilization and in animals with inflammation and superimposed immobilization. Although single twitch tensions did not show differences in post hoc analysis for therapy, the tibialis muscle mass changes with GTS-21 was associated with statistically significant improvement in maximal tetanic tension particularly when inflammation was present with immobilization. Parenthetically, one might add tetanic tension and not single twitch measurements reflect the ability to perform repetitive work.
In previous studies during disuse atrophy [32, 41] and during denervation and sepsis [60], the upregulation of α7nAChRs has been documented. The present study documents that systemic inflammation leading to MW also results in marked upregulation of α7nAChRs in muscle (Fig. 6). When we previously characterized the used double-hit model, the changes observed included increases in MetHb levels, and acute phase reactant protein responses, and decrease of red blood cell and platelet counts [9, 57]. Two recent studies demonstrate that after injury to muscle, the α7nAChRs are upregulated (with a peak around the 7th–9th day after the impact). It was reasoned that α7nAChRs are involved in muscle regeneration by modulating inflammatory reaction and fibroblast activity [7, 59]. Experimental evidence confirming this hypothesis, however, was not provided.
The utility of GTS-21 to decrease systemic inflammatory responses has been tested in a phase II clinical trial [34], where GTS-21 could safely be used in healthy non-smoking volunteers. Although higher plasma concentration of GTS-21 significantly correlated with lower blood cytokine levels, there was no significant difference between GTS-21 vs. placebo. The ineffectiveness of GTS-21 to control cytokines was probably related to the oral dosing regimen, since the low bioavailability of orally administered GTS-21 resulted in relatively low blood concentrations (mean, 13 ng/ml at time of LPS administration). GTS-21 has previously been administered orally to healthy, schizophrenic, Alzheimer’s disease, and attention-deficit hyperactivity disorder subjects in clinical tests [11, 29, 33, 50]. These human clinical studies are indeed important in that no serious side effects have been documented, paving the way for more studies with GTS-21 using alternative routes of administration. In our study, a dose of 10 mg/kg b.i.d. demonstrated especially beneficial effects evidenced by the attenuation of inflammation alone-induced and inflammation with disuse-induced biochemical, physiological, and functional changes. These findings suggest that the α7nAChRs could be used to advantage to mitigate the inflammatory responses and its consequences on body weight, muscle mass, and force if initiated at the beginning of a perturbation and continued during prolonged systemic inflammation.
Our dose of 10 mg/kg GTS-21 did not completely reverse the body weight and muscle changes. Treatment for longer period than 12 days may have most likely reversed muscle mass faster than untreated controls. The pharmacokinetics, however, of GTS-21 in critically illness of rodents is unknown. Some drugs have a faster clearance in critical illness [5, 17, 18]. Thus, alternative therapeutic modalities such as smaller, more frequent doses and/or for longer periods may result in complete reversal of changes.
GTS-21 downregulated α7nAChR expression in tibialis muscle in all groups, especially in inflammation animals by more than 60% compared to controls. This downregulation probably suggests decreased inflammation in muscle, consistent with a previous in vitro finding in macrophages [30] and this study that inflammation upregulates α7nAChR expression. The downregulation was concomitantly associated with mitigation of the inflammation-induced biochemical and body mass and muscle changes including force. This begs the question whether the site of action of GTS-21 is via actions on α7nAChRs on circulating cells or on muscle itself. Future studies with depletion of cells are warranted as which of the α7nAChRs (muscle vs. macrophages) play a more predominant role. These studies could include the use of muscle specific α7nAChR knockout mice (currently not available) or by a depletion of macrophages in vivo [24].
Our study has some limitations. First, we did not measure cytokines levels as inflammation markers, but only methemoglobin as previously [9, 57]. Second, our study is descriptive and does not provide mechanistic data to establish a direct link of GTS-21 induced α7nAChR reduction on improvements in muscle mass and function. Third, in order to have a clinically relevant model, e.g., a longer duration of immobilization and inflammation, as well as clinically relevant endpoints, we performed an in vivo study. This results in a higher variability because of the individual responses of the different animals.
