Abstract
Purpose
A recent trend in urinary catheter management in patients who underwent laparoscopic rectal cancer surgery is early removal. However, some patients develop bladder dysfunction and require urinary re-catheterization. In 2016, a scoring system to predict bladder dysfunction after laparoscopic rectal cancer surgery was developed in our institution. The aim of this study was to demonstrate the validity of this scoring system and to determine the suitability of patients for early removal of urinary catheter.
Methods
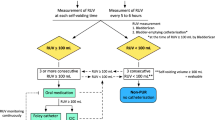
A single-center, retrospective study from a prospective database was conducted on 234 patients who underwent elective laparoscopic rectal cancer surgery between January 2016 and December 2019. According to bladder dysfunction predictive score, the urinary catheter was removed on the first postoperative day (low-risk group) and fifth postoperative day (high-risk group). After catheter removal, all patients were managed using in-house protocols.
Results
Of 234 patients, 130 (55.6%) were classified as a low-risk group. The overall incidence of bladder dysfunction was 8.5% (11/130) in the low-risk group and 13.5% (14/104) in the high-risk group.
Conclusion
The scoring system developed to predict bladder dysfunction showed good overall performance for discriminating between patients suitable or not for early removal of urinary catheter after laparoscopic rectal cancer surgery.


Similar content being viewed by others
References
Carmichael JC, Keller DS, Baldini G, Bordeianou L, Weiss E, Lee L, Boutros M, McClane J, Feldman LS, Steele SR (2017) Clinical practice guidelines for enhanced recovery after colon and rectal surgery from the American Society of Colon and Rectal Surgeons and Society of American Gastrointestinal and Endoscopic Surgeons. Dis Colon Rectum 60:761–784. https://doi.org/10.1097/DCR.0000000000000883
Duchalais E, Larson DW, Machairas N, Mathis KL, Dozois EJ, Kelley SR (2019) Outcomes of early removal of urinary catheter following rectal resection for cancer. Ann Surg Oncol 26:79–85. https://doi.org/10.1245/s10434-018-6822-x
Zmora O, Madbouly K, Tulchinsky H, Hussein A, Khaikin M (2010) Urinary bladder catheter drainage following pelvic surgery—is it necessary for that long? Dis Colon Rectum 53:321–326. https://doi.org/10.1007/DCR.06013e3181c7525c
Patel DN, Felder SI, Luu M, Daskivich TJ, Zaghiyan KN, Fleshner P (2018) Early urinary catheter removal following pelvic colorectal surgery: a prospective, randomized, noninferiority trial. Dis Colon Rectum 61:1180–1186. https://doi.org/10.1097/DCR.0000000000001206
Hiraki M, Tanaka T, Sadashima E, Sato H, Kitahara K (2021) Retrospective risk analysis for acute urinary dysfunction after laparoscopic rectal cancer surgery in patients receiving epidural analgesia. Int J Colorectal Dis 36:169–175. https://doi.org/10.1007/s00384-020-03745-1
Hamamoto H, Yamamoto M, Masubuchi S, Ishii M, Osumi W, Tanaka K, Okuda J, Uchiyama K (2020) Male sex and anterior wall tumor location as risk factors for urinary dysfunction after laparoscopic rectal surgery. Surg Endosc 34:3567–3573. https://doi.org/10.1007/s00464-019-07186-y
Sterk P, Shekarriz B, Gunter S, Nolde J, Keller R, Bruch HP, Shekarriz H (2005) Voiding and sexual dysfunction after deep rectal resection and total mesorectal excision: prospective study on 52 patients. Int J Colorectal Dis 20:423–427. https://doi.org/10.1007/s00384-004-0711-4
Kim HO, Cho YS, Kim H, Lee SR, Jung KU, Chun HK (2016) Scoring systems used to predict bladder dysfunction after laparoscopic rectal cancer surgery. World J Surg 40:3044–3051. https://doi.org/10.1007/s00268-016-3636-5
