Abstract
Interleukin-17A (IL-17A) is an important pro-inflammatory cytokine that regulates leukocyte mobilization and recruitment. To better understand how IL-17A controls leukocyte trafficking across capillaries in the peripheral blood circulation, we used primary human dermal microvascular endothelial cells (HDMEC) to investigate their secretory potential and barrier function when activated with IL-17A and TNFα. Activation by TNFα and IL-17A causes phosphorylation of p38 as well as IκBα whereby NFκB subsequently becomes phosphorylated, a mechanism that initiates transcription of adhesion molecules such as E-selectin. Members of the neutrophil-specific GRO-family chemokines were significantly up-regulated upon IL-17A stimulation on the mRNA and protein level, whereas all tested non-neutrophil-specific chemokines remained unchanged in comparison. Moreover, a striking synergistic effect in the induction of granulocyte colony-stimulating factors (G-CSF) was elicited when IL-17A was used in combination with TNFα, and IL-17A was able to significantly augment the levels of TNFα-induced E-selectin and ICAM-1. In accordance with this observation, IL-17A was able to markedly increase TNFα-induced neutrophil adherence to HDMEC monolayers in an in vitro adhesion assay. Using a trans-well migration assay with an HDMEC monolayer as a barrier, we here show that pre-stimulating the endothelial cells with TNFα and IL-17A together enhances the rate of neutrophil transmigration compared to TNFα or IL-17A alone. These results show that IL-17A and TNFα act in cooperation to facilitate neutrophil migration across the endothelial cell barrier. In addition, the synergistic actions of IL-17A with TNFα to secrete G-CSF appear to be important for mobilizing neutrophils from the bone marrow to the blood stream.
Similar content being viewed by others
Introduction
The interleukin-17 (IL-17) family comprises six members, IL-17A through IL-17F [33]. Of these, IL-17A is best described and is believed to play an important role in regulating monocyte and neutrophil recruitment during inflammatory conditions [25]. IL-17A is produced primarily by Th17 cells [56] which have been implicated in the pathogenesis of auto-immune and inflammatory diseases in humans [24]. By binding to its trans-membrane receptor complex, consisting of the IL-17RA and IL-17RC subunits, IL-17A affects the expression of many genes involved in inflammatory processes, but the exact expressional pattern varies considerably depending on cell type [35]. The IL-17 receptor is ubiquitously expressed, and IL-17A target genes have been reported to include a multitude of cytokines such as IL-1β, TNFα, IL-6 and granulocyte colony-stimulating factor (G-CSF) as well as chemokines including CXCL1, CXCL8 and CXCL10. Other regulated genes include several members of the C-C motif family of chemokines and various anti-microbial peptides. The expression of many non-secreted molecules such as ICAM-1, iNOS and COX-2 is also affected by IL-17A, further supporting its role as a pro-inflammatory cytokine [23, 35]. Furthermore, IL-17 receptor knock-out mice have accelerated disease progression and suffer early deaths, as a result of impaired neutrophil recruitment, when challenged with Klebsiella pneumonia [55]. In patients with inflammatory bowel disease, the numbers of IL-17A-producing T-cells and serum levels of IL-17A correlate with disease severity [15]. Moreover, patients suffering from psoriasis have increased serum levels of IL-17A, strongly indicating an involvement of this molecule in auto-immunity [46]. It has also been shown that the number of IL-17A-producing T-cells is significantly increased in aged individuals compared to young healthy ones, implicating a role for IL-17A in ageing processes [36].
The ability of IL-17A to stimulate the maturation/mobilization as well as the recruitment of neutrophils to sites of inflammation is heavily supported in the literature. Initially, Fossiez et al. [13] found that IL-17A-stimulated fibroblasts produced G-CSF and IL-8. Subsequently, Witowski et al. [50, 51] demonstrated that G-CSF and GROα derived from mesothelial cells caused massive peritoneal neutrophil infiltration when IL-17A was administered as an i.p. bolus. Moreover, Schwarzenberger et al. [42] showed that adenovirus-mediated IL-17A over-expression caused increased levels of G-CSF which correlated with a marked neutrophilia in mice. IL-17A also promotes the expression of the neutrophil-specific chemokine IL-8 in different cell types such as intestinal epithelial cells, keratinocytes and airway endothelial cells [2, 10, 32, 39]. IL-17A has likewise been reported to augment the production of several non-neutrophil-specific cytokines, including GM-CSF, MCP-1 and CCL20, in various cell types such as vascular smooth muscle cells, rheumatoid synoviocytes, endothelial cells and endometriotic stromal cells [8, 9, 13, 22, 37]. The fact that so many cell types express the IL-17 receptor makes it difficult to evaluate the relative contribution of each to the inflammatory milieu. Moreover, IL-17A has been reported to interact with other pro-inflammatory cytokines such as TNFα and IL-1β, making it even more difficult to decipher its specific actions [8, 9]. Thus, the exact role of IL-17A during inflammation is still unclear. We hypothesized that the effect of IL-17A is highly dependent on the cell and/or tissue context and therefore set out to investigate the role of this cytokine in an isolated system of human dermal microvascular endothelial cells. Our goal was to characterize the specific effects of IL-17A, focusing on the interaction between IL-17A and TNFα and their role in regulating neutrophil biology via the microvascular endothelium. We also hypothesized that the effects of IL-17 alone are small compared to those of TNFα and that the true importance of IL-17A can only be seen in combination with TNFα. Here, we show that in the human microvascular endothelium, IL-17 and TNFα interact in the endothelial cells by causing granulocyte mobilization via adhesion molecule expression and cytokine secretion.
Materials and methods
Reagents
Recombinant human (rh)IL-17A and recombinant human (rh)TNFα were obtained from R&D systems (Abingdon, UK). Bovine fibrinogen and bovine ferricytochrome C as well as phorbol 12-myristate 13-acetate (PMA) and N-formyl-l-methionyl-l-leucyl-l-phenylalanine (fMLP) was from Sigma (St. Louis, MO, USA). Calcein-AM, SYBR® Safe DNA stain and rabbit anti-p38 (pT180/pY182) were from Invitrogen (Carlsbad, CA, USA). Rabbit anti-IκBα binding [pSpS32/36] and rabbit anti-NFκB binding [pS529] antibodies were from Biosource International Inc., USA. Mouse anti-GAPDH was from Millipore (Billerica, MA, USA). Human P-selectin/CD62P blocking antibody, human E-selectin/CD62E blocking antibody and isotype control antibody were from R&D systems (Abingdon, UK). Collagen I (rat tail) was from Becton Dickinson (Franklin Lakes, NJ, USA).
