Abstract
Purpose
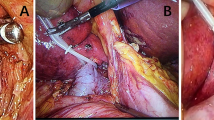
Uncontrollable bleeding remained problematic in anatomical hepatectomy exposing hepatic veins. Based on the inferior vena cava (IVC) anatomy, we attempted to analyze the hemodynamic and surgical effects of the combined IVC-partial clamp (PC) accompanied with the Trendelenburg position (TP).
Methods
We prospectively assessed 26 consecutive patients who underwent anatomical hepatectomies exposing HV trunks between 2020 and 2023. Patients were divided into three groups: use of IVC-PC (group 1), no use of IVC-PC (group 2), and use of IVC-PC accompanied with TP (group 3). In 10 of 26 patients (38%), hepatic venous pressure was examined using transhepatic catheter insertion.
Results
IVC-PC was performed in 15 patients (58%). Operating time and procedures did not significantly differ between groups. A direct hemostatic effect on hepatic veins was evaluated in 60% and 70% of patients in groups 1 and 3, respectively. Group 1 showed significantly more unstable vital status and vasopressor use (p < 0.01). Blood or fluid transfusion and urinary output were similar between groups. Group 2 had a significantly lower baseline central venous pressure (CVP), while group 3 showed a significant increase in CVP in TP. CVP under IVC-PC seemed lower than under TP; however, not significantly. Hepatic venous pressure did not significantly differ between groups. Systolic arterial blood pressure significantly decreased via IVC-PC in group 1 and to a similar extent in group 3. Heart rate significantly increased during IVC-PC (p < 0.05).
Conclusion
IVC-PC combined with the TP may be an alternative procedure to control intrahepatic venous bleeding during anatomical hepatectomy exposing hepatic venous trunks.
Similar content being viewed by others
Data availability
The data that support the findings of this study are available in public.
References
Moris D, Tsilimigras DI, Kostakis ID et al (2018) Anatomic versus non-anatomic resection for hepatocellular carcinoma: a systematic review and meta-analysis. Eur J Surg Oncol 44:927–938
Walcott-Sapp S, Billingsley KG (2018) Preoperative optimization for major hepatic resection. Langenbecks Arch Surg 403:23–35
Kokudo N, Takemura N, Ito K, Mihara F (2020) The history of liver surgery: achievements over the past 50 years. Ann Gastroenterol Surg 4:109–117
Nanashima A, Sumida Y, Abo T et al (2008) Principle of perioperative management for hepatic resection and education for young surgeons. Hepatogastroenterol 55:587–591
Rahbari NN, Garden OJ, Padbury R et al (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149:713–724
Latchana N, Hirpara DH, Hallet J, Karanicolas PJ (2019) Red blood cell transfusion in liver resection. Langenbecks Arch Surg 404:1–9
Houben P, Hinz U, Knebel P, Diener MK, Mehrabi A, Schemmer P (2019) Randomized controlled trial on Pringle Maneuver to reduce blood loss during stapler hepatectomy-PriMal StHep. BMC Surg 19:60
Melendez JA, Arslan V, Fischer ME et al (1998) Perioperative outcomes of major hepatic resections under low central venous pressure anesthesia: blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg 187:620–625
Jones RM, Moulton CE, Hardy KJ (1998) Central venous pressure and its effect on blood loss during liver resection. Br J Surg 85:1058–1060
Li Z, Sun YM, Wu FX, Yang LQ, Lu ZJ, Yu WF (2014) Controlled low central venous pressure reduces blood loss and transfusion requirements in hepatectomy. World J Gastroenterol 20(1):303–309
Hughes MJ, Ventham NT, Harrison EM, Wigmore SJ (2015) Central venous pressure and liver resection: a systematic review and meta-analysis. HPB (Oxford) 17(10):863–871
Nanashima A, Tanoue Y, Sakae T et al (2021) Relationship between hepatic venous anatomy and hepatic venous blood loss during hepatectomy. Surg Today 51(12):1953–1968
Okuno A, Kimura F, Nakagawa K et al (2010) Effects of partial hepatic venous congestion on hepatic hemodynamics and histology. Hepatogastroenterol 57:127–133
Otsubo T, Takasaki K, Yamamoto M et al (2004) Bleeding during hepatectomy can be reduced by clamping the inferior vena cava below the liver. Surgery 135(1):67–73
Ueno M, Kawai M, Hayami S et al (2017) Partial clamping of the infrahepatic inferior vena cava for blood loss reduction during anatomic liver resection: a prospective, randomized, controlled trial. Surgery 161:1502–1513
Rahbari NN, Koch M, Mehrabi A et al (2009) Portal triad clamping versus vascular exclusion for vascular control during hepatic resection: a systematic review and meta-analysis. J Gastrointest Surg 13(3):558–568
Xiao LK, Huang P, Wu K et al (2021) Effect of infrahepatic inferior vena cava partial clamping on central venous pressure and intraoperative blood loss during laparoscopic hepatectomy. Surg Endosc 35:2773–2780
Imamura T, Yamamoto Y, Sugiura T et al (2019) Infrahepatic inferior vena cava semi-clamping can reduce blood loss during hepatic resection but still requires monitoring to avoid acute kidney injury. World J Surg 43:2038–2047
Rahbari NN, Koch M, Zimmermann JB et al (2011) Infrahepatic inferior vena cava clamping for reduction of central venous pressure and blood loss during hepatic resection: a randomized controlled trial. Ann Surg 253:1102–1110
Junrungsee S, Suwannikom K, Tiyaprasertkul W et al (2021) Efficacy and safety of infrahepatic inferior vena cava clamping under controlled central venous pressure for reducing blood loss during hepatectomy: a randomized controlled trial. J Hepatobiliary Pancreat Sci 28:604–616
