Abstract
Purpose
Sarcopenia is common in pancreatic cancer patients. Considering the growing adoption of standardized protocols for enhanced recovery after surgery (ERAS), we examined the clinical impact of sarcopenia in pancreaticoduodenectomy (PD) patients in a 5-day accelerated ERAS program, termed the Whipple Accelerated Recovery Pathway.
Methods
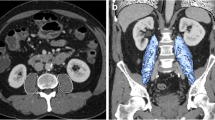
A retrospective review was conducted of patients undergoing PD from 2017 through 2020 on the ERAS pathway. Preoperative computerized tomographic scans taken within 45 days before surgery were analyzed to determine psoas muscle cross-sectional area (PMA) at the third lumbar vertebral body. Sarcopenia was defined as the lowest quartile of PMA respective to gender. Outcome measures were compared between patients with or without sarcopenia.
Results
In this 333-patient cohort, 252 (75.7%) patients had final pathology revealing pancreatic or periampullary cancer. The median age was 66.7 years (16.4–88.4 years) with a 161:172 male to female ratio. Sarcopenia correlated with delayed tolerance of oral intake (OR 2.2; 95%CI 1.1–4.3, P = 0.03), increased complication rates (OR 4.3; 95%CI 2.2–8.5, P < 0.01), and longer hospital length of stay (LOS) (P < 0.05). Preoperative albumin levels, BMI, and history of pancreatitis were also found to correlate with LOS (P < 0.05). Multivariate regression analysis found low PMA, BMI, and male gender to be independent predictors of increased LOS (P < 0.05).
Conclusion
Sarcopenia correlated with increased LOS and postoperative complications in ERAS patients after PD. Sarcopenia can be used to predict poor candidates for ERAS protocols who may require an alternative recovery protocol, promoting a clinical tier-based approach to ERAS for pancreatic surgery.

Similar content being viewed by others
References
McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS (2018) Pancreatic cancer: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol 24(43):4846–4861
Ansari D, Tingstedt B, Andersson B, Holmquist F, Sturesson C, Williamsson C et al (2016) Pancreatic cancer: yesterday, today and tomorrow. Future Oncol 12(16):1929–1946
Singhi AD, Koay EJ, Chari ST, Maitra A (2019) Early detection of pancreatic cancer: opportunities and challenges. Gastroenterology 156(7):2024–2040
Furukawa H, Okada S, Saisho H, Ariyama J, Karasawa E, Nakaizumi A et al (1996) Clinicopathologic features of small pancreatic adenocarcinoma. A collective study Cancer 78(5):986–990
Tran KTC, Smeenk HG, van Eijck CHJ, Kazemier G, Hop WC, Greve JWG et al (2004) Pylorus preserving pancreaticoduodenectomy versus standard Whipple procedure: a prospective, randomized, multicenter analysis of 170 patients with pancreatic and periampullary tumors. Ann Surg 240(5):738–745
D’Cruz JR, Misra S, Shamsudeen S. Pancreaticoduodenectomy. StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
Srinarmwong C, Luechakiettisak P, Prasitvilai W (2008) Standard Whipple’s operation versus pylorus preserving pancreaticoduodenectomy: a randomized controlled trial study. J Med Assoc Thai 91(5):693–698
Lassen K, Coolsen MME, Slim K, Carli F, de Aguilar-Nascimento JE, Schäfer M et al (2012) Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin Nutr 31(6):817–830
Ji H-B, Zhu W-T, Wei Q, Wang X-X, Wang H-B, Chen Q-P (2018) Impact of enhanced recovery after surgery programs on pancreatic surgery: a meta-analysis. World J Gastroenterol 24(15):1666–1678
Melloul E, Lassen K, Roulin D, Grass F, Perinel J, Adham M et al (2020) Guidelines for perioperative care for pancreatoduodenectomy: enhanced recovery after surgery (ERAS) recommendations 2019. World J Surg 44(7):2056–2084
Bongers BC, Dejong CHC, den Dulk M. Enhanced recovery after surgery programmes in older patients undergoing hepatopancreatobiliary surgery: what benefits might prehabilitation have? Eur J Surg Oncol. 2021 Mar;47(3 Pt A):551–9.