Cell lines and cell culture
Human dermal microvascular endothelial cells (HDMEC) and human umbilical vein endothelial cells (HUVEC) were purchased from Promocell (Heidelberg, Germany). The cells were cultured in tissue-culture-treated collagen-I-coated (50 μg/ml) flasks using basal MCDB-131 medium supplemented with 5 % FCS, 0.4 % endothelial cell growth supplement (ECGS), 10 ng/ml epidermal growth factor (EGF), 1 μg/ml hydrocortisone, 200 U/ml penicillin and 50 μg/ml streptomycin. Medium and all supplements except antibiotics were purchased from Promocell. The cells were used until the ninth passage. For all experiments, HDMEC and HUVEC were cultured on collagen-I-coated (50 μg/ml) materials.
Human neutrophils were isolated from whole venous blood obtained from a healthy donor by centrifugation on a discontinuous density gradient of Ficoll-Hypaque with subsequent hypotonic lysis of red blood cells. Neutrophil viability was evaluated by trypan blue exclusion and was found to be > 95 % routinely. The percentage of isolated cells displaying a non-neutrophil morphology was found to be less than 5 %.
RNA purification
Cells were grown until (newly) confluent in 24-well or 6-well plates. Subsequently, their growth medium was exchanged with fresh medium, and the cells were stimulated with cytokines. Total RNA was extracted using the RNeasy® mini kit from Qiagen (Hilden, Germany) according to the manufacturer's instructions.
Quantitative real-time PCR
RNA was extracted and reverse-transcribed using the Omniscript® mini kit from Qiagen according to the manufacturer's instructions. Quantitative real-time PCR (qRT-PCR) was performed in 96-well plate format using SYBR green-based detection on an Mx3000PTM thermal cycler from Agilent Technologies (Santa Clara, CA, USA). Each reaction contained 1× Brilliant® SYBR® green QPCR master mix from Agilent Technologies. The plate was sealed and cycled under the following conditions: 95 °C for 10 min, 40 cycles of 95 °C for 30 s (melting), 40 cycles of 55–62 °C for 60 s (annealing) and 40 cycles of 72 °C for 60 s (elongation) (Table 1). Each reaction was performed in triplicate. Triplicate reactions for detection of GAPDH mRNA levels were used for normalization between samples. Fold changes were determined from cycle threshold values using the ∆∆CT method. Sequences of primers used were as shown in Table 1.
FACS method
The surface expression of IL-17R on HDMECs was assessed using flow cytometry. Cultures of HDMEC were harvested using a VERSENE chelating medium (containing EDTA, DOW, USA) and washed in PBS with 5 % FCS and stained with Alexa Fluor® 647 (Red A) anti-human CD217 (IL-17RA) antibody (# 340903 Biolegend, San Diego, CA, USA) and as a control mouse IgG1 K Isotype (Yellow A) (# 12–4714 eBioscience, San Diego, CA, USA) for 30 min in the dark at 4 °C. Data acquisition and analysis were done using a FACSArray™ (BD Biosciences).
Western blotting
Cells were grown to 90 % confluence in tissue-culture-treated polystyrene petri-dishes and serum-starved in serum-free basal medium containing 2 % FCS for 90 min before stimulation. After stimulation, the medium was aspirated, and all reactions were stopped by the addition of lysis buffer. The lysates were analysed by western blotting as described previously [12].
ELISA
Cells were grown until (newly) confluent in 24-well or 12-well plates. Subsequently, their growth medium was exchanged with fresh medium, and the cells were stimulated with cytokines.
Human IL-8, CXCL10, GROα, G-CSF, E-selectin, VCAM-1 and ICAM-1 DuoSet ELISA kits were purchased from R&D Systems. Cell supernatant or whole cell lysate was collected after cell stimulation and stored at −20 °C until used for quantification. The total amount of target proteins in the lysate from each well was normalized to the total amount of cells by labelling with SYBR® Safe DNA stain (10.000× concentrate diluted to 5× concentrate) added directly to the lysis buffer. The amount of fluorescence (proportional to the number of cells) was determined using a Synergy HT microplate reader from BioTek® (Winooski, VT, USA).
Neutrophil adhesion assay
Neutrophil adhesion to fibrinogen
Freshly isolated human neutrophils, which had been loaded in advance with calcein (1 μM) for 45 min at room temperature, were added to each well (1.5 × 105 cells/well) of a 96-well plate which had been pre-coated for 3 h at room temperature using a solution of 1 mg/ml bovine fibrinogen in PBS without Ca2+/Mg2+. Cells were allowed to adhere for 30 min in the presence of either IL-17A or fMLF as a positive control. Fluorescence was measured (485 nm excitation, 520 nm emission) immediately hereafter using a Synergy HT microplate reader from BioTek® and then measured again after the wells had been washed twice with PBS. Neutrophil adherence was calculated according to the equation below.
Neutrophil adhesion to HDMEC
HDMEC were grown until (newly) confluent in 24-well plates. Subsequently, their growth medium was exchanged with fresh, and the cells were stimulated with cytokines. Afterwards, the cell monolayers were washed twice in adhesion buffer (MCDB-131 medium containing antibiotics and 10 % FCS). Then, freshly isolated human neutrophils, which had been loaded in advance with calcein (1 μM) for 45 min at room temperature, were added to each well (2–4 × 105 cells/well) and allowed to adhere for 20 min. Fluorescence was measured (485 nm exCitation, 520 nm emission) immediately hereafter using a Synergy HT microplate reader from BioTek® and then measured again after the wells had been washed twice with PBS. Neutrophil adherence was calculated according to the equation below. In some experiments, anti-human P-selectin, anti-human E-selectin or isotype control antibodies were added to the endothelial cells 1 h before the addition of neutrophils. Immediately before adding neutrophils, unbound antibodies were washed away by three washes in adhesion buffer.
Transmigration assay
HDMEC were seeded (60,000/well) in the insert wells of 96-well FalconTM FluoroBlokTM plates (8 μm) and allowed to reach confluence for 48 h before they were washed twice in growth medium and subsequently stimulated with cytokines. After stimulation, the cell monolayers were washed twice in transmigration buffer (MCDB-131 medium containing antibiotics and 10 % FCS). Then, freshly isolated human neutrophils, which had been loaded in advance with calcein (1 μM) for 45 min at room temperature, were added to each insert well (1 × 105 cells/well) and allowed to transmigrate for 90 min. Fluorescence was measured (485 nm excitation, 520 nm emission) immediately hereafter using a Synergy HT microplate reader from BioTek®. Neutrophils appearing on the endothelial cell layer after transmigration were visualized using a fluorescence microscope with a 20 × 0.75 numeric aperture objective from Olympus (Japan) and a MetaMorph Imaging system as previously described [21].