In summary, most previous studies focused on altering disease-induced muscle changes to reverse MW of critical illness. This current study is different in that it attempts control systemic and possibly local inflammation in muscle to reverse or mitigate the disease-associated changes. Using a novel molecular target, namely the α7nAChRs, we confirmed our hypothesis that modulation of inflammatory responses via α7nAChRs by use of GTS-21 can indeed attenuate body mass, muscle mass, and/or tension loss when inflammation is present alone and with immobilization. The current study also adds to the evidence that the α7nAChR is a novel target that might be the subject of future studies concerned with inflammation and organ dysfunction [30, 35]. These findings are indeed encouraging in view of the recent clinical trials on α7nAChR modulators in humans to control lipopolysaccharide-induced inflammatory responses [36] and safe use of α7nAChR agonists to treat neuro-inflammation and schizophrenia [6]. Our findings could have direct applications to the bedside after validations of some of the questions that have been raised by us.
References
Blobner M, Kochs E, Fink H, Mayer B, Veihelmann A, Brill T, Stadler J (1999) Pharmacokinetics and pharmacodynamics of vecuronium in rats with systemic inflammatory response syndrome: treatment with NG-monomethyl-L-arginine. Anesthesiology 91:999–1005
Briggs CA, Anderson DJ, Brioni JD, Buccafusco JJ, Buckley MJ, Campbell JE, Decker MW, Donnelly-Roberts D, Elliott RL, Gopalakrishnan M, Holladay MW, Hui YH, Jackson WJ, Kim DJ, Marsh KC, O'Neill A, Prendergast MA, Ryther KB, Sullivan JP, Arneric SP (1997) Functional characterization of the novel neuronal nicotinic acetylcholine receptor ligand GTS-21 in vitro and in vivo. Pharmacol Biochem Behav 57:231–241
Buras JA, Holzmann B, Sitkovsky M (2005) Animal models of sepsis: setting the stage. Nat Rev Drug Discov 4:854–865
Casaer MP (2015) Muscle weakness and nutrition therapy in ICU. Curr Opin Clin Nutr Metab Care 18:162–168
Choi L, Ferrell BA, Vasilevskis EE, Pandharipande PP, Heltsley R, Ely EW, Stein CM, Girard TD (2016) Population pharmacokinetics of fentanyl in the critically ill. Crit Care Med 44:64–72
Conejero-Goldberg C, Davies P, Ulloa L (2008) Alpha7 nicotinic acetylcholine receptor: a link between inflammation and neurodegeneration. Neurosci Biobehav Rev 32:693–706
Fan YY, Zhang ST, Yu LS, Ye GH, Lin KZ, Wu SZ, Dong MW, Han JG, Feng XP, Li XB (2014) The time-dependent expression of alpha7nAChR during skeletal muscle wound healing in rats. Int J Legal Med 128:779–786
Fink H, Bogdanski R, Luppa P, Martyn JA, Blobner M (2005) Nitric oxide is not a mediator of inflammation-induced resistance to atracurium. Anesth Analg 101:1362–1367
Fink H, Helming M, Unterbuchner C, Lenz A, Neff F, Martyn JA, Blobner M (2008) Systemic inflammatory response syndrome increases immobility-induced neuromuscular weakness. Crit Care Med 36:910–916
Fink H, Luppa P, Mayer B, Rosenbrock H, Metzger J, Martyn JA, Blobner M (2003) Systemic inflammation leads to resistance to atracurium without increasing membrane expression of acetylcholine receptors. Anesthesiology 98:82–88
Freedman R, Olincy A, Buchanan RW, Harris JG, Gold JM, Johnson L, Allensworth D, Guzman-Bonilla A, Clement B, Ball MP, Kutnick J, Pender V, Martin LF, Stevens KE, Wagner BD, Zerbe GO, Soti F, Kem WR (2008) Initial phase 2 trial of a nicotinic agonist in schizophrenia. Am J Psychiatry 165:1040–1047