Lavu H, McCall NS, Winter JM, Burkhart RA, Pucci M, Leiby BE et al (2019) Enhancing patient outcomes while containing costs after complex abdominal operation: a randomized controlled trial of the Whipple accelerated recovery pathway. J Am Coll Surg 228(4):415–424
Whittle J, Wischmeyer PE, Grocott MPW, Miller TE (2018) Surgical prehabilitation: nutrition and exercise. Anesthesiol Clin 36(4):567–580
Thomas G, Tahir MR, Bongers BC, Kallen VL, Slooter GD, van Meeteren NL (2019) Prehabilitation before major intra-abdominal cancer surgery: a systematic review of randomised controlled trials. Eur J Anaesthesiol 36(12):933–945
Wilson RJT, Davies S, Yates D, Redman J, Stone M (2010) Impaired functional capacity is associated with all-cause mortality after major elective intra-abdominal surgery. Br J Anaesth 105(3):297–303
Choi MH, Yoon SB, Lee K, Song M, Lee IS, Lee MA et al (2018) Preoperative sarcopenia and post-operative accelerated muscle loss negatively impact survival after resection of pancreatic cancer. J Cachexia Sarcopenia Muscle 9(2):326–334
Ozola Zalite I, Zykus R, Francisco Gonzalez M, Saygili F, Pukitis A, Gaujoux S et al (2015) Influence of cachexia and sarcopenia on survival in pancreatic ductal adenocarcinoma: a systematic review. Pancreatology 15(1):19–24
Amini N, Spolverato G, Gupta R, Margonis GA, Kim Y, Wagner D et al (2015) Impact total psoas volume on short- and long-term outcomes in patients undergoing curative resection for pancreatic adenocarcinoma: a new tool to assess sarcopenia. J Gastrointest Surg 19(9):1593–1602
Pecorelli N, Carrara G, De Cobelli F, Cristel G, Damascelli A, Balzano G et al (2016) Effect of sarcopenia and visceral obesity on mortality and pancreatic fistula following pancreatic cancer surgery. Br J Surg 103(4):434–442
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48(1):16–31
Chan MY, Chok KSH (2019) Sarcopenia in pancreatic cancer - effects on surgical outcomes and chemotherapy. World J Gastrointest Oncol 11(7):527–537
Simonsen C, de Heer P, Bjerre ED, Suetta C, Hojman P, Pedersen BK et al (2018) Sarcopenia and postoperative complication risk in gastrointestinal surgical oncology: a meta-analysis. Ann Surg 268(1):58–69
von Haehling S, Anker SD (2014) Prevalence, incidence and clinical impact of cachexia: facts and numbers-update 2014. J Cachexia Sarcopenia Muscle 5(4):261–263
Amundson JR, Williams JK, Benjamin AJ, Witmer HDD, Roggin KK (2020) The impact of sarcopenia on patients undergoing treatment for pancreatic ductal adenocarcinoma. Journal of Pancreatology 3(2):59–71
Pulvirenti A, Ramera M, Bassi C (2017) Modifications in the International Study Group for Pancreatic Surgery (ISGPS) definition of postoperative pancreatic fistula. Transl Gastroenterol Hepatol 2(12):107
Panwar R, Pal S (2017) The International Study Group of Pancreatic Surgery definition of delayed gastric emptying and the effects of various surgical modifications on the occurrence of delayed gastric emptying after pancreatoduodenectomy. HBPD INT 16(4):353–363
Zager Y, Khalilieh S, Ganaiem O, Gorgov E, Horesh N, Anteby R et al (2021) Low psoas muscle area is associated with postoperative complications in Crohn’s disease. Int J Colorectal Dis 36(3):543–550
Miyamoto Y, Baba Y, Sakamoto Y, Ohuchi M, Tokunaga R, Kurashige J et al (2015) Sarcopenia is a negative prognostic factor after curative resection of colorectal cancer. Ann Surg Oncol 22(8):2663–2668
Shin HE, Walston JD, Kim M, Won CW (2021) Sex-specific differences in the effect of free testosterone on sarcopenia components in older adults. Front Endocrinol (Lausanne) 22:12
Wang S, Xie H, Gong Y, Kuang J, Yan L, Ruan G et al (2020) The value of L3 skeletal muscle index in evaluating preoperative nutritional risk and long-term prognosis in colorectal cancer patients. Sci Rep 10(1):8153
Takagi K, Yagi T, Yoshida R, Umeda Y, Nobuoka D, Kuise T et al (2017) Sarcopenia predicts postoperative infection in patients undergoing hepato-biliary-pancreatic surgery. International Journal of Surgery Open 6:12–18
Makris K, Spanou L (2016) Acute kidney injury: definition, pathophysiology and clinical phenotypes. Clin Biochem Rev 37(2):85–98
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ et al (2013) Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol 31(12):1539–1547