Measurements of superoxide radical generation
The ability of human neutrophils to generate superoxide anion was assayed by the reduction of bovine ferricytochrome C. Freshly isolated human neutrophils were re-suspended in a modified phosphate-buffered Krebs-Ringer solution containing 1 mM glucose. The cell suspension (7.5 × 105 cells/ml) was distributed in the wells of a polystyrene tissue-culture-treated 96-well plate (200 μl/well) which had been pre-coated for 3 h at room temperature using a solution of 1 mg/ml bovine fibrinogen in PBS without Ca2+/Mg2+. Then, 20 μl of ferricytochrome C (10 mg/ml in PBS without Ca2+/Mg2+) was added to a final concentration of 75 μM. The cells were allowed to adhere for 1 h prior to the addition of stimulators. The relative amount of superoxide anion formation was measured by reading the absorbance of reduced cytochrome C at 550 nm in a Synergy HT microplate reader from BioTek® with 630 nm as reference.
Statistical evaluations
Data are presented as means ± standard deviation (SD). Statistical evaluation of the results was made by a two-tailed Student's t-test not assuming equal variance between groups. P-values are indicated with * ≤ 0.05, ** ≤ 0.01 and *** ≤ 0.001.
Results
Human microvascular endothelial cells express the IL-17A receptor
Our first objective was to verify the ability of HDMEC to signal through the IL-17A receptor. The precise molecular composition with regards to stoichiometry and structure of the IL-17 receptor is still unclear, but it is believed that at least two subunits, IL-17RA and IL-17RC are necessary to make up a functional receptor complex for signalling upon IL-17A binding [16]. By reverse transcription of total cellular RNA followed by PCR amplification using IL-17RA and IL-17RC transcript selective primers (intron spanning), we identified the presence of these transcripts in HDMEC (Fig. 1a). In addition, FACS analysis revealed a low expression of IL-17RA in unstimulated HDMEC comprising 25 % of the cell population (Fig. 1b).
Human microvascular endothelial cells express and signal through the IL-17A receptor. a Agarose-gel photos showing PCR products for IL-17RA (548 bp) and IL-17RC (416 bp) at the predicted band sizes loaded next to a DNA ladder for band size determination. b Expression of IL-17 receptor A (IL-17RA) on human dermal microvascular endothelial cells (HDMECs) as shown by surface binding of IL-17RA antibody (black curve) compared to control IgG1 antibody (grey curve) using a BD FACSArray. The mean fluorescent intensity (MFI) is 99 for control and 689 for IL-17RA antibody. One representative experiment out of three. c Western blotting showing phosphorylation of p38 (P-p38), IκBα (P- IκBα) and NFκB (P-NFκB) after stimulation with IL-17A (50 ng/ml) and TNFα (10 ng/ml) alone or together. d Measurements of grey values from the Western blotting of P-p38 and P-NFκB
When HDMEC were stimulated with IL-17A phosphorylation of the MAP kinase, p38 was significantly increased after 20 min (Fig. 1c, d). p38 phosphorylation by IL-17A was reported previously in other cell types [3, 38, 44]. Figure 1c, d also shows the powerful effect of TNFα on p38 phosphorylation both in the presence and absence of IL-17A. The effect is sustained over 30 min and several fold larger than the effect of IL-17A alone. TNFα is known to be a powerful activator of NFκB, and we therefore investigated the role of both IL-17A and TNFα in the activation process. We, at first, determined the phosphorylation of IκBα that releases the NFκB complex for influx into the nucleus. We found that IκBα is phosphorylated following TNFα stimulation with and without IL-17A after 10 min, but phosphorylation was undetectable after 20 min. The consequence of this phosphorylation is the subsequent phosphorylation of NFκB. Stimulation with TNFα and TNFα + IL-17A results in a powerful phosphorylation of NFκB after 10 min, and the effect is detectable up to 30 min (Fig. 1c, d).
IL-17A cooperates with TNFα in the induction of G-CSF and GRO-family chemokines
IL-17A plays an important role in recruiting monocytes and neutrophils to sites of inflammation [45]. We therefore investigated whether IL-17A regulated the expression of CSFs which are known to affect leukocyte mobilization and recruitment by mediating their maturation and release from the bone marrow [7].
Using qRT-PCR and ELISA, we found that IL-17A specifically enhanced HDMEC expression of G-CSF on both mRNA and protein level and that IL-17A could function in synergy with TNFα in this effect (Fig. 2a, b). Similar results were obtained using HUVEC as analysed by qRT-PCR (data not shown). In marked contrast, there was no interaction between IL-17A and TNFα on HDMEC expression of macrophage-CSF (M-CSF) (Table 2) for which TNFα alone was a strong inducer (data not shown).
IL-17A cooperates with TNFα in the induction of G-CSF and GRO-family chemokines. a Relative mRNA levels of G-CSF in HDMEC challenged with IL-17A (50 ng/ml), TNFα (2 ng/ml) or both for 4 h (means of technical triplicates). b Protein levels of secreted G-CSF from HDMEC challenged with IL-17A (50 ng/ml), TNFα (2 ng/ml) or both for 24 h. c Relative mRNA levels of GROα in HDMEC challenged with IL-17A (50 ng/ml), TNFα (10 ng/ml) or both for 4 h (means of technical triplicates). d Protein levels of secreted GROα from HDMEC challenged with IL-17A (50 ng/ml), TNFα (10 ng/ml) or both for 12 h. e Protein levels of secreted IL-8 from HDMEC challenged with IL-17A (50 ng/ml), TNFα (10 ng/ml) or both for 24 h. f Protein levels of secreted CXCL10 from HDMEC challenged with IL-17A (50 ng/ml), TNFα (10 ng/ml) or both for 24 h. CXCL10 was undetectable in the CTR- and IL-17A-treated samples. b, d, e and f are representative of two independent experiments
Chemokines are cytokines which act as chemoattractants facilitating leukocyte adhesion and migration across the endothelium [45]. We therefore investigated if some of the chemokines previously reported to be regulated by IL-17A would also be regulated in HDMEC. IL-17A caused an up-regulation of GROα mRNA expression and protein secretion albeit to a lesser extent than TNFα (Fig. 2c, d). However, when the cells were challenged with IL-17A together with TNFα, GROα production rose to levels higher than those seen when stimulating with either alone (Fig. 2c, d). Similar results were obtained using HUVEC as analysed by qRT-PCR (data not shown). TNFα was also a potent inducer of GRO-γ (CXCL3) mRNA expression which, like GROα, could be further enhanced in combination with IL-17A (Table 2). Among the cytokines tested in this study, IL-17A seems specific for GRO-family chemokine secretion as levels of other chemokines such as CXCL10, CXCL11 and MCP-1 were not affected (Fig. 2f and Table 2) albeit potently induced by TNFα (Fig. 2f and data not shown). Interestingly, the expression of IL-8, which has previously been reported to be regulated by IL-17A in endothelial cells [39] and which is similar to GRO-family chemokines in terms of structure and function, was not significantly affected by IL-17A in HDMEC (Fig. 2e).
