Abstract
Purpose
Laparoscopy is the preferred approach to elective surgery for diverticulitis and is increasingly common in the emergent setting. Although diverticulitis is most prevalent among older adults, little is known about the safety of laparoscopy for elderly patients with diverticulitis. This study aims to compare 30-day outcomes of a laparoscopic versus open approach for diverticulitis among elderly patients undergoing elective and urgent/emergent surgery.
Methods
Patients ≥ 65 years who underwent surgery for diverticulitis from 2015 to 2019 were identified from the ACS-NSQIP database. Elective and non-elective groups were analyzed separately. Coarsened exact matching matched laparoscopic and open patients 1:1 based on preoperative factors to minimize selection bias by creating comparable cohorts. Short-term outcomes of laparoscopic versus open surgery were compared.
Results
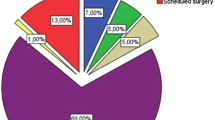
A total of 15,316 patients were included, 69.2% female and 88% White, with a mean age of 72.7 ± 6.1 years. Approximately half (50.9%) of cases were laparoscopic and 60.6% were elective. After matching, laparoscopy was associated with lower 30-day morbidity in both the elective (OR, 0.47; 95%CI, 0.38–0.58) and non-elective (OR, 0.76; 95%CI, 0.58–0.98) cohorts. Laparoscopic surgery in both cohorts was associated with fewer surgical site infections (SSIs) (elective, OR 0.43; 95%CI, 0.33–0.57; non-elective, OR, 0.66; 95%CI, 0.44–0.98) and shorter length of stay (LOS) (elective, mean difference, 1.7 days; 95%CI, 1.5–1.9; non-elective, mean difference, 1.2 days; 95%CI, 0.43–2.1).
Conclusion
Elderly patients undergoing both elective and non-elective laparoscopic surgery for diverticulitis have less 30-day morbidity, SSIs, and shorter LOS compared to an open approach. Therefore, laparoscopy for elderly patients is safe in elective surgery and in select emergent cases as well.
Similar content being viewed by others
References
Masoomi H, Buchberg B, Nguyen B, Tung V, Stamos MJ, Mills S (2011) Outcomes of laparoscopic versus opexn colectomy in elective surgery for diverticulitis. World J Surg 35(9):2143–2148. https://doi.org/10.1007/S00268-011-1117-4
Keller DS, Delaney CP, Hashemi L, Haas EM (2016) A national evaluation of clinical and economic outcomes in open versus laparoscopic colorectal surgery. Surg Endosc 30(10):4220–4228. https://doi.org/10.1007/S00464-015-4732-6/TABLES/5
Letarte F, Hallet J, Drolet S et al (2013) Laparoscopic emergency surgery for diverticular disease that failed medical treatment: a valuable option? Results of a retrospective comparative cohort study. Dis Colon Rectum 56(12):1395–1402. https://doi.org/10.1097/DCR.0B013E3182A760B6
Vennix S, Boersema GS, Buskens CJ et al (2016) Emergency laparoscopic Sigmoidectomy for perforated diverticulitis with generalised peritonitis: a systematic review. Dig Surg 33(1):1–7. https://doi.org/10.1159/000441150
Turley RS, Barbas AS, Lidsky ME, Mantyh CR, Migaly J, Scarborough JE (2013) Laparoscopic versus open Hartmann procedure for the emergency treatment of diverticulitis: a propensity-matched analysis. Dis Colon Rectum 56(1):72–82. https://doi.org/10.1097/DCR.0B013E3182749CF5
Hall J, Hardiman K, Lee S et al The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the treatment of left-sided colonic diverticulitis. Dis Colon Rectum Published online 2020:728–747. https://doi.org/10.1097/DCR.0000000000001679
Sheer AJ, Heckman JE, Schneider EB et al (2011) Congestive heart failure and chronic obstructive pulmonary disease predict poor surgical outcomes in older adults undergoing elective diverticulitis surgery. Dis Colon Rectum 54(11):1430–1437. https://doi.org/10.1097/DCR.0B013E31822C4E85
Lidor AO, Schneider E, Segal J, Yu Q, Feinberg R, Wu AW (2010) Elective surgery for diverticulitis is associated with high risk of intestinal diversion and hospital readmission in older adults. J Gastrointest Surg 14(12):1867–1874. https://doi.org/10.1007/S11605-010-1344-2
Person B, Cera SM, Sands DR et al (2007) Do elderly patients benefit from laparoscopic colorectal surgery? Surg Endosc 22(2):401–405. https://doi.org/10.1007/S00464-007-9412-8
Chautard J, Alves A, Zalinski S, Bretagnol F, Valleur P, Panis Y (2008) Laparoscopic colorectal surgery in elderly patients: a matched case-control study in 178 patients. J Am Coll Surg 206(2):255–260. https://doi.org/10.1016/J.JAMCOLLSURG.2007.06.316
Tuech JJ, Pessaux P, Rouge C et al (2000) Laparoscopic vs open colectomy for sigmoid diverticulitis. Surg Endosc 14:1031–1033. https://doi.org/10.1007/s004640000267
Abbas S (2007) Resection and primary anastomosis in acute complicated diverticulitis, a systematic review of the literature. Int J Colorectal Dis 22:351–357. https://doi.org/10.1007/s00384-005-0059-4
Lee JM et al (2019) Hartmann’s procedure vs primary anastomosis with diverting loop ileostomy for acute diverticulitis: nationwide analysis of 2,729 emergency surgery patients. J Am Coll Surg 229(1):48–55
Oberkofler CE et al (2012) A multicenter randomized clinical trial of primary anastomosis or Hartmann’s procedure for perforated left colonic diverticulitis with purulent or fecal peritonitis. Ann Surgery 256(5):819–827
Bridoux V et al (2017) Hartmann’s procedure or primary anastomosis for generalized peritonitis due to perforated diverticulitis: a prospective multicenter randomized trial (DIVERTI). J Am Coll Surg 225(6):798–805
Author information
Authors and Affiliations
Contributions
Study conception and design, Braschi, Moazzez, and Petrie. Acquisition of data, Moazzez. Analysis and interpretation of data, Moazzez and Braschi. Drafting of manuscript, Braschi, Liu, Moazzez, and Petrie. Critical revision of manuscript, Braschi, Liu, Moazzez, and Petrie.
Corresponding author
Ethics declarations
Disclosures
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS-NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Braschi, C., Liu, J.K., Moazzez, A. et al. Is laparoscopic surgery safe for elderly patients with diverticulitis? A national database study. Langenbecks Arch Surg 407, 3599–3606 (2022). https://doi.org/10.1007/s00423-022-02695-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02695-2