Abstract
Purpose
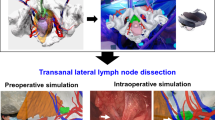
Urethral injury is one of the most important complications in transanal total mesorectal excision (TaTME) in male patients with rectal cancer. The purpose of this study was to investigate holographic image-guided surgery in TaTME.
Methods
Polygon (stereolithography) files were created and exported from SYNAPSE VINCENT, and then uploaded into the Holoeyes MD system (Holoeyes Inc., Tokyo, Japan). After uploading the data, the three-dimensional image was automatically converted into a case-specific hologram. The hologram was then installed into the head mount display, HoloLens (Microsoft Corporation, Redmond, WA). The surgeons and assistants wore the HoloLens when they performed TaTME.
Results
In a Wi-Fi-enabled operating room, each surgeon, wearing a HoloLens, shared the same hologram and succeeded in adjusting the hologram by making simple hand gestures from their respective angles. The hologram contributed to better comprehension of the positional relationships between the urethra and the surrounding pelvic organs during surgery. All surgeons were able to properly determine the dissection line.
Conclusions
This first experience suggests that intraoperative holograms contributed to reducing the risk of urethral injury and understanding transanal anatomy. Intraoperative holograms have the potential to become a new next-generation surgical support tool for use in spatial awareness and the sharing of information between surgeons.




Similar content being viewed by others
Availability of data and materials
The current datasets are deposited in publicly available repositories (where available and appropriate).
Code availability
Not applicable.
Abbreviations
- TaTME:
-
Transanal total mesorectal excision
- HMD:
-
Head mount display
- 3D:
-
Three-dimensional
- MR images:
-
Magnetic resonance images
- MDCT:
-
Multi-detector computed tomography
References
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery – the clue to pelvic recurrence? Br J Surg 69(10):613–616
de Lacy AM, Rattner DW, Adelsdorfer C, Tasende MM, Fernández M, Delgado S, Sylla P, Martínez-Palli G (2013) Transanal natural orifice transluminal endoscopic surgery (NOTES) rectal resection: “down-to up” total mesorectal excision (TME)-short-term outcomes in the first 20 cases. Surg Endosc 27(9):3165–3172
Ma B, Gao P, Song Y, Zhang C, Zhang C, Wang L, Liu H, Wang Z (2016) Transanal total mesorectal excision (taTME) for rectal cancer: a systematic review and meta-analysis of oncological and perioperative outcomes compared with laparoscopic total mesorectal excision. BMC Cancer 4(16):380
Xu W, Xu Z, Cheng H, Ying J, Cheng F, Xu W, Cao J, Luo J (2016) Comparison of short-term clinical outcomes between transanal and laparoscopic total mesorectal excision for the treatment of mid and low rectal cancer: a meta-analysis. Eur J Surg Oncol 42(12):1841–1850
Rubinkiewicz M, Czerwińska A, Zarzycki P, Małczak P, Nowakowski M, Major P, Budzyński A, Pędziwiatr M (2018) Comparison of short-term clinical and pathological outcomes after transanal versus laparoscopic total mesorectal excision for low anterior rectal resection due to rectal cancer: a systematic review with meta-analysis. J Clin Med 7(11):448
Aubert M, Mege D, Panis Y (2020) Total mesorectal excision for low and middle rectal cancer: laparoscopic versus transanal approach-a meta-analysis. Surg Endosc 34(9):3908–3919
Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J, Moran B, Hanna GB, Mortensen NJ, Tekkis PP, International TaTME Registry Collaborative (2019) Incidence and risk factors for anastomotic failure in 1594 patients treated by transanal total mesorectal excision: results from the international TaTME registry. Ann Surg 269(4):700–711
Rouanet P, Mourregot A, Azar CC, Carrere S, Gutowski M, Quenet F, Saint-Aubert B, Colombo PE (2013) Transanal endoscopic proctectomy: an innovative procedure for difficult resection of rectal tumors in men with narrow pelvis. Dis Colon Rectum 56:408–415