Kehlet H, Wilmore DW (2008) Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 248:189–198. https://doi.org/10.1097/SLA.0b013e31817f2c1a
Davis NF, Bhatt NR, MacCraith E, Flood HD, Mooney R, Leonard G, Walsh MT (2020) Long-term outcomes of urethral catheterisation injuries: a prospective multi-institutional study. World J Urol 38:473–480. https://doi.org/10.1007/s00345-019-02775-x
Manalo M Jr, Lapitan MC, Buckley BS (2011) Medical interns’ knowledge and training regarding urethral catheter insertion and insertion-related urethral injury in male patients. BMC Med Educ 11:73. https://doi.org/10.1186/1472-6920-11-73
Feneley RC, Hopley IB, Wells PN (2015) Urinary catheters: history, current status, adverse events and research agenda. J Med Eng Technol 39:459–470. https://doi.org/10.3109/03091902.2015.1085600
Smart NJ, White P, Allison AS, Ockrim JB, Kennedy RH, Francis NK (2012) Deviation and failure of enhanced recovery after surgery following laparoscopic colorectal surgery: early prediction model. Colorectal Dis 14:e727–e734. https://doi.org/10.1111/j.1463-1318.2012.03096.x
Tammela T, Kontturi M, Lukkarinen O (1986) Postoperative urinary retention. I. Incidence and predisposing factors. Scand J Urol Nephrol 20:197–201. https://doi.org/10.3109/00365598609024494
Keita H, Diouf E, Tubach F, Brouwer T, Dahmani S, Mantz J, Desmonts JM (2005) Predictive factors of early postoperative urinary retention in the postanesthesia care unit. Anesth Analg 101:592–6, table of contents. https://doi.org/10.1213/01.Ane.0000159165.90094.40
Mundy AR (1982) An anatomical explanation for bladder dysfunction following rectal and uterine surgery. Br J Urol 54:501–504. https://doi.org/10.1111/j.1464-410x.1982.tb13575.x
Benoist S, Panis Y, Denet C, Mauvais F, Mariani P, Valleur P (1999) Optimal duration of urinary drainage after rectal resection: a randomized controlled trial. Surgery 125:135–141
Toritani K, Watanabe J, Suwa Y, Suzuki S, Nakagawa K, Suwa H, Ishibe A, Ota M, Kunisaki C, Endo I (2019) The risk factors for urinary dysfunction after autonomic nerve-preserving rectal cancer surgery: a multicenter retrospective study at Yokohama Clinical Oncology Group (YCOG1307). Int J Colorectal Dis 34:1697–1703. https://doi.org/10.1007/s00384-019-03374-3
Hojo K, Vernava AM 3rd, Sugihara K, Katumata K (1991) Preservation of urine voiding and sexual function after rectal cancer surgery. Dis Colon Rectum 34:532–539. https://doi.org/10.1007/bf02049890
Saito N, Koda K, Nobuhiro K, Takiguchi K, Oda K, Soda H, Nunomura M, Sarashina H, Nakajima N (1999) Nerve-sparing surgery for advanced rectal cancer patients: special reference to Dukes C patients. World J Surg 23:1062–1068. https://doi.org/10.1007/s002689900624
Author information
Authors and Affiliations
Contributions
Study conception and design: Min C, Lee SR, Jung KU, Kim H, and Kim HO. Acquisition of data: Min C, Kim YB, Park Y, and Son JT. Analysis and interpretation of data: Lee KH and Min C. Drafting of manuscript: Lee KH and Min C. Critical revision of manuscript: Lee KH, Kim YB, Park Y, Son JT, Lee SR, Jung KU, Kim H, and Kim HO.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board of Kangbuk Samsung Hospital (KBSMC 2016–07-003, KBSMC 2021–06-015).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, K.H., Min, C., Kim, H.O. et al. Validation of a scoring system to predict bladder dysfunction after laparoscopic rectal cancer surgery. Langenbecks Arch Surg 407, 2929–2935 (2022). https://doi.org/10.1007/s00423-022-02582-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02582-w