Abstract
Objectives
Totally laparoscopic total gastrectomy has been developed with difficulty in intracorporeal esophagojejunostomy. Although mechanical stapling has been widely used for intracorporeal esophagojejunostomy, manual suture holds great promise with the emergence of high-resolution 3D vision and robotic surgery. After exploration of how to improve the safety and efficiency of intracorporeal suture for esophagojejunostomy, we recommended the technique of single-layer running “trapezoid-shaped” suture. The cost-effectiveness was analyzed by comparing with conventional mechanical stapling.
Methods
The study retrospectively reviewed the patients undergoing laparoscopic gastrectomy for gastric cancer from January 2010 to December 2021. The patients were divided into two cohorts based on the methods of intracorporeal esophagojejunostomy: manual suture versus stapling suture. Propensity score matching was performed to match patients from the two cohorts at a ratio of 1:1. Then group comparison was made to determine whether manual suture was non-inferior to stapling suture in terms of operation time, anastomotic complications, postoperative hospital stay, and surgical cost.
Results
The study included 582 patients with laparoscopic total gastrectomy. The manual and stapling suture for esophagojejunostomy were performed in 50 and 532 patients, respectively. In manual suture cohort, the median time for the whole operation and digestive tract reconstruction were 300 min and 110 min. There was no anastomotic bleeding and stenosis but two cases of anastomotic leak which occurred at 3 days after surgery. The median length of postoperative hospital stay was 11 days. After propensity score matching, group comparison yielded two variables with statistical significance: time for digestive tract reconstruction and surgery cost. The manual suture cohort spent less money but more time for esophagojejunostomy. Intriguingly, the learning curve of manual suture revealed that the time for digestive tract reconstruction was declined with accumulated number of operations.
Conclusions
Laparoscopic single-layer running “trapezoid-shaped” suture appears safe and cost-effective for intracorporeal esophagojejunostomy after total gastrectomy. Although the concern remains about prolonged operation time for beginners of performing the suture method, adequate practice is expected to shorten the operation time based on our learning curve analysis.




Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Li GZ, Doherty GM, Wang J (2022) Surgical management of gastric cancer: a review. JAMA Surg 157(5):446–454. https://doi.org/10.1001/jamasurg.2022.0182
Kitano S, Iso Y, Moriyama M, Sugimachi K (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4(2):146–148
Huang C, Liu H, Hu Y, Sun Y, Su X, Cao H, Hu J, Wang K, Suo J, Tao K, He X, Wei H, Ying M, Hu W, Du X, Yu J, Zheng C, Liu F, Li Z et al (2022) Laparoscopic vs open distal gastrectomy for locally advanced gastric cancer: five-year outcomes from the CLASS-01 randomized clinical trial. JAMA Surg 157(1):9–17. https://doi.org/10.1001/jamasurg.2021.5104
Hyung WJ, Yang HK, Park YK, Lee HJ, An JY, Kim W, Kim HI, Kim HH, Ryu SW, Hur H, Kim MC, Kong SH, Cho GS, Kim JJ, Park DJ, Ryu KW, Kim YW, Kim JW, Lee JH et al (2020) Long-term outcomes of laparoscopic distal gastrectomy for locally advanced gastric cancer: the KLASS-02-RCT randomized clinical trial. J Clin Oncol 38(28):3304–3313. https://doi.org/10.1200/JCO.20.01210
