Abstract
Purpose
Since 01/2018, AVOS (ambulant vor stationär = outpatient to inpatient) regulation has been progressively implemented in hernia surgery in Switzerland. The aim of this prospective, observational, two-centre comparative study was to compare the outcome of outpatient and inpatient post-operative care in terms of AVOS by examining the re-admission rate, complication rate and quality of life in patients with primary unilateral inguinal hernia repair.
Methods
The study ran between 01/2019 and 04/2020 and included 237 patients with a primary unilateral inguinal hernia. Treatment setting was decided according to AVOS guidelines. Primary endpoint was re-admission rate within 6 weeks postoperatively. Secondary endpoints were the complication rate and patient outcome (quality of life) at 6 weeks follow-up postoperatively, as measured by the Short Form 36 Health Survey Questionnaire (SF-36).
Results
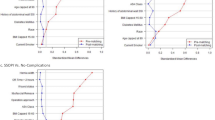
Complications occurred in 11 (14%) inpatient patients, but none required re-admitting for revision until follow-up at 6 weeks after discharge. In the outpatient group, there were 27 (17%) complications reported, while 6 (4%) of these patients crossed over to the inpatient group immediately after surgery. None of the other complications required re-admission until follow-up at 6 weeks. No significant relationship between treatment setting and number of complications/re-admission rate (p=0.458, p=0.061) was observed. The mean outcome (SF-36) between the treatment groups was not significantly different (p=0.16–0.856).
Conclusion
In terms of AVOS selection criteria in Switzerland, primary unilateral inguinal hernia can be safely treated in both treatment settings. Re-admission rates, complications and quality of life do not significantly differ. Day surgery in terms of AVOS might be as effective and efficient, both from the patient’s perspective and that of the institution.
Trial registration number
Similar content being viewed by others
Change history
16 February 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00423-023-02824-5
Abbreviations
- ER:
-
Emergency Room
- TEP:
-
Total Extraperitoneal Patch
- TAPP:
-
Transabdominal Preperitoneal Patch
- ASA:
-
American Society of Anaesthesiologists
- AVOS:
-
Ambulant Vor Stationär = Outpatient to Inpatient
- BMI:
-
Body Mass Index
- DRG:
-
Diagnosis-Related Groups
- SD:
-
Standard Deviation
References
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165
Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362:1561–1571
Schmedt CG, Sauerland S, Bittner R (2005) Comparison of endoscopic procedures vs Lichtenstein and other open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Surg Endosc 19:188–189
Tschuor C, Metzger J, Clavien PA, Vonlanthen R, Lehmann K (2015) Inguinal hernia repair in Switzerland. Hernia 19(5):741–745. https://doi.org/10.1007/s10029-015-1385-2
Light D, Stephenson BM, Sanders DL, British Hernia Society (2020) Management of the uncomplicated primary inguinal hernia in 2019: the practice amongst members of the British Hernia Society. Ann R Coll Surg Engl 102(3):191–193. https://doi.org/10.1308/rcsann.2019.0152
Prabhu A, Chung F (2001) Anaesthetic strategies towards developments in day care surgery. Eur J Anaesthesiol Suppl 23:36–42
De Lathouwer C, Poullier JP (2000) How much ambulatory surgery in the World in 1996–1997 and trends? Ambul Surg 8:191–210
Jarrett PE (2001) Day care surgery. Eur J Anaesthesiol Suppl 23:32–35
Drissi F, Gillion JF, Duchalais E, Hernie C (2021) Readmissions at 30 days after inguinal hernia repair: a series of 5126 patients. J Visc Surg 158(4):299–304. https://doi.org/10.1016/j.jviscsurg.2020.08.009
Steger U, Bisping M, Urban J, Vowinkel T, Wiesmann A, Ryll J (2019) Minimalinvasive Leistenhernienchirurgie – TEP ambulant [Day surgery for endoscopic inguinal hernia repair]. Zentralbl Chir 144(1):26–31. https://doi.org/10.1055/s-0043-123347
