Abstract
Introduction
Fournier’s gangrene (FG) is a necrotizing fasciitis affecting the perineum and urogenital tissue. The mortality rate is high although early detection and aggressive debridement can reduce mortality by up to 16%. The prevalence of sequelae is very high and a colostomy is often necessary to control the perineal wound.
Material and methods
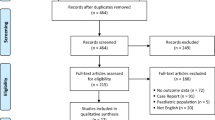
A retrospective study was carried out to recruit all patients operated on by the General Surgery and Urology Departments with a diagnosis of GF at the University Hospital over 22 years. Mortality, the Fournier gangrene severity index (FGSI), and fecal diversion (either surgical (colostomy) or straight (Flexi-seal)) are collected.
Results
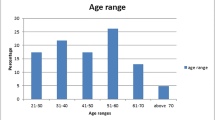
A total of 149 patients met the inclusion criteria. FG’s most frequent cause was a perianal abscess (107 patients—72%). Eighteen patients (12%) died of a specific cause of FG. Age (p = 0.014) and patients with an oncological history (p = 0.038) both were the only mortality risk factors for mortality according to logistic regression. Fifty patients required some form of fecal diversion in the postoperative period (32 colostomies and 18 Flexi-seal). Neither the use of postoperative fecal diversion (surgical or Flexi-seal) nor the timing of its use had any effect on postoperative mortality.
Conclusions
One in eight patients died in the immediate postoperative period secondary to FG. Despite improved outcomes, 22% required a colostomy during admission. However, neither the performance of a colostomy nor the timing was associated with decreased FG-associated mortality. Non-invasive methods should be used first and surgical bowel diversion should be postponed as long as possible.



Similar content being viewed by others
Data Availability
Data are available for consultation.
References
Laucks SS (1994) Fournier’s gangrene. Surg Clin North Am 74(6):1339–1352
Vick R, Carson CC (1999) Fournier’s disease. Urol Clin North Am 26(4):841–849
Tang LM, Su YJ, Lai YC (2015) The evaluation of microbiology and prognosis of Fournier’s gangrene in past five years. Springerplus 4(1):2013–2016
Provenzano D, Lo Bianco S, Zanghì M, Campione A, Vecchio R, Zanghì G (2021) Fournier’s gangrene as a rare complication in patient with uncontrolled type 2 diabetes treated with surgical debridement: a case report and literature review. Int J Surg Case Rep 79:462–465
Yoshino Y, Funahashi K, Okada R, Miura Y, Suzuki T, Koda T et al (2016) Severe Fournier’s gangrene in a patient with rectal cancer: case report and literature review. World J Surg Oncol 14(1):1–5
Singh A, Ahmed K, Aydin A, Khan MS, Dasgupta P (2016) Archivio italiano di urologia e andrologia Arch ital urol androl = Archives of Italian urology and andrology. Arch Ital di Urol e Androl 88(3):157–164
Sorensen MD, Krieger JN, Rivara FP, Broghammer JA, Klein MB, Mack CD et al (2009) Fournier’s gangrene: population based epidemiology and outcomes. J Urol 181(5):2120–2126
Carvalho JP, Hazan A, Cavalcanti AG, Favorito LA (2007) Relation between the area affected by Fournier’s gangrene and the type of reconstructive surgery used. A study with 80 patients. Int Braz J Urol. 33(4):510–4
Laor E, Palmer LS, Tolia BM, Reid RE, Winter HI (1995) Outcome prediction in patients with Fournier’s gangrene. J Urol 154(1):89–92
Lin TY, Ou CH, Tzai TS et al (2014) Validation and simplification of Fournier’s gangrene severity index. Int J Urol 21(7):696–701. https://doi.org/10.1111/iju.12426
Thwaini A, Khan A, Malik A et al (2006) Fournier’s gangrene and its emergency management. Postgrad Med J 82(970):516–519. https://doi.org/10.1136/pgmj.2005.042069
Eray IC, Alabaz O, Akcam AT et al (2015) Comparison of diverting colostomy and bowel management catheter applications in fournier gangrene cases requiring fecal diversion. Indian J Surg 77(Suppl 2):438–441. https://doi.org/10.1007/s12262-013-0868-6
Chen CS, Liu KL, Chen HW, Chou CC, Chuang CK, Chu SH (1999) Prognostic factors and strategy of treatment in Fournier’s gangrene: a 12-year retrospective study. Changgeng Yi Xue Za Zhi 22(1):31–36
Tosun Y, Akıncı O, Küçük HF (2022) Risk factors for mortality in Fournier’s gangrene of anorectal origin. Ulus Travma ve Acil Cerrahi Derg 28(8):1128–1133
Leslie SW, Rad J, Foreman J (2023) Fournier Gangrene. In: StatPearls. Treasure Island (FL): StatPearls Publishing
Şahin E, Erşen O, Mercan Ü, Yılmaz S (2022) The effect of Fournier gangrene severity index and microbial culture results on hospital length of stay, frequency of debridement, and mortality. Ulus Travma ve Acil Cerrahi Derg 28(2):155–161
Ozturk E, Sonmez Y, Yilmazlar T (2011) What are the indications for a stoma in Fournier’s gangrene? Colorectal Dis 13(9):1044–1047. https://doi.org/10.1111/j.1463-1318.2010.02353.x
Sarofim M, Di Re A, Descallar J, Toh JWT (2021) Relationship between diversional stoma and mortality rate in Fournier’s gangrene: a systematic review and meta-analysis. Langenbecks Arch Surg 406(8):2581–2590. https://doi.org/10.1007/s00423-021-02175-z
Rosen DR, Brown ME, Cologne KG, Ault GT, Strumwasser AM (2016) Long-term follow-up of Fournier’s gangrene in a tertiary care center. J Surg Res 206(1):175–181
Li Y-D, Zhu W-F, Qiao J-J, Lin J-J (2014) Enterostomy can decrease the mortality of patients with Fournier gangrene. World J Gastroenterol 20(24):7950–7954
Bronder CS, Cowey A, Hill J (2004) Delayed stoma formation in Fournier’s gangrene. Colorectal Dis 6(6):518–520. https://doi.org/10.1111/j.1463-1318.2004.00663.x
Czymek R, Kujath P, Bruch HP, Pfeiffer D, Nebrig M, Seehofer D et al (2013) Treatment, outcome and quality of life after Fournier’s gangrene: a multicentre study. Color Dis 15(12):1529–1536
Hallam S, Mothe BS, Tirumulaju RMR (2018) Hartmann’s procedure, reversal and rate of stoma-free survival. Ann R Coll Surg Engl 100(4):301–307
Estrada O, Martinez I, Del Bas M, Salvans S, Hidalgo LA (2009) Rectal diversion without colostomy in Fournier’s gangrene. Tech Coloproctol 13(2):157–159
MarínVivó G, Calixto Rodríguez J, Rodríguez MX (2008) Fecal control system Flexi-Seal FMS. Rev Enferm 31(10):16–20
Ozkan OF, Koksal N, Altinli E, Celik A, Uzun MA, Cıkman O et al (2016) Fournier’s gangrene current approaches. Int Wound J 13(5):713–716
Author information
Authors and Affiliations
Contributions
A. Ortega and E. López conducted the data search and drafted the main text of the manuscript. L.D. Juez prepared the figures and tables. All authors wrote, reviewed, and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ortega Ferrete, A., López, E., Juez Sáez, L.D. et al. Fournier’s gangrene and fecal diversion. When, in which patients, and what type should I perform?. Langenbecks Arch Surg 408, 428 (2023). https://doi.org/10.1007/s00423-023-03137-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03137-3