Frick CG, Helming M, Martyn JA, Blobner M, Fink H (2010) Continuous administration of pyridostigmine improves immobilization-induced neuromuscular weakness. Crit Care Med 38:922–927
Friedrich O, Reid MB, Van den Berghe G, Vanhorebeek I, Hermans G, Rich MM, Larsson L (2015) The sick and the weak: neuropathies/myopathies in the critically ill. Physiol Rev 95:1025–1109
Ghosh R, Gilda JE, Gomes AV (2014) The necessity of and strategies for improving confidence in the accuracy of western blots. Expert Rev Proteomics 11:549–560
Gilda JE, Gomes AV (2015) Western blotting using in-gel protein labeling as a normalization control: stain-free technology. Methods Mol Biol 1295:381–391
Gurtler A, Kunz N, Gomolka M, Hornhardt S, Friedl AA, McDonald K, Kohn JE, Posch A (2013) Stain-free technology as a normalization tool in western blot analysis. Anal Biochem 433:105–111
Han T, Harmatz JS, Greenblatt DJ, Martyn JA (2007) Fentanyl clearance and volume of distribution are increased in patients with major burns. J Clin Pharmacol 47:674–680
Han TH, Greenblatt DJ, Martyn JA (2009) Propofol clearance and volume of distribution are increased in patients with major burns. J Clin Pharmacol 49:768–772
Herencia F, Lopez-Garcia MP, Ubeda A, Ferrandiz ML (2002) Nitric oxide-scavenging properties of some chalcone derivatives. Nitric Oxide 6:242–246
Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS, Canadian critical care trials G (2003) One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 348:683–693
Herridge MS, Tansey CM, Matte A, Tomlinson G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart TE, Kudlow P, Cook D, Slutsky AS, Cheung AM, Canadian critical care trials G (2011) Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med 364:1293–1304
Hirose M, Kaneki M, Sugita H, Yasuhara S, Ibebunjo C, Martyn JA (2001) Long-term denervation impairs insulin receptor substrate-1-mediated insulin signaling in skeletal muscle. Metabolism 50:216–222
Hirose M, Kaneki M, Sugita H, Yasuhara S, Martyn JA (2000) Immobilization depresses insulin signaling in skeletal muscle. Am J Physiol Endocrinol Metab 279:E1235–E1241
Jiang S, Gavrikova TA, Sharifov OF, Messina JL (2012) Role of tissue macrophages in the development of critical illness diabetes. Shock 37:70–76
Kalashnyk O, Lykhmus O, Oliinyk O, Komisarenko S, Skok M (2014) α7 Nicotinic acetylcholine receptor-specific antibody stimulates interleukin-6 production in human astrocytes through p38-dependent pathway. Int Immunopharmacol 23:475–479
Kashiwagi S, Khan MA, Yasuhara S, Goto T, Kem WR, Tompkins RG, Kaneki M, Martyn JA (2017) Prevention of burn-induced inflammatory responses and muscle wasting by GTS-21, a specific agonist for alpha7 nicotinic acetylcholine receptors. Shock 47:61–69
Kem W, Soti F, Wildeboer K, LeFrancois S, MacDougall K, Wei D-Q, Chou K-C, Arias HR (2006) The nemertine toxin anabaseine and its derivative DMXBA (GTS-21): chemical and pharmacological properties. Marine Drugs 4:255–273
Kem WR (2000) The brain alpha7 nicotinic receptor may be an important therapeutic target for the treatment of Alzheimer’s disease: studies with DMXBA (GTS-21). Behav Brain Res 113:169–181