IL-17A potentiates TNFα-induced E-selectin and ICAM-1 expression
Adhesion molecules such as E-selectin, ICAM-1 and VCAM-1 on the surface of the endothelium mediate attachment and transmigration of circulating leukocytes, facilitating their recruitment to extravascular tissues [45]. We therefore investigated if IL-17A could modulate the expression of these molecules. When HDMEC were challenged with TNFα in combination with IL-17A, E-selectin levels were significantly augmented between 8 and 32 h of stimulation as compared to treatment with TNFα alone (Fig. 3a). After 32 h, levels of E-selectin were still significantly elevated compared to untreated cells (in which E-selectin was undetectable) and were approximately twofold higher in the presence of TNFα + IL-17A than in the presence of TNFα alone (Fig. 3a). We measured increased mRNA expressions for E-selectin between 4 and 24 h following TNFα stimulation that was further enhanced in the presence of IL-17 after 15–24 h (data not shown). The fold change of mRNA for a number of proteins as well as significance levels is shown in Table 2. These data are consistent with the finding that IL-17 enhances E-selectin expression in the presence of TNFα on the protein level as shown in Fig. 3a. mRNA for the other important cell adhesion protein P-selectin did not show any up-regulated expression between 4 and 24 h when stimulated with TNFα with or without IL-17A (data not shown). Furthermore, Western blotting of P-selectin did not show any change in protein expression following IL-17A stimulation that is neither the full-length nor the soluble P-selectin isoform (data not shown).
IL-17A modulates TNFα-induced E-selectin and ICAM-1 expression. a ELISA data showing cell-associated (lysate) protein levels of E-selectin in HDMEC when challenged with TNFα (2 ng/ml) or TNFα in combination with IL-17A (100 ng/ml) for 2–32 h. The effect of IL-17A was statistically significant at all time-points (P < 0.05) except at “4 h”. b Same as in a only for VCAM-1 protein. The effect of IL-17A was statistically significant at all time-points (P < 0.05) except at “4” and “32 h”. c Same as in a only for ICAM-1 protein. The effect of IL-17A was only statistically significant at “24 h” (P < 0.05). a, b and c are representative of two independent experiments
Levels of TNFα-induced VCAM-1 were unaffected except for a slight decrease after 24 h (Fig. 3b). The results were confirmed at the mRNA level by qRT-PCR (Table 2). Furthermore, IL-17A also augmented TNFα-induced ICAM-1 albeit to a modest extent (Fig. 3c). Untreated HDMEC expressed very low levels of adhesion molecules which could be modulated in the presence of IL-17A alone (data not shown). However, these effects were negligible in terms of potency compared to those of TNFα or TNFα + IL-17A.
It is not yet well documented how the synergistic effect between IL-17A and TNFα takes place, but it has been suggested that the mRNA stabilizing effects of Il-17A could play a role. In addition, the effect of activation of enhancer binding proteins (C/EBP) could be important as it has been shown in relation to IL-6 synthesis [40].
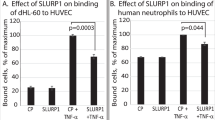
Elevated E-selectin levels by IL-17A correlate with increased leukocyte adhesion
E-selectin is crucial in the binding of leukocyte to the endothelium, and studies have shown that neutrophilic cells bind to endothelial cells in an E-selectin dependent manner [5, 30, 47]. We therefore investigated if the potentiating effect of IL-17A on TNFα-induced E-selectin expression correlated with increased neutrophil adhesion. After 30 h of stimulation, the effect of TNFα + IL-17A was maximal relative to TNFα alone, and we therefore chose to investigate adhesion at this time-point. Figure 4a, b shows that IL-17A is able to significantly augment TNFα-stimulated adhesion of neutrophils to an HDMEC monolayer in a manner which mirrored the observed effect on E-selectin expression (Fig. 3a). The design of the experiments was such that neutrophils were at no point exposed to IL-17A or TNFα and the adhesion therefore solely reflects the change in expression pattern and behaviour of the endothelial cells. To investigate the specificity of the E-selectin effect on adhesion, we applied E-selectin and P-selectin blocking antibodies to HDMEC monolayers pre-treated with either IL-17A, TNFα or both for 24 h. E-selectin or P-selectin blocking antibodies were added 1 h before the addition of neutrophils. The data reveal that the E-selectin antibody significantly reduces the binding of neutrophils to the endothelial cells when pre-stimulated with TNFα or TNFα + IL-17A. P-selectin antibodies had no effects on adhesion. These data reveal that E-selectin expression plays a dominant role in the neutrophil adhesion and thus is one of the important factors for controlling the rate of passage across the endothelial cell layer as seen in Fig. 4c.