Katai H, Mizusawa J, Katayama H, Morita S, Yamada T, Bando E, Ito S, Takagi M, Takagane A, Teshima S, Koeda K, Nunobe S, Yoshikawa T, Terashima M, Sasako M (2020) Survival outcomes after laparoscopy-assisted distal gastrectomy versus open distal gastrectomy with nodal dissection for clinical stage IA or IB gastric cancer (JCOG0912): a multicentre, non-inferiority, phase 3 randomised controlled trial. Lancet Gastroenterol Hepatol 5(2):142–151. https://doi.org/10.1016/S2468-1253(19)30332-2
van der Veen A, Brenkman HJF, Seesing MFJ, Haverkamp L, Luyer MDP, Nieuwenhuijzen GAP, Stoot JHMB, Tegels JJW, Wijnhoven BPL, Lagarde SM, de Steur WO, Hartgrink HH, Kouwenhoven EA, Wassenaar EB, Draaisma WA, Gisbertz SS, van der Peet DL, May AM, Ruurda JP et al (2021) Laparoscopic versus open gastrectomy for gastric cancer (LOGICA): a multicenter randomized clinical trial. J Clin Oncol 39(9):978–989. https://doi.org/10.1200/JCO.20.01540
Lee I, Oh Y, Park SH, Kwon Y, Park S (2020) Postoperative nutritional outcomes and quality of life-related complications of proximal versus total gastrectomy for upper-third early gastric cancer: a meta-analysis. Sci Rep 10(1):21460. https://doi.org/10.1038/s41598-020-78458-0
Sato R, Kinoshita T, Akimoto E, Yoshida M, Nishiguchi Y, Harada J (2021) Feasibility and quality of life assessment of laparoscopic proximal gastrectomy using double-tract reconstruction. Langenbeck's Arch Surg 406(2):479–489. https://doi.org/10.1007/s00423-020-02076-7
Kimura Y, Mikami J, Yamasaki M, Hirao M, Imamura H, Fujita J, Takeno A, Matsuyama J, Kishi K, Hirao T, Fukunaga H, Demura K, Kurokawa Y, Takiguchi S, Eguchi H, Doki Y (2020) Comparison of 5-year postoperative outcomes after Billroth I and Roux-en-Y reconstruction following distal gastrectomy for gastric cancer: results from a multi-institutional randomized controlled trial. Ann Gastroenterol Surg 5(1):93–101. https://doi.org/10.1002/ags3.12400
Zhao S, Zheng K, Zheng JC, Hou TT, Wang ZN, Xu HM, Jiang CG (2019) Comparison of totally laparoscopic total gastrectomy and laparoscopic-assisted total gastrectomy: a systematic review and meta-analysis. Int J Surg 68:1–10. https://doi.org/10.1016/j.ijsu.2019.05.020
Chen K, He Y, Cai JQ, Pan Y, Wu D, Chen DW, Yan JF, Maher H, Mou YP (2016) Comparing the short-term outcomes of intracorporeal esophagojejunostomy with extracorporeal esophagojejunostomy after laparoscopic total gastrectomy for gastric cancer. BMC Surg 16:13. https://doi.org/10.1186/s12893-016-0130-9
Wang Z, Wei Y, Liu X, Li Z, Zhu G, Li Y, Wang K (2021) Application value of hand-sewn anastomosis in totally laparoscopic total gastrectomy for gastric cancer. World J Surg Oncol 19(1):229. https://doi.org/10.1186/s12957-021-02249-8
Chen K, Pan Y, Cai JQ, Xu XW, Wu D, Yan JF, Chen RG, He Y, Mou YP (2016) Intracorporeal esophagojejunostomy after totally laparoscopic total gastrectomy: a single-center 7-year experience. World J Gastroenterol 22(12):3432–3440. https://doi.org/10.3748/wjg.v22.i12.3432
Chen XH, Hu YF, Luo J, Chen YH, Liu H, Lin T, Chen H, Li GX, Yu J (2019) The safety of esophagojejunostomy via a transorally inserted-anvil method vs extracorporeal anastomosis using a circular stapler during total gastrectomy for Siewert type 2 adenocarcinoma of the esophagogastric junction. Gastroenterol Rep (Oxf) 8(3):242–251. https://doi.org/10.1093/gastro/goz046
Du J, Zhao L, Xue H, Hu J, Zhang Z (2022) Bracket-like suture method: a novel, circular marked, simplest sided purse-string suture technique for intracorporeal circular-stapled oesophagojejunostomy during laparoscopic total gastrectomy. Langenbeck's Arch Surg 407(1):357–364. https://doi.org/10.1007/s00423-021-02305-7
Takayama Y, Kaneoka Y, Maeda A, Fukami Y, Takahashi T, Uji M (2019) A novel technique of hand-sewn purse-string suturing by double ligation method (DLM) for intracorporeal circular esophagojejunostomy. J Gastric Cancer 19(3):290–300. https://doi.org/10.5230/jgc.2019.19.e26
