Abstract
Introduction
Delayed coloanal anastomosis (DCAA) is a two-stage procedure. DCAA has been increasingly reused in recent years in the management of rectal cancer. Such increased use of DCAA has highlighted the complications associated with this procedure. We aimed to evaluate the risk and risk factors of ischemia/necrosis of the colonic stump between the two stages of DCAA.
Patients and methods
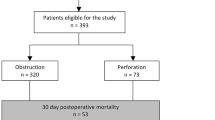
All patients who underwent a proctectomy with a DCAA were included in this retrospective single-centre study from November 2012 to June 2022. Two groups of patients were defined: patients with a well vascularized colonic stump (well vascularized group) and those who experienced ischemia or necrosis of the colonic stump (ischemic group). The primary endpoint was the rate of ischemia or necrosis of the colonic stump and an evaluation of the associated risk factors.
Results
During the study period, 43 patients underwent DCAA. Amongst them, 32 (75%) had a well-vascularized colonic stump (well-vascularized group) and 11 (25%) ischemia of the colonic stump (ischemic group). Relative to patients in the well-vascularized group, those in the ischemic group were more often men (81.8% vs 40.6%, p = 0.034), had a higher BMI (29.2 kg/m2 vs 25.7 kg/m2, p = 0.03), were more frequently diabetic (63.6% vs 21.9%, p = 0.01) and more frequently had had preoperative radiotherapy (100% vs 53.1%, p = 0.008). On the preoperative CT scan, the interspinous diameter was shorter in the ischemic group (9.4 ± 1.01 cm vs 10.6 ± 1.01 cm, p = 0.001), the intertuberosity diameter was shorter (9.2 ± 1.18 cm vs 11.9 ± 1.18 cm, p < 0.0001), and the length of the anal canal was longer (31.9 ± 3 mm vs 27.4 ± 3.2 mm, p < 0.0001).
Conclusion
This study highlights clear risk factors for ischemia/necrosis of the colonic stump after proctectomy with DCAA.




Similar content being viewed by others
Data availability
Data archiving is not mandated but data will be made available on reasonable request.
References
Cutait DE, Figliolini FJ (1961) A new method of colorectal anastomosis in abdominoperineal resection. Dis Colon Rectum 4:335–342
Turnbull RB, Cuthbertson A (1961) Abdominorectal pull-through resection for cancer and for Hirschsprung’s disease. Delayed posterior colorectal anastomosis. Cleve Clin Q 28:109–115
Bianco F, Belli A, De Franciscis S, Falato A, Romano GM (2016) “Scarless” and no-stoma surgery for low rectal cancer: the laparoscopic pull-through delayed “high” colo-anal anastomosis. Updates Surg 68(1):99–104
Baulieux J, Olagne E, Ducerf C, De La Roche E, Adham M, Berthoux N, Bourdeix O, Gérard JP (1999) Résultats oncologiques et fonctionnels des résections avec anastomose coloanale directe différée dans les cancers du bas rectum préalablement irradiés [Oncologic and functional results of resections with direct delayed coloanal anastomosis in previously irradiated cancers of the lower rectum]. Chirurgie 124(3):240–50. https://doi.org/10.1016/s0001-4001(99)80089-0
Wang Z (2021) Colonic J-pouch versus side-to-end anastomosis for rectal cancer: a systematic review and meta-analysis of randomized controlled trials. BMC Surg 21(1):331
Paun BC, Cassie S, MacLean AR, Dixon E, Buie WD (2010) Postoperative complications following surgery for rectal cancer. Ann Surg 251(5):807–818
Eriksen MT, Wibe A, Norstein J, Haffner J, Wiig JN, Group NRC (2005) Anastomotic leakage following routine mesorectal excision for rectal cancer in a national cohort of patients. Colorectal Dis 7(1):51–57
Bell SW, Walker KG, Rickard MJ, Sinclair G, Dent OF, Chapuis PH et al (2003) Anastomotic leakage after curative anterior resection results in a higher prevalence of local recurrence. Br J Surg 90(10):1261–1266
Hallet J, Milot H, Drolet S, Desrosiers E, Grégoire RC, Bouchard A (2014) The clinical results of the Turnbull-Cutait delayed coloanal anastomosis: a systematic review. Tech Coloproctol 18(6):579–590
Jarry J, Faucheron JL, Moreno W, Bellera CA, Evrard S (2011) Delayed colo-anal anastomosis is an alternative to prophylactic diverting stoma after total mesorectal excision for middle and low rectal carcinomas. Eur J Surg Oncol 37(2):127–133
Biondo S, Trenti L, Espin E, Bianco F, Barrios O, Falato A et al (2020) Two-stage Turnbull-Cutait pull-through coloanal anastomosis for low rectal cancer: a randomized clinical trial. JAMA Surg 155(8):e201625
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Beltzer C, Vetter M, Axt S, Bachmann R, Schmidt R (2020) Impact of bowel preparation on surgical site infections and anastomotic leakage after elective colon resection: results of a retrospective study with 260 patients. Chirurg 91(6):491–501
Son GM, Ahn HM, Lee IY, Lee SM, Park SH, Baek KR (2021) Clinical effect and standardization of indocyanine green angiography in the laparoscopic colorectal surgery. J Minim Invasive Surg 24(3):113–122
Zhou XC, Su M, Hu KQ, Su YF, Ye YH, Huang CQ et al (2016) CT pelvimetry and clinicopathological parameters in evaluation of the technical difficulties in performing open rectal surgery for mid-low rectal cancer. Oncol Lett 11(1):31–38
Danielsen AK, Park J, Jansen JE, Bock D, Skullman S, Wedin A et al (2017) Early closure of a temporary ileostomy in patients with rectal cancer: a multicenter randomized controlled trial. Ann Surg 265(2):284–290
Clausen FB, Dohrn N, Holmich ER, Klein M, Gogenur I (2021) Safety of early ileostomy closure: a systematic review and meta-analysis of randomized controlled trials. Int J Colorectal Dis 36(2):203–212
den Dulk M, Smit M, Peeters KC, Kranenbarg EM, Rutten HJ, Wiggers T et al (2007) A multivariate analysis of limiting factors for stoma reversal in patients with rectal cancer entered into the total mesorectal excision (TME) trial: a retrospective study. Lancet Oncol 8(4):297–303
Author information
Authors and Affiliations
Contributions
Jules Le Pessot, Alexandra Pellegrin, Jean-Marc Regimbeau and Charles Sabbagh state the following: (1) made substantial contributions to the conception or design of the work; or the acquisition, analysis or interpretation of data; or the creation of new software used in the work; (2) drafted the work or revised it critically for important intellectual content; (3) approved the version to be published; and (4) agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Le Pessot, J., Pellegrin, A., Regimbeau, JM. et al. Risk factors for ischemia/necrosis of the colonic stump after proctectomy and delayed coloanal anastomosis. Langenbecks Arch Surg 408, 424 (2023). https://doi.org/10.1007/s00423-023-03157-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03157-z