Kem WR, Olincy A, Johnson L, Harris J, Wagner BD, Buchanan RW, Christians U, Freedman R (2017) Pharmacokinetic limitations on effects of an alpha7-nicotinic receptor agonist in schizophrenia: randomized trial with an extended-release formulation. Neuropsychopharmacology
Khan MA, Farkhondeh M, Crombie J, Jacobson L, Kaneki M, Martyn JA (2012) Lipopolysaccharide upregulates alpha7 acetylcholine receptors: stimulation with GTS-21 mitigates growth arrest of macrophages and improves survival in burned mice. Shock 38:213–219
Khan MA, Khan MF, Kashiwagi S, Kem WR, Yasuhara S, Kaneki M, Tompkins RG, Martyn JA (2017) An alpha7 nicotinic acetylcholine receptor agonist (GTS-21) promotes C2C12 Myonuclear accretion in association with release of Interleukin-6 (IL-6) and improves survival in burned mice. Shock 48:227–235
Khan MA, Sahani N, Neville KA, Nagashima M, Lee S, Sasakawa T, Kaneki M, Martyn JA (2014) Nonsurgically induced disuse muscle atrophy and neuromuscular dysfunction upregulates alpha7 acetylcholine receptors. Can J Physiol Pharmacol 92:1–8
Kitagawa H, Takenouchi T, Azuma R, Wesnes KA, Kramer WG, Clody DE, Burnett AL (2003) Safety, pharmacokinetics, and effects on cognitive function of multiple doses of GTS-21 in healthy, male volunteers. Neuropsychopharmacology 28:542–551
Kox M, Pompe JC, Gordinou de Gouberville MC, van der Hoeven JG, Hoedemaekers CW, Pickkers P (2011) Effects of the alpha7 nicotinic acetylcholine receptor agonist GTS-21 on the innate immune response in humans. Shock 36:5–11
Kox M, Pompe JC, Peters E, Vaneker M, van der Laak JW, van der Hoeven JG, Scheffer GJ, Hoedemaekers CW, Pickkers P (2011) alpha7 nicotinic acetylcholine receptor agonist GTS-21 attenuates ventilator-induced tumour necrosis factor-alpha production and lung injury. Br J Anaesth 107:559–566
Kox M, Pompe JC, van der Hoeven JG, Hoedemaekers CW, Pickkers P (2011) Influence of different breathing patterns on heart rate variability indices and reproducibility during experimental endotoxaemia in human subjects. Clin Sci (Lond) 121:215–222
Kress JP, Hall JB (2014) ICU-acquired weakness and recovery from critical illness. N Engl J Med 370:1626–1635
Langhans C, Weber-Carstens S, Schmidt F, Hamati J, Kny M, Zhu X, Wollersheim T, Koch S, Krebs M, Schulz H, Lodka D, Saar K, Labeit S, Spies C, Hubner N, Spranger J, Spuler S, Boschmann M, Dittmar G, Butler-Browne G, Mouly V, Fielitz J (2014) Inflammation-induced acute phase response in skeletal muscle and critical illness myopathy. PLoS One 9:e92048
Latronico N, Guarneri B (2008) Critical illness myopathy and neuropathy. Minerva Anestesiol 74:319–323
Lee RH, Vazquez G (2013) Evidence for a prosurvival role of alpha-7 nicotinic acetylcholine receptor in alternatively (M2)-activated macrophages. Physiological reports 1:e00189
Lee S, Yang HS, Sasakawa T, Khan MA, Khatri A, Kaneki M, Martyn JA (2014) Immobilization with atrophy induces de novo expression of neuronal nicotinic alpha7 acetylcholine receptors in muscle contributing to neurotransmission. Anesthesiology 120:76–85
Levine S, Nguyen T, Taylor N, Friscia ME, Budak MT, Rothenberg P, Zhu J, Sachdeva R, Sonnad S, Kaiser LR, Rubinstein NA, Powers SK, Shrager JB (2008) Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med 358:1327–1335
Liu L, Min S, Li W, Wei K, Luo J, Wu G, Ao L, Cao J, Wang B, Wang Z (2014) Pharmacodynamic changes with vecuronium in sepsis are associated with expression of alpha7- and gamma-nicotinic acetylcholine receptor in an experimental rat model of neuromyopathy. Br J Anaesth 112:159–168