Köckerling F, Lorenz R, Reinpold W, Zarras K, Conze J, Kuthe A, Lammers B, Stechemesser B, Mayer F, Fortelny R, Hoffmann H, Kukleta J, Weyhe D (2021) What is the reality in outpatient vs inpatient groin hernia repair? An analysis from the Herniamed Registry. Hernia 16. https://doi.org/10.1007/s10029-021-02494-6
Drissi F, Jurczak F, Cossa JP, Gillion JF (2018) Baayen C; For “Club Hernie”. Outpatient groin hernia repair: assessment of 9330 patients from the French “Club Hernie” database. Hernia 22(3):427–435. https://doi.org/10.1007/s10029-017-1689-5
Weyhe D, Winnemöller C, Hellwig A, Meurer K, Plugge H, Kasoly K, Laubenthal H, Bauer KH, Uhl W (2006) (section sign) 115 b SGB V threatens outpatient treatment for inguinal hernia. Analysis of outcome and economics. Der Chirurg 77:844–855
Wirth U, Saller ML, von Ahnen T et al (2017) Ambulanter transabdomineller präperitonealer Leistenhernienverschluss (TAPP) – um welchen Preis? Chirurg 88:792–798. https://doi.org/10.1007/s00104-017-0429-9
Voorbrood CE, Burgmans JP, Clevers GJ, Davids PH, Verleisdonk EJ, Schouten N, van Dalen T (2015) One-stop endoscopic hernia surgery: efficient and satisfactory. Hernia 19(3):395–400. https://doi.org/10.1007/s10029-013-1151-2
Aiolfi A, Cavalli M, Ferraro SD, Manfredini L, Bonitta G, Bruni PG, Bona D, Campanelli G (2021) Treatment of inguinal hernia: systematic review and updated network meta-analysis of randomized controlled trials. Ann Surg 274(6):954–961. https://doi.org/10.1097/SLA.0000000000004735
Köckerling F, Bittner R, Kofler M, Mayer F, Adolf D, Kuthe A, Weyhe D (2017) Lichtenstein versus total extraperitoneal patch plasty versus transabdominal patch plasty technique for primary unilateral inguinal hernia repair. Ann Surg 269(2):351–357. https://doi.org/10.1097/SLA.0000000000002541
Wake BL, McCormack K, Fraser C, Vale L, Perez J, Grant A (2005) Transabdominal pre-peritoneal (TAPP) vs totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair. Cochrane Database Syst Rev 1:CD004703
Bracale U, Melillo P, Pagnata G, Di Salvo E, Rovani M, Merola G, Pecchia L (2012) Which is the best laparoscopic approach for inguinal hernia repair: TEP or TAPP? A systematic review of the literature with a network meta-analysis. Surg Endosc 26:3355–3366
Antoniou S, Antoniou G, Bartsch D, Fendrich V, Koch OO, Pointner R, Granderath FA (2013) Transabdominal preperitoneal versus totally extraperitoneal repair of inguinal hernia: a meta-analysis of randomized studies. Am J Surg 206:245–252
Wei FX, Zhang YC, Wei H, Zhang YL, Shao Y, Ni R (2015) Transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) for laparoscopic hernia repair: a meta-analysis. Surg Laparosc Endosc Percutan Tech 25:375–383
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Study preparation and data collection were performed by Michal Ziga and Laurin Burla. Analysis and the first draft of the manuscript were written by Michal Ziga, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Zürich (Kantonale Ethikkomission Zürich, BASEC Nr. 2018-10832) and retrospectively registered in ClinicalTrial.com (NCT05234242).
Human and animal rights
All the procedures performed in the study were in accordance with the ethical standards of the institutional review board/international ethics committee for each centre and with the 1964 Helsinki Declaration and its later amendments.
Consent to participate and consent for publication
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ziga, M., Burla, L., Imhof, A. et al. Inguinal hernia treatment in Switzerland: inpatient vs. outpatient setting — HerStAmb Study (prospective observational two-centre comparative study). Langenbecks Arch Surg 408, 14 (2023). https://doi.org/10.1007/s00423-023-02766-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02766-y