Asbun HJ, Stauffer JA (2012) Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the Accordion Severity Grading System. J Am Coll Surg 215(6):810–819
Chua TC, Saxena A (2010) Extended pancreaticoduodenectomy with vascular resection for pancreatic cancer: a systematic review. J Gastrointest Surg 14(9):1442–1452
Pugalenthi A, Protic M, Gonen M, Kingham TP, Angelica MID, Dematteo RP et al (2016) Postoperative complications and overall survival after pancreaticoduodenectomy for pancreatic ductal adenocarcinoma. J Surg Oncol 113(2):188–193
Weber CE, Bock EA, Hurtuk MG, Abood GJ, Pickleman J, Shoup M et al (2014) Clinical and pathologic features influencing survival in patients undergoing pancreaticoduodenectomy for pancreatic adenocarcinoma. J Gastrointest Surg 18(2):340–347
Gouma DJ, van Geenen RC, van Gulik TM, de Haan RJ, de Wit LT, Busch OR et al (2000) Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg 232(6):786–795
Yu L, Huang Q, Xie F, Lin X, Liu C (2014) Risk factors of postoperative complications of pancreatoduodenectomy. Hepatogastroenterology 61(135):2091–2095
Ren S, Liu P, Zhou N, Dong J, Liu R, Ji W (2011) Complications after pancreaticoduodenectomy for pancreatic cancer: a retrospective study. Int Surg 96(3):220–227
Chen J-S, Liu G, Li T-R, Chen J-Y, Xu Q-M, Guo Y-Z et al (2019) Pancreatic fistula after pancreaticoduodenectomy: risk factors and preventive strategies. J Cancer Res Ther 15(4):857–863
Roberts KJ, Hodson J, Mehrzad H, Marudanayagam R, Sutcliffe RP, Muiesan P et al (2014) A preoperative predictive score of pancreatic fistula following pancreatoduodenectomy. HPB (Oxford) 16(7):620–628
Mogal H, Vermilion SA, Dodson R, Hsu F-C, Howerton R, Shen P et al (2017) Modified frailty index predicts morbidity and mortality after pancreaticoduodenectomy. Ann Surg Oncol 24(6):1714–1721
Benton K, Thomson I, Isenring E, Mark Smithers B, Agarwal E (2018) An investigation into the nutritional status of patients receiving an Enhanced Recovery After Surgery (ERAS) protocol versus standard care following oesophagectomy. Support Care Cancer 26(6):2057–2062
Braga M, Pecorelli N, Ariotti R, Capretti G, Greco M, Balzano G et al (2014) Enhanced recovery after surgery pathway in patients undergoing pancreaticoduodenectomy. World J Surg 38(11):2960–2966
Shintakuya R, Sasaki M, Nakamitsu A, Kohyama M, Tazaki T, Sugiyama Y et al (2019) Sarcopenia is an independent predictor of delayed gastric emptying following pancreaticoduodenectomy: a retrospective study. ANZ J Surg 89(10):E433–E437
Morley JE, Argiles JM, Evans WJ, Bhasin S, Cella D, Deutz NEP et al (2010) Nutritional recommendations for the management of sarcopenia. J Am Med Dir Assoc 11(6):391–396
Horowitz M, Neeman E, Sharon E, Ben-Eliyahu S (2015) Exploiting the critical perioperative period to improve long-term cancer outcomes. Nat Rev Clin Oncol 12(4):213–226
Roschel H, Hayashi AP, Fernandes AL, Jambassi-Filho JC, Hevia-Larraín V, de Capitani M et al (2021) Supplement-based nutritional strategies to tackle frailty: a multifactorial, double-blind, randomized placebo-controlled trial. Clin Nutr 40(8):4849–4858
Berkelmans GHK, Wilts BJW, Kouwenhoven EA, Kumagai K, Nilsson M, Weijs TJ et al (2016) Nutritional route in oesophageal resection trial II (NUTRIENT II): study protocol for a multicentre open-label randomised controlled trial. BMJ Open 6(8):e011979
van Dijk DPJ, van Woerden V, Cakir H, den Dulk M, Olde Damink SWM, Dejong CHC (2017) ERAS: improving outcome in the cachectic HPB patient. J Surg Oncol 116(5):617–622
Author information
Authors and Affiliations
Contributions
DON, HH, DM, EP, AN: data collection, data analysis, writing (original, review, and editing). AN, HL, CJY: resources, supervision, writing (review and editing).
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work accepted for presentation to the American College of Surgeons Clinical Congress, 10/23/2021 and Pancreas Club 11/11/2021.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nauheim, D.O., Hackbart, H., Papai, E. et al. Preoperative sarcopenia is a negative predictor for enhanced postoperative recovery after pancreaticoduodenectomy. Langenbecks Arch Surg 407, 2355–2362 (2022). https://doi.org/10.1007/s00423-022-02558-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02558-w