IL-17A modulates TNFα-induced neutrophil adhesion and transmigration. a ELISA data showing cell-associated (lysate) protein levels of E-selectin in HDMEC when challenged with IL-17A (50 ng/ml), TNFα (1 ng/ml) or both for 24 h. b Relative number of neutrophils adhering to a confluent HDMEC monolayer pre-treated with either IL-17A (100 ng/ml), TNFα (2 ng/ml) or both for 30 h. c Relative number of neutrophils that had transmigrated through a confluent HDMEC monolayer pre-treated with either IL-17A (100 ng/ml), TNFα (2 ng/ml) or both for 30 h. a, b and c are representative of two independent experiments. d Relative number of neutrophils adhering to a confluent HDMEC monolayer pre-treated with either IL-17A (100 ng/ml), TNFα (2 ng/ml) or both for 24 h. The cells were pre-treated with 25 μg/ml E-selectin or 1 μg/ml P-selectin blocking antibodies for 1 h before the addition of neutrophils. e Photos of transmigrated neutrophils from c revealing the shape changes induced by TNFα with IL-17A
IL-17A causes increased neutrophil transmigration across an endothelial cell layer
Migration of neutrophils across the capillary wall is an important part of the inflammatory process that occurs after leukocytes have attached to the endothelium. E-selectin is essential in this context because it mediates the capturing of circulating leukocytes, causing them to roll along the endothelium. This, in turn, triggers integrins on their surface to interact with ICAM-1 and/or VCAM-1 resulting in a firm adherence [49]. We therefore hypothesized that IL-17A would be able to augment TNFα-stimulated transmigration of neutrophils. The passage of neutrophils across the endothelium was assayed using a trans-well migration-based experimental setup with confluent HDMEC layers as a barrier on both sides of the insert wells. The endothelial cells were pre-stimulated, and the stimulators were subsequently removed by washing prior to the addition of neutrophils to the insert wells. When HDMEC had been challenged with TNFα, the number of transmigrating neutrophils rose significantly above control, and this effect could be further enhanced when TNFα had been present together with IL-17A (Fig. 4c). When neutrophils were visualized after passage, they appeared round and were loosely attached to the barrier in control and IL-17A-stimulated conditions. When TNFα alone or in combination with IL-17A had been present, neutrophils (clearly) changed morphology after passage and adhered firmly to the endothelial surface with a large surface area (Fig. 4e). Thus, under conditions of potentiated E-selectin expression by IL-17A and TNFα in combination, we observed an enhanced transmigration of neutrophils across a confluent HDMEC layer.
IL-17A does not directly affect neutrophil activation
In the adhesion and migration experiments, neutrophils were not exposed to TNFα or IL-17A. In this way, we could investigate the endothelial cell-mediated effect on neutrophil adhesion and migration without interference from potential activating effects of IL-17A directly on the neutrophils. To investigate if IL-17A had such a direct effect, we established a monoculture adhesion assay in which the neutrophils were allowed to adhere to a fibrinogen substratum in the presence of IL-17A. Several cytokines including IL-8 and TNFα have previously been reported to induce and/or potentiate/prime neutrophil activation as measured by their ability to adhere to matrix proteins and/or generate superoxide radicals [11, 20, 53]. However, IL-17A was not able to induce adherence or generation of superoxide in neutrophils, nor was it able to prime/augment the effect of PMA and fMLP (Fig. 5a, b).
IL-17A does not directly affect neutrophil adherence and function. a Data showing neutrophil adherence to a fibrinogen substratum when challenged with IL-17A (50 ng/ml) or fMLP (1 μM) for 30 min. b Data showing neutrophil superoxide radical generation, as measured by reduction of ferricytochrome C, when challenged with IL-17A (50 ng/ml), fMLP (1 μM), PMA (10 ng/ml) or combinations of these
Discussion
In this study, we report that IL-17A in synchrony with TNFα potently induces endothelial cells to secrete chemokines important for mobilization and recruitment of neutrophils and up-regulates proteins that serve as binding sites during their passage through the endothelial barrier.
Stimulation of HDMEC with IL-17A caused enhanced p38 phosphorylation, which, however, was much smaller than that observed in the presence of TNFα (Fig. 1c, d). TNFα with and without IL-17A caused phosphorylation of IκBα and subsequently phosphorylation of NFκB that has a binding site in the human E-selectin gene [41]. This is consistent with the augmented E-selectin synthesis observed on the protein level (Fig. 3a).
Expression of E-selectin and P-selectin
The inducible expression of P-selectin and E-selectin is regulating inflammation, but their expression is mediated through different pathways. In human endothelial cells, E-selectin is encoded by the SELE gene that requires binding of NFκB and the activating transcription factor -2 (ATF-2) [29]. E-selectin is not stored in vesicles in the cell, but mRNA is translated and protein is transported to the cell surface. In human endothelial cells, P-selectin is upon thrombin and histamine stimulation mobilized from storage granules to the plasma membrane. However, mRNA synthesis for P-selectin in human endothelial cells is encoded by the Selp gene that lacks binding sites for NFκB and ATF-2, and mRNA synthesis is not activated by TNFα but by IL-4 [54].We found that E-selectin mRNA is increased several fold between 4 and 16 h with TNFα + IL-17A compared to unstimulated cells and that P-selectin mRNA is not increased, which are all consistent with the finding that different pathways are involved in their expressions. It is thus important to note that caution should be taken in comparing inflammatory mouse and human models due to the fact that P-selectin is expressed differently as pointed out by Liu et al. [29].
Secretion of chemokines
Endothelial stimulation with IL-17A caused a significant rise in the production of G-CSF and GROα consistent with previous observations in other cell types [13, 51]. IL-17A also caused an up-regulation of GRO-γ as shown by qRT-PCR (Table 2), a chemokine which is believed to have effects similar to GROα, i.e. function as a chemoattractant and a maturation factor specific for neutrophils [1, 14, 48]. Interestingly, we show that IL-8, another neutrophil-specific chemokine, is not significantly regulated by IL-17A in HDMEC, although this has been reported to be the case in human lung microvascular endothelial cells [39]. Neutrophils possess two receptors for IL-8 (CXCR1 and CXCR2), whereas GRO-family chemokines can only bind CXCR2 [1]. It has been shown that IL-8 efficiently triggers all aspects of neutrophil activation including shape change, chemotaxis, granule release and respiratory burst, i.e. generation of reactive oxygen species [4]. GRO-family chemokines, however, are significantly weaker activators of neutrophils in terms of both efficiency and efficacy when compared to IL-8 [17, 26]. It is possible that IL-17A regulates neutrophil recruitment and subsequent activation by orchestrating a local chemokine environment, the composition of which differs depending on the nature of the tissue and/or organ affected. Thus, appropriate attraction and activation of neutrophils in the lungs, by virtue of the respiratory microvascular endothelium, may require a distinct chemokine profile different from that of the dermal microvascular endothelium reflecting dissimilarities between the two tissues in terms of architecture, cellular environment and external exposure. The differences in neutrophil-activating properties between IL-8 and GRO-family chemokines could be of central importance in this context and would provide an adequate explanation as to why IL-17A seems to mediate cytokine expression profiles that differ between cell types. In support of this notion, we observed that IL-17A had no effect on the expression of non-neutrophil-specific chemokines such as CXCL10, CXCL11 and MCP-1 in HDMEC, although IL-17A has been reported to modulate both basal and TNFα-induced expression of these chemokines in other cell types [27, 34].