Maldifassi MC, Atienza G, Arnalich F, Lopez-Collazo E, Cedillo JL, Martin-Sanchez C, Bordas A, Renart J, Montiel C (2014) A new IRAK-M-mediated mechanism implicated in the anti-inflammatory effect of nicotine via alpha7 nicotinic receptors in human macrophages. PLoS One 9:e108397
Martyn JA, Fagerlund MJ, Eriksson LI (2009) Basic principles of neuromuscular transmission. Anaesthesia 64(Suppl 1):1–9
Mayer B, Fink H, Bogdanski R, Stadler J, Blobner M (2001) Inflammatory liver disease shortens atracurium-induced neuromuscular blockade in rats. Eur J Anaesthesiol 18:599–604
Metcalf K, Jungersten L, Lisander B (2002) Effective inhibition of nitric oxide production by aminoguanidine does not reverse hypotension in endotoxaemic rats. Acta Anaesthesiol Scand 46:17–23
Meyer EM, Tay ET, Papke RL, Meyers C, Huang GL, de Fiebre CM (1997) 3-[2,4-Dimethoxybenzylidene]anabaseine (DMXB) selectively activates rat alpha7 receptors and improves memory-related behaviors in a mecamylamine-sensitive manner. Brain Res 768:49–56
Mondello P, Mian M, Aloisi C, Fama F, Mondello S, Pitini V (2015) Cancer cachexia syndrome: pathogenesis, diagnosis, and new therapeutic options. Nutr Cancer 67:12–26
Olincy A, Harris JG, Johnson LL, Pender V, Kongs S, Allensworth D, Ellis J, Zerbe GO, Leonard S, Stevens KE, Stevens JO, Martin L, Adler LE, Soti F, Kem WR, Freedman R (2006) Proof-of-concept trial of an alpha7 nicotinic agonist in schizophrenia. Arch Gen Psychiatry 63:630–638
Osta WA, El-Osta MA, Pezhman EA, Raad RA, Ferguson K, McKelvey GM, Marsh HM, White M, Perov S (2010) Nicotinic acetylcholine receptor gene expression is altered in burn patients. Anesth Analg 110:1355–1359
Poli-de-Figueiredo LF, Garrido AG, Nakagawa N, Sannomiya P (2008) Experimental models of sepsis and their clinical relevance. Shock 30(Suppl 1):53–59
Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, Hopkinson NS, Padhke R, Dew T, Sidhu PS, Velloso C, Seymour J, Agley CC, Selby A, Limb M, Edwards LM, Smith K, Rowlerson A, Rennie MJ, Moxham J, Harridge SDR, Hart N, Montgomery HE (2013) Acute skeletal muscle wasting in critical illness. JAMA - J Am Med Assoc 310:1591–1600
Rivero-Gutierrez B, Anzola A, Martinez-Augustin O, de Medina FS (2014) Stain-free detection as loading control alternative to Ponceau and housekeeping protein immunodetection in western blotting. Anal Biochem 467:1–3
Schaller SJ, Anstey M, Blobner M, Edrich T, Grabitz SD, Gradwohl-Matis I, Heim M, Houle T, Kurth T, Latronico N, Lee J, Meyer MJ, Peponis T, Talmor D, Velmahos GC, Waak K, Walz JM, Zafonte R, Eikermann M, International early S-gMRI (2016) Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet 388:1377–1388
Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, Spears L, Miller M, Franczyk M, Deprizio D, Schmidt GA, Bowman A, Barr R, McCallister KE, Hall JB, Kress JP (2009) Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 373:1874–1882
Stauble CG, Helming M, Martyn JA, Blobner M, Fink H (2016) Neuromuscular recovery is prolonged after immobilization or superimposition of inflammation with immobilization compared to inflammation alone: data from a preclinical model. Crit Care Med 44:e1097–e1110