Charalabopoulos A, Davakis S, Paraskeva P, Machairas N, Kapelouzou A, Kordzadeh A, Sakarellos P, Vailas M, Baili E, Bakoyiannis C, Felekouras E (2021) Feasibility and short-term outcomes of three-dimensional hand-sewn esophago-jejunal anastomosis in completely laparoscopic total gastrectomy for cancer. Cancers (Basel) 13(18):4709. https://doi.org/10.3390/cancers13184709
Chen K, Wu D, Pan Y, Cai JQ, Yan JF, Chen DW, Maher H, Mou YP (2016) Totally laparoscopic gastrectomy using intracorporeally stapler or hand-sewn anastomosis for gastric cancer: a single-center experience of 478 consecutive cases and outcomes. World J Surg Oncol 14:115. https://doi.org/10.1186/s12957-016-0868-7
Sindayigaya R, Guizani M, Thébault B, Dussart D, Abou Mrad Fricquegnon A, Piquard A, Saint-Marc O (2019) Robot-assisted total gastrectomy: preliminary evaluation. J Laparoendosc Adv Surg Tech A 29(5):589–594. https://doi.org/10.1089/lap.2018.0659
Jiang ZW, Liu J, Wang G, Zhao K, Zhang S, Li N, Li JS (2015) Esophagojejunostomy reconstruction using a robot-sewing technique during totally robotic total gastrectomy for gastric cancer. Hepatogastroenterology 62(138):323–326
Huang C, Zhao J, Liu Z, Huang J, Zhu Z (2020) Esophageal suspension method for hand-sewn esophagojejunostomy after totally laparoscopic total gastrectomy: a simple, safe, and feasible suturing technique. Front Oncol 10:575. https://doi.org/10.3389/fonc.2020.00575
Park KB, Kim EY, Song KY (2019) Esophagojejunal anastomosis after laparoscopic total gastrectomy for gastric cancer: circular versus linear stapling. J Gastric Cancer 19(3):344–354. https://doi.org/10.5230/jgc.2019.19.e34
Sajid MS, Siddiqui MR, Baig MK (2012) Single layer versus double layer suture anastomosis of the gastrointestinal tract. Cochrane Database Syst Rev 1:CD005477. https://doi.org/10.1002/14651858.CD005477.pub4
Nieto JE, Dechant JE, Snyder JR (2006) Comparison of one-layer (continuous Lembert) versus two-layer (simple continuous/Cushing) hand-sewn end-to-end anastomosis in equine jejunum. Vet Surg 35(7):669–673. https://doi.org/10.1111/j.1532-950X.2006.00206.x
Herrle F, Diener MK, Freudenberg S, Willeke F, Kienle P, Boenninghoff R, Weiss C, Partecke LI, Schuld J, Post S (2016) Single-layer continuous versus double-layer continuous suture in colonic anastomoses-a randomized multicentre trial (ANATECH Trial). J Gastrointest Surg 20(2):421–430. https://doi.org/10.1007/s11605-015-3003-0
Tavakoli A, Bakhtiari J, Khalaj AR, Gharagozlou MJ, Veshkini A (2010) Single-layer versus double-layer laparoscopic intracorporeally sutured gastrointestinal anastomoses in the canine model. JSLS 14(4):509–515. https://doi.org/10.4293/108680810X12924466007881
Zhang F, Qiao S, Li C, Wu B, Reischl S, Neumann PA (2020) The immunologic changes during different phases of intestinal anastomotic healing. J Clin Lab Anal 34(11):e23493. https://doi.org/10.1002/jcla.23493
Ballantyne GH (1984) The experimental basis of intestinal suturing. Effect of surgical technique, inflammation, and infection on enteric wound healing. Dis Colon Rectum 27(1):61–71. https://doi.org/10.1007/BF02554084
Ellison GW, Case JB, Regier PJ (2019) Intestinal surgery in small animals: historical foundations, current thinking, and future horizons. Vet Surg 48(7):1171–1180. https://doi.org/10.1111/vsu.13275
Rozier MD, Ghaferi AA, Rose AM, Simon NJ, Birkmeyer NJ, Prosser LA (2020) Preferences for bariatric surgery: comparing surgeons and patients using a discrete choice experiment. Surg Obes Relat Dis 16(6):738–744. https://doi.org/10.1016/j.soard.2020.02.005