Neutrophil adhesion
Selectins (P-selectin and E-selectin) are the first adhesion molecules to interact with circulating leukocytes and allow leukocyte chemokine receptors to engage their ligands presented on the endothelium surface. This, in turn, triggers a more firm adhesion facilitated by ICAM-1 and VCAM-1. E-selectin is a “promiscuous” molecule in the sense that it can interact with all major types of leukocytes [6, 18, 28]. Which of these are then allowed to adhere firmly and subsequently extravasate is determined by the specific nature of the chemokines presented (neutrophil recruiting, e.g. GROα, or non-neutrophil recruiting, e.g. CXCL10). VCAM-1, however, can only interact with non-neutrophil leukocytes as its counter receptor VLA-4α is not expressed on human neutrophils but is expressed on human eosinophils and basophils [6]. We found that in HDMEC, IL-17A only affects the expression of cytokines specifically involved in controlling neutrophil recruitment. Furthermore, an investigation of HDMEC adhesion molecule expression revealed that IL-17A does not augment TNFα-induced VCAM-1 (Fig. 3b). These data are consistent with IL-17A being neutrophil specific since these cells cannot engage VCAM-1. In fact, our data show that on both the mRNA and protein levels, VCAM-1 is slightly down-regulated after 24 h of stimulation (Table 2). In contrast, we here show that IL-17A significantly potentiates TNFα-stimulated E-selectin expression, whereas levels of ICAM-1 are only slightly augmented in comparison. Taken together, our results are in agreement with the notion that in HDMEC, IL-17A only regulates factors controlling neutrophil biology.
It has previously been shown that E-selectin levels in HDMEC directly correlate with the number of adhering neutrophilic cells [43]. Moreover, both E-selectin and ICAM-1 are necessary for cytokine-stimulated transmigration of neutrophils to occur, as shown by studies using blocking antibodies directed against these adhesion molecules [31, 52]. We here show that the IL-17A-mediated potentiation of TNFα-induced E-selectin expression correlates with an equally increased ability of human neutrophils to adhere to an HDMEC monolayer (Fig. 4a, b). Furthermore, our data revealed a significant increase in neutrophil passage albeit not to an extent which matched its effect on neutrophil adhesion. It was recently shown in a mouse endothelial cell model that IL-17A and TNFα act in a synergistic manner to induce an endothelial cell activation and that neutrophil migration is mediated by its CXCR2 expression [19]. We found that a P-selectin-specific antibody did not affect the adherence of neutrophils to endothelial cell monolayer after 24-h stimulation with TNFα + IL-17A contrary to the effect of an antibody against E-selectin (Fig. 4d). We interpret this finding as being due to the high E-selectin expression on the endothelial cell surface compared to P-selectin. Cells had not been exposed to agonists such as thrombin or histamine that promotes transfer of P-selectin to the plasma membrane.
We have used a static system (no simulation of blood flow) to assay the transmigration potential of neutrophils resting on a confluent monolayer of HDMEC. Therefore, initial establishment of contact between neutrophils and endothelial cells did not, to the same extent, depend on E-selectin-mediated “stickiness” as it does in vivo. Given that neutrophil transmigration downstream of E-selectin depends on ICAM-1 and given that IL-17A only had a modest effect on the expression of this protein as compared to E-selectin, our system could not be expected to reveal the true potential of IL-17A in the recruitment of neutrophils as could be expected under in vivo conditions.
We found that IL-17A alone had no effect on neutrophil activation as measured by their ability to adhere to a fibrinogen substratum and their generation of superoxide radicals. These data are in agreement with the finding that only IL-17RA is present on neutrophils. We could not detect expression of IL-17RC transcripts using reverse-transcribed neutrophil total RNA, despite the fact that the IL-17RC-specific primers used were designed to allow amplification of all known splice variants. An IL-17RA transcript was, however, readily detectable.
The cooperative and synergistic actions on TNFα-induced secretion of neutrophil-specific cytokines, together with the ability to prolong TNFα-induced E-selectin expression as shown here, are likely to be mechanisms by which IL-17A causes an enhanced recruitment of neutrophils to sites of inflammation. Thus, we have shown that IL-17A controls mediators of leukocyte trafficking in a highly specific and selective manner via the microvascular endothelium in interaction with TNFα. The importance of IL-17A is thus seen when cellular effects are studied in cooperation with other pro-inflammatory cytokines.
References
Ahuja SK, Murphy PM (1996) The CXC chemokines growth-regulated oncogene (GRO) alpha, GRObeta, GROgamma, neutrophil-activating peptide-2, and epithelial cell-derived neutrophil-activating peptide-78 are potent agonists for the type B, but not the type A, human interleukin-8 receptor. J Biol Chem 271:20545–20550
Andoh A, Takaya H, Makino J, Sato H, Bamba S, Araki Y, Hata K, Shimada M, Okuno T, Fujiyama Y, Bamba T (2001) Cooperation of interleukin-17 and interferon-gamma on chemokine secretion in human fetal intestinal epithelial cells. Clin Exp Immunol 125:56–63
Awane M, Andres PG, Li DJ, Reinecker HC (1999) NF-kappa B-inducing kinase is a common mediator of IL-17-, TNF-alpha-, and IL-1 beta-induced chemokine promoter activation in intestinal epithelial cells. J Immunol 162:5337–5344
Baggiolini M, Clark-Lewis I (1992) Interleukin-8, a chemotactic and inflammatory cytokine. FEBS Lett 307:97–101