Stevens RD, Dowdy DW, Michaels RK, Mendez-Tellez PA, Pronovost PJ, Needham DM (2007) Neuromuscular dysfunction acquired in critical illness: a systematic review. Intensive Care Med 33:1876–1891
Tian ZL, Jiang SK, Zhang M, Wang M, Li JY, Zhao R, Wang LL, Liu M, Li SS, Zhang MZ, Guan DW (2015) alpha7nAChR is expressed in satellite cells at different myogenic status during skeletal muscle wound healing in rats. J Mol Histol 46:499–509
Tsuneki H, Salas R, Dani JA (2003) Mouse muscle denervation increases expression of an alpha7 nicotinic receptor with unusual pharmacology. J Physiol 547:169–179
van Haaren F, Anderson KG, Haworth SC, Kem WR (1999) GTS-21, a mixed nicotinic receptor agonist/antagonist, does not affect the nicotine cue. Pharmacol Biochem Behav 64:439–444
van Maanen MA, Papke RL, Koopman FA, Koepke J, Bevaart L, Clark R, Lamppu D, Elbaum D, LaRosa GJ, Tak PP, Vervoordeldonk MJ (2015) Two novel alpha7 nicotinic acetylcholine receptor ligands: in vitro properties and their efficacy in collagen-induced arthritis in mice. PLoS One 10:e0116227
Veihelmann A, Brill T, Blobner M, Scheller I, Mayer B, Prolls M, Himpel S, Stadler J (1997) Inhibition of nitric oxide synthesis improves detoxication in inflammatory liver dysfunction in vivo. Am J Phys 273:G530–G536
Vincent JL, Norrenberg M (2009) Intensive care unit-acquired weakness: framing the topic. Crit Care Med 37:S296–S298
Weber-Carstens S, Schneider J, Wollersheim T, Assmann A, Bierbrauer J, Marg A, Al Hasani H, Chadt A, Wenzel K, Koch S, Fielitz J, Kleber C, Faust K, Mai K, Spies CD, Luft FC, Boschmann M, Spranger J, Spuler S (2013) Critical illness myopathy and GLUT4: significance of insulin and muscle contraction. Am J Respir Crit Care Med 187:387–396
Wollersheim T, Woehlecke J, Krebs M, Hamati J, Lodka D, Luther-Schroeder A, Langhans C, Haas K, Radtke T, Kleber C, Spies C, Labeit S, Schuelke M, Spuler S, Spranger J, Weber-Carstens S, Fielitz J (2014) Dynamics of myosin degradation in intensive care unit-acquired weakness during severe critical illness. Intensive Care Med 40:528–538
Acknowledgements
The authors would like to thank Univ. Prof. Dr. med., Dipl.-Phys. Eberhard Kochs for his continued scientific advice and support and the following collaborators for their technical assistance: Sandra Baur, Andreas Blaschke, Nina Bayer, Anna Folz, Eva Nuspl (all from Klinikum rechts der Isar, Technical University of Munich, Germany).
Funding
Support in Munich, Germany, was provided solely from institutional and/or departmental sources. Jeevendra Martyn was supported in part by grants from the National Institutes of Health, Bethesda, MD (P50-GM21500, Project I, and RO1-GM 118947) and grants from Shriners Hospitals for Children®—Tampa, FL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Research involving animals
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted. This animal study was approved by the institutional review board (Subcommittee on Research Animal Care, Committee on Research, Massachusetts General Hospital, #2010N000168).
Rights and permissions
About this article
Cite this article
Schaller, S.J., Nagashima, M., Schönfelder, M. et al. GTS-21 attenuates loss of body mass, muscle mass, and function in rats having systemic inflammation with and without disuse atrophy. Pflugers Arch - Eur J Physiol 470, 1647–1657 (2018). https://doi.org/10.1007/s00424-018-2180-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-018-2180-6