Roh CK, Lee S, Son SY, Hur H, Han SU (2021) Risk factors for the severity of complications in minimally invasive total gastrectomy for gastric cancer: a retrospective cohort study. J Gastric Cancer 21(4):352–367. https://doi.org/10.5230/jgc.2021.21.e34
Qiu GL, Li XW, Wang HJ, Wang PX, Liu JH, Zhu MK, Liao XH, Fan L, Che XM (2022) Influence of visceral lipids obesity on the early postoperative complications after radical gastrectomy. Zhonghua Wei Chang Wai Ke Za Zhi 25(7):596–603. Chinese. https://doi.org/10.3760/cma.j.cn441530-20210907-00365
Bracale U, Corcione F, Pignata G, Andreuccetti J, Dolce P, Boni L, Cassinotti E, Olmi S, Uccelli M, Gualtierotti M, Ferrari G, De Martini P, Bjelović M, Gunjić D, Cuccurullo D, Sciuto A, Pirozzi F, Peltrini R (2021) Impact of neoadjuvant therapy followed by laparoscopic radical gastrectomy with D2 lymph node dissection in Western population: a multi-institutional propensity score-matched study. J Surg Oncol 124(8):1338–1346. https://doi.org/10.1002/jso.26657
Cui H, Zhang KC, Cao B, Deng H, Liu GB, Song LQ, Zhao RY, Liu Y, Chen L, Wei B (2022) Short and long-term outcomes between laparoscopic and open total gastrectomy for advanced gastric cancer after neoadjuvant chemotherapy. World J Gastrointest Surg 14(5):452–469. https://doi.org/10.4240/wjgs.v14.i5.452
Liu L, Wang C, Li F, Zhang X, Cheng X, Lin S, Liu Y, Yang C, Li W (2022) The safety and efficacy of laparoscopic gastrectomy for patients with locally advanced gastric cancer following neoadjuvant chemotherapy. Sci Rep 12(1):10384. https://doi.org/10.1038/s41598-022-14717-6
Funding
1. National Natural Science Foundation (Grant Number: 81874058 to Jian-Ping Zhang)
2. 789 Outstanding Talent Program of SAHNMU (Grant Number: 789ZYRC202070210 to Wei Wei)
3. Project of Invigorating Health Care through Science, Technology and Education of Jiangsu Province Medical Youth Talent (Grant Number: QNRC2016671 to Wei Wei)
Author information
Authors and Affiliations
Contributions
Xu L, Wang XQ, and Lu N collected data; Wei W, Xu L, and Gu QO drafted the manuscript; Tang CY helped in acquisition of the data and performed data analysis; Yang QP, Shen J, and Dong XG were responsible for illustration design and video editing. Zhang JP and Wei W designed the study, supervised the study, and revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and approved by the Research Ethics Committee of Nanjing Medical University. The informed written consent was obtained from all study participants or their legal guardian prior to study enrollment.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information

Fig. S1
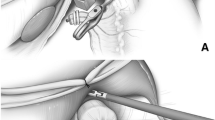
Distribution of anastomosis tension is different between end-to-side and side-to-side esophagojejunostomy. The circular stapling renders the esophagus vertically anastomosed to jejunal limb, which creates an anastomosis with evenly distributed tensile strength (A). However, when esophagojejunostomy is performed in a side-to-side manner by a linear stapler (B), tensile strength varys along the anastomotic line with a weak point at the cephlic part (C). The linear stapler is designed to perform anastomosis with three rows of staples, except at the cephalic point where there is only one raw of staples (D). (PNG 175 kb)
(MP4 20587 kb)
(MP4 364028 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, L., Tang, CY., Wang, XQ. et al. Laparoscopic single-layer running “trapezoid-shaped” suture versus mechanical stapling for esophagojejunostomy after total gastrectomy for gastric cancer: cost-effect analysis of propensity score-matched study cohorts. Langenbecks Arch Surg 407, 3397–3406 (2022). https://doi.org/10.1007/s00423-022-02694-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02694-3