Benjamin C, Dougas I, Chi-Rosso G, Luhowskyj S, Rosa M, Newman B, Osborn L, Vassallo C, Hession C, Goelz S (1990) A blocking monoclonal antibody to endothelial-leukocyte adhesion molecule-1 (ELAM1). Biochem Biophys Res Commun 171:348–353
Bochner BS, Luscinskas FW, Gimbrone MA Jr, Newman W, Sterbinsky SA, Derse-Anthony CP, Klunk D, Schleimer RP (1991) Adhesion of human basophils, eosinophils, and neutrophils to interleukin 1-activated human vascular endothelial cells: contributions of endothelial cell adhesion molecules. J Exp Med 173:1553–1557
Cannistra SA, Griffin JD (1988) Regulation of the production and function of granulocytes and monocytes. Semin Hematol 25:173–188
Chabaud M, Fossiez F, Taupin JL, Miossec P (1998) Enhancing effect of IL-17 on IL-1-induced IL-6 and leukemia inhibitory factor production by rheumatoid arthritis synoviocytes and its regulation by Th2 cytokines. J Immunol 161:409–414
Chabaud M, Page G, Miossec P (2001) Enhancing effect of IL-1, IL-17, and TNF-alpha on macrophage inflammatory protein-3alpha production in rheumatoid arthritis: regulation by soluble receptors and Th2 cytokines. J Immunol 167:6015–6020
Dudas PL, Sague SL, Elloso MM, Farrell FX (2011) Proinflammatory/profibrotic effects of interleukin-17A on human proximal tubule epithelium. Nephron Exp Nephrol 117:e114–e123
Elbim C, Guichard C, Dang PM, Fay M, Pedruzzi E, Demur H, Pouzet C, El BJ, Gougerot-Pocidalo MA (2005) Interleukin-18 primes the oxidative burst of neutrophils in response to formyl-peptides: role of cytochrome b558 translocation and N-formyl peptide receptor endocytosis. Clin Diagn Lab Immunol 12:436–446
Eriksson A, Cao R, Roy J, Tritsaris K, Wahlestedt C, Dissing S, Thyberg J, Cao Y (2003) Small GTP-binding protein Rac is an essential mediator of vascular endothelial growth factor-induced endothelial fenestrations and vascular permeability. Circulation 107:1532–1538
Fossiez F, Djossou O, Chomarat P, Flores-Romo L, Ait-Yahia S, Maat C, Pin JJ, Garrone P, Garcia E, Saeland S, Blanchard D, Gaillard C, Das MB, Rouvier E, Golstein P, Banchereau J, Lebecque S (1996) T cell interleukin-17 induces stromal cells to produce proinflammatory and hematopoietic cytokines. J Exp Med 183:2593–2603
Fox SE, Lu W, Maheshwari A, Christensen RD, Calhoun DA (2005) The effects and comparative differences of neutrophil specific chemokines on neutrophil chemotaxis of the neonate. Cytokine 29:135–140
Fujino S, Andoh A, Bamba S, Ogawa A, Hata K, Araki Y, Bamba T, Fujiyama Y (2003) Increased expression of interleukin 17 in inflammatory bowel disease. Gut 52:65–70
Gaffen SL (2008) An overview of IL-17 function and signaling. Cytokine 43:402–407
Geiser T, Dewald B, Ehrengruber MU, Clark-Lewis I, Baggiolini M (1993) The interleukin-8-related chemotactic cytokines GRO alpha, GRO beta, and GRO gamma activate human neutrophil and basophil leukocytes. J Biol Chem 268:15419–15424
Graber N, Gopal TV, Wilson D, Beall LD, Polte T, Newman W (1990) T cells bind to cytokine-activated endothelial cells via a novel, inducible sialoglycoprotein and endothelial leukocyte adhesion molecule-1. J Immunol 145:819–830
Griffin GK, Newton G, Tarrio ML, Bu DX, Maganto-Garcia E, Azcutia V, Alcaide P, Grabie N, Luscinskas FW, Croce KJ, Lichtman AH (2012) IL-17 and TNF-alpha sustain neutrophil recruitment during inflammation through synergistic effects on endothelial activation. J Immunol 188:6287–6299
Guichard C, Pedruzzi E, Dewas C, Fay M, Pouzet C, Bens M, Vandewalle A, Ogier-Denis E, Gougerot-Pocidalo MA, Elbim C (2005) Interleukin-8-induced priming of neutrophil oxidative burst requires sequential recruitment of NADPH oxidase components into lipid rafts. J Biol Chem 280:37021–37032
Hammer T, Tritsaris K, Hubschmann MV, Gibson J, Nisato RE, Pepper MS, Dissing S (2009) IL-20 activates human lymphatic endothelial cells causing cell signalling and tube formation. Microvasc Res 78:25–32
Hirata T, Osuga Y, Takamura M, Kodama A, Hirota Y, Koga K, Yoshino O, Harada M, Takemura Y, Yano T, Taketani Y (2010) Recruitment of CCR6-expressing Th17 cells by CCL 20 secreted from IL-1 beta-, TNF-alpha-, and IL-17A-stimulated endometriotic stromal cells. Endocrinology 151:5468–5476
Iwakura Y, Nakae S, Saijo S, Ishigame H (2008) The roles of IL-17A in inflammatory immune responses and host defense against pathogens. Immunol Rev 226:57–79
Kagami S (2011) IL-23 and Th17 cells in infections and psoriasis. Nihon Rinsho Meneki Gakkai Kaishi 34:13–19
Kolls JK, Linden A (2004) Interleukin-17 family members and inflammation. Immunity 21:467–476
L'Heureux GP, Bourgoin S, Jean N, McColl SR, Naccache PH (1995) Diverging signal transduction pathways activated by interleukin-8 and related chemokines in human neutrophils: interleukin-8, but not NAP-2 or GRO alpha, stimulates phospholipase D activity. Blood 85:522–531
Lee JW, Wang P, Kattah MG, Youssef S, Steinman L, DeFea K, Straus DS (2008) Differential regulation of chemokines by IL-17 in colonic epithelial cells. J Immunol 181:6536–6545
Leeuwenberg JF, Jeunhomme TM, Buurman WA (1992) Role of ELAM-1 in adhesion of monocytes to activated human endothelial cells. Scand J Immunol 35:335–341
Liu Z, Miner JJ, Yago T, Yao L, Lupu F, Xia L, McEver RP (2010) Differential regulation of human and murine P-selectin expression and function in vivo. J Exp Med 207:2975–2987
Luscinskas FW, Brock AF, Arnaout MA, Gimbrone MA Jr (1989) Endothelial-leukocyte adhesion molecule-1-dependent and leukocyte (CD11/CD18)-dependent mechanisms contribute to polymorphonuclear leukocyte adhesion to cytokine-activated human vascular endothelium. J Immunol 142:2257–2263
Luscinskas FW, Cybulsky MI, Kiely JM, Peckins CS, Davis VM, Gimbrone MA Jr (1991) Cytokine-activated human endothelial monolayers support enhanced neutrophil transmigration via a mechanism involving both endothelial-leukocyte adhesion molecule-1 and intercellular adhesion molecule-1. J Immunol 146:1617–1625