Jaffurs W Jr, Spicer SS, Carroll RG, Allison EJ Jr, Whitley TW, Mayo HL (1989) Transcutaneous oxygen tension measurements during hemorrhagic hypoperfusion using Trendelenburg and the pneumatic antishock garment. Resuscitation 17:119–129
Nanashima A, Tobinaga S, Abo T, Nonaka T, Sawai T, Nagayasu T (2010) Usefulness of the combination procedure of crash clamping and vessel sealing for hepatic resection. J Surg Oncol 102:179–183
Takasaki T, Kobayashi S, Suzuki S et al (1980) Predetermining postoperative hepatic function for hepatectomies. Int Surg 65:309–313
Kubota K, Makuuchi M, Kusaka K et al (1997) Measurement of liver volume and hepatic functional reserve as a guide to decision-making in resection surgery for hepatic tumors. Hepatology 26:1176–1181
Yamaguchi H, Nanashima A, Hatano K et al (1998) Safety of repeated total hepatic inflow occlusion during liver resection. (in Japanese with English title and abstract) Kanzo 39:812–819. https://doi.org/10.2957/kanzo.39.812
Brooke-Smith M, Figueras J, Ullah S, Rees M et al (2015) Prospective evaluation of the International Study Group for Liver Surgery definition of bile leak after a liver resection and the role of routine operative drainage: an international multicentre study. HPB(Oxford) 17:46–51
Hughes MJ, Ventham NT, Harrison EM, Wigmore SJ (2015) Central venous pressure and liver resection: a systematic review and meta-analysis. HPB (Oxford) 17:863–871
Yoneda G, Katagiri S, Yamamoto M (2015) Reverse Trendelenburg position is a safer technique for lowering central venous pressure without decreasing blood pressure than clamping of the inferior vena cava below the liver. J Hepatobiliary Pancreat Sci 22:463–436
Gan EC, Habib AR, Rajwani A, Javer AR (2014) Five-degree, 10-degree, and 20-degree reverse Trendelenburg position during functional endoscopic sinus surgery: a double-blind randomized controlled trial. Int Forum Allergy Rhinol 4:61–68
Soonawalla ZF, Stratopoulos C, Stoneham M, Wilkinson D, Britton BJ, Friend PJ (2008) Role of the reverse-Trendelenberg patient position in maintaining low-CVP anaesthesia during liver resections. Langenbecks Arch Surg 393:195–198
De Backer D, Vincent JL (2018) Should we measure the central venous pressure to guide fluid management? Ten answers to 10 questions. Crit Care 22:43
Behem CR, Grassler MF, Trepte CJC (2018) Central venous pressure in liver surgery: a primary therapeutic goal or a hemodynamic tessera? Anaesthesist 67:780–789
Lau WY, Lai EC, Lau SH (2010) Methods of vascular control technique during liver resection: a comprehensive review. Hepatobiliary Pancreat Dis Int 9:473–481
van Gulik TM, de Graaf W, Dinant S, Busch OR, Gouma DJ (2007) Vascular occlusion techniques during liver resection. Dig Surg 24:274–281
Makuuchi M, Yamamoto J, Takayama T et al (1991) Extrahepatic division of the right hepatic vein in hepatectomy. Hepatogastroenterol 38:176–179
Lakhal K, Ehrmann S, Runge I et al (2010) Central venous pressure measurements improve the accuracy of leg raising-induced change in pulse pressure to predict fluid responsiveness. Intensive Care Med 36:940–948
Satterly SA, Salgar S, Hoffer Z et al (2015) Hydrogen sulfide improves resuscitation via non-hibernatory mechanisms in a porcine shock model. J Surg Res 199:197–210
Sakamoto K, Iwamoto Y, Ogawa K et al (2023) Impact of the inferior vena cava morphology on fluid dynamics of the hepatic veins. Surg Today. https://doi.org/10.1007/s00595-023-02733-6
Zhu P, Lau WY, Chen YF et al (2012) Randomized clinical trial comparing infrahepatic inferior vena cava clamping with low central venous pressure in complex liver resections involving the Pringle manoeuvre. Br J Surg 99:781–788
Sakamoto K, Ogawa K, Matsui T et al (2020) Vertical interval between hepatic segment of inferior vena cava and right atrium predicts intraoperative blood loss during hemi-hepatectomy. J Hepatobiliary Pancreat Sci 27:90–100
Tranchart H, O’Rourke N, Van Dam R et al (2015) Bleeding control during laparoscopic liver resection: a review of literature. J Hepatobiliary Pancreat Sci 22:371–378
Acknowledgements
The authors would like to thank Elsevier’s editing service for the English language review. Revised sentences were edited by another English editing service, FORTE Science Communications (No. R2304389 October 19th).
Funding
This study was supported by an institutional Grant-in-Aid for Clinical Research from Miyazaki University Hospital in 2022 (without reference number). English was edited by the Elsevier language service.
Author information
Authors and Affiliations
Contributions
All listed authors attended the prospective study project. Principle writing, study design making, paper writing, and all responsibility of study: AN; measurement, data collection, and patient management: MH, NI, TH, YT, IS, YO; support the circulatory management as a director of cardiovascular surgery: KF; instruction and anesthetic management as a director of anesthesia: IT.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nanashima, A., Hiyoshi, M., Imamura, N. et al. Measuring intraoperative anesthetic parameters during hepatectomy with inferior vena cava clamping. Langenbecks Arch Surg 408, 455 (2023). https://doi.org/10.1007/s00423-023-03172-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03172-0