Atallah S (2015) Transanal total mesorectal excision: full steam ahead. Tech Coloproctol 19:57–61
Sylla P, Knol JJ, D’Andrea AP, Perez RO, Atallah SB, Penna M, Hompes R, Wolthuis A, Rouanet P, Fingerhut A, International taTME Urethral Injury Collaborative (2021) Urethral injury and other urologic injuries during transanal total mesorectal excision: an international collaborative study. Ann Surg 274(2):e115–e125
Tokunaga T, Higashijima J, Yoshikawa K, Nishi M, Kashihara H, Takasu C, Shimada M (2020) The usefulness of intraoperative X-ray fluoroscopy in avoiding urethral injury during transanal total mesorectal excision. Asian J Endosc Surg 13(2):242–245
Pratt P, Ives M, Lawton G, Simmons J, Radev N, Spyropoulou L, Amiras D (2018) Through the HoloLens™ looking glass: augmented reality for extremity reconstruction surgery using 3D vascular models with perforating vessels. Eur Radiol Exp 2(1):2
Müller F, Roner S, Liebmann F, Spirig JM, Fürnstahl P, Farshad M (2020) Augmented reality navigation for spinal pedicle screw instrumentation using intraoperative 3D imaging. Spine J 20(4):621–628
Neves CA, Vaisbuch Y, Leuze C, McNab JA, Daniel B, Blevins NH, Hwang PH (2020) Application of holographic augmented reality for external approaches to the frontal sinus. Int Forum Allergy Rhinol 10(7):920–925
Scherl C, Stratemeier J, Karle C, Rotter N, Hesser J, Huber L, Männle D (2021) Augmented reality with HoloLens in parotid surgery: how to assess and to improve accuracy. Eur Arch Otorhinolaryngol 278(7):2473–2483
Tepper OM, Rudy HL, Lefkowitz A, Weimer KA, Marks SM, Stern CS, Garfein ES (2017) Mixed reality with HoloLens: where virtual reality meets augmented reality in the operating room. Plast Reconstr Surg 140(5):1066–1070
Saito Y, Sugimoto M, Imura S, Morine Y, Ikemoto T, Iwahashi S, Yamada S, Shimada M (2020) Intraoperative 3D hologram support with mixed reality techniques in liver surgery. Ann Surg 271(1):e4–e7
Incekara F, Smits M, Dirven C, Vincent A (2018) Clinical feasibility of a wearable mixed-reality device in neurosurgery. World Neurosurg 118:e422–e427
Atallah S, Martin-Perez B, Larach S (2015) Image-guided real-time navigation for transanal total mesorectal excision: a pilot study. Tech Coloproctol 19:679–684
Acknowledgements
We thank Jane Charbonneau, DVM, from Edanz (https://jp.edanz.com/ac), for editing draft of this manuscript. We also thank Holoeyes Inc. for their technical support.
Author information
Authors and Affiliations
Contributions
Takuya Tokunaga: study concepts and design, analysis and interpretation of data, manuscript preparation. Maki Sugimoto: drafting of the manuscript, software development, technical instruction, critical revision of the manuscript. Yu Saito: acquisition of data, analysis and interpretation of data. Hideya Kashihara: study concepts and design, technical instruction. Kozo Yoshikawa: statistical analysis. Toshihiro Nakao: study concepts and design, analysis and interpretation of data. Masaaki Nishi: statistical analysis. Chie Takasu: quality control of data and algorithms. Toshiaki Yoshimoto: acquisition of data. Shoko Yamashita: acquisition of data. Noriko Yokota: acquisition of data. Yosuke Iwakawa: acquisition of data. Mitsuo Shimada: drafting of the manuscript, critical revision of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by Tokushima University Hospital ethics committee and with the approval of corresponding regulatory agencies, and all the experiments were carried out in accordance with the approved guidelines (Tokushima Clinical Trial Management System Number; 3294). Meanwhile, all the patients involved in the study signed the informed consent form and agreed to participate.
Consent to participate
All patients consented to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tokunaga, T., Sugimoto, M., Saito, Y. et al. Intraoperative holographic image-guided surgery in a transanal approach for rectal cancer. Langenbecks Arch Surg 407, 2579–2584 (2022). https://doi.org/10.1007/s00423-022-02607-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02607-4