Moniaga CS, Egawa G, Doi H, Miyachi Y, Kabashima K (2011) Histamine modulates the responsiveness of keratinocytes to IL-17 and TNF-alpha through the H1-receptor. J Dermatol Sci 61:79–81
Moseley TA, Haudenschild DR, Rose L, Reddi AH (2003) Interleukin-17 family and IL-17 receptors. Cytokine Growth Factor Rev 14:155–174
Numasaki M, Lotze MT, Sasaki H (2004) Interleukin-17 augments tumor necrosis factor-alpha-induced elaboration of proangiogenic factors from fibroblasts. Immunol Lett 93:39–43
Onishi RM, Gaffen SL (2010) Interleukin-17 and its target genes: mechanisms of interleukin-17 function in disease. Immunology 129:311–321
Ouyang X, Yang Z, Zhang R, Arnaboldi P, Lu G, Li Q, Wang W, Zhang B, Cui M, Zhang H, Liang-Chen J, Qin L, Zheng F, Huang B, Xiong H (2011) Potentiation of Th17 cytokines in aging process contributes to the development of colitis. Cell Immunol 266:208–217
Pietrowski E, Bender B, Huppert J, White R, Luhmann HJ, Kuhlmann CR (2011) Pro-inflammatory effects of interleukin-17A on vascular smooth muscle cells involve NAD(P)H-oxidase derived reactive oxygen species. J Vasc Res 48:52–58
Rahman MS, Yamasaki A, Yang J, Shan L, Halayko AJ, Gounni AS (2006) IL-17A induces eotaxin-1/CC chemokine ligand 11 expression in human airway smooth muscle cells: role of MAPK (Erk1/2, JNK, and p38) pathways. J Immunol 177:4064–4071
Roussel L, Houle F, Chan C, Yao Y, Berube J, Olivenstein R, Martin JG, Huot J, Hamid Q, Ferri L, Rousseau S (2010) IL-17 promotes p38 MAPK-dependent endothelial activation enhancing neutrophil recruitment to sites of inflammation. J Immunol 184:4531–4537
Ruddy MJ, Wong GC, Liu XK, Yamamoto H, Kasayama S, Kirkwood KL, Gaffen SL (2004) Functional cooperation between interleukin-17 and tumor necrosis factor-alpha is mediated by CCAAT/enhancer-binding protein family members. J Biol Chem 279:2559–2567
Schindler U, Baichwal VR (1994) Three NF-kappa B binding sites in the human E-selectin gene required for maximal tumor necrosis factor alpha-induced expression. Mol Cell Biol 14:5820–5831
Schwarzenberger P, La RV, Miller A, Ye P, Huang W, Zieske A, Nelson S, Bagby GJ, Stoltz D, Mynatt RL, Spriggs M, Kolls JK (1998) IL-17 stimulates granulopoiesis in mice: use of an alternate, novel gene therapy-derived method for in vivo evaluation of cytokines. J Immunol 161:6383–6389
Sepp NT, Gille J, Li LJ, Caughman SW, Lawley TJ, Swerlick RA (1994) A factor in human plasma permits persistent expression of E-selectin by human endothelial cells. J Invest Dermatol 102:445–450
Shalom-Barak T, Quach J, Lotz M (1998) Interleukin-17-induced gene expression in articular chondrocytes is associated with activation of mitogen-activated protein kinases and NF-kappaB. J Biol Chem 273:27467–27473
Speyer CL, Ward PA (2011) Role of endothelial chemokines and their receptors during inflammation. J Invest Surg 24:18–27
Takahashi H, Tsuji H, Hashimoto Y, Ishida-Yamamoto A, Iizuka H (2010) Serum cytokines and growth factor levels in Japanese patients with psoriasis. Clin Exp Dermatol 35:645–649
Walter UM, Ayer LM, Manning AM, Frenette PS, Wagner DD, Hynes RO, Wolitzky BA, Issekutz AC (1997) Generation and characterization of a novel adhesion function blocking monoclonal antibody recognizing both rat and mouse E-selectin. Hybridoma 16:355–361
Wengner AM, Pitchford SC, Furze RC, Rankin SM (2008) The coordinated action of G-CSF and ELR + CXC chemokines in neutrophil mobilization during acute inflammation. Blood 111:42–49
Williams MR, Azcutia V, Newton G, Alcaide P and Luscinskas FW (2011) Emerging mechanisms of neutrophil recruitment across endothelium. Trends Immunol
Witowski J, Ksiazek K, Warnecke C, Kuzlan M, Korybalska K, Tayama H, Wisniewska-Elnur J, Pawlaczyk K, Trominska J, Breborowicz A, Jorres A (2007) Role of mesothelial cell-derived granulocyte colony-stimulating factor in interleukin-17-induced neutrophil accumulation in the peritoneum. Kidney Int 71:514–525
Witowski J, Pawlaczyk K, Breborowicz A, Scheuren A, Kuzlan-Pawlaczyk M, Wisniewska J, Polubinska A, Friess H, Gahl GM, Frei U, Jorres A (2000) IL-17 stimulates intraperitoneal neutrophil infiltration through the release of GRO alpha chemokine from mesothelial cells. J Immunol 165:5814–5821
Yan HC, DeLisser HM, Pilewski JM, Barone KM, Szklut PJ, Chang XJ, Ahern TJ, Langer-Safer P, Albelda SM (1994) Leukocyte recruitment into human skin transplanted onto severe combined immunodeficient mice induced by TNF-alpha is dependent on E-selectin. J Immunol 152:3053–3063
Yan SR, Novak MJ (1999) Diverse effects of neutrophil integrin occupation on respiratory burst activation. Cell Immunol 195:119–126
Yao L, Pan J, Setiadi H, Patel KD, McEver RP (1996) Interleukin 4 or oncostatin M induces a prolonged increase in P-selectin mRNA and protein in human endothelial cells. J Exp Med 184:81–92
Ye P, Rodriguez FH, Kanaly S, Stocking KL, Schurr J, Schwarzenberger P, Oliver P, Huang W, Zhang P, Zhang J, Shellito JE, Bagby GJ, Nelson S, Charrier K, Peschon JJ, Kolls JK (2001) Requirement of interleukin 17 receptor signaling for lung CXC chemokine and granulocyte colony-stimulating factor expression, neutrophil recruitment, and host defense. J Exp Med 194:519–527
Yu JJ, Gaffen SL (2008) Interleukin-17: a novel inflammatory cytokine that bridges innate and adaptive immunity. Front Biosci 13:170–177
Acknowledgments
We are grateful to Wid Talal and Charlotte Therland for the expert technical assistance. This work was supported by Nordea Fonden, NOVO Nordisk Fonden and Center for Healthy Aging (Nordea Fonden).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Bosteen, M.H., Tritsaris, K., Hansen, A.J. et al. IL-17A potentiates TNFα-induced secretion from human endothelial cells and alters barrier functions controlling neutrophils rights of passage. Pflugers Arch - Eur J Physiol 466, 961–972 (2014). https://doi.org/10.1007/s00424-013-1354-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-013-1354-5