Abstract
Aims
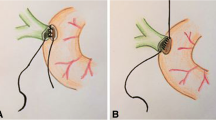
To compare outcomes of interrupted (IS) and continuous (CS) suturing techniques for Roux-en-Y hepaticojejunostomy and duct-to-duct choledochocholedochostomy.
Methods
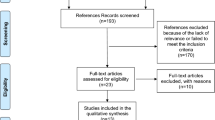
The study protocol was prospectively registered in PROSPERO (registration number: CRD42021286294). A systematic search of MEDLINE, CENTRAL, and Web of Science and bibliographic reference lists were conducted (last search: 14th March 2022). All comparative studies reporting outcomes of IS and CS in hepaticojejunostomy and choledochocholedochostomy were included and their risk of bias was assessed using ROBINS-I tool. Overall biliary complications, bile leak, biliary stricture, cholangitis, liver abscess, and anastomosis time were the evaluated outcome parameters.
Results
Ten comparative studies (2 prospective and 8 retrospective) were included which reported 1617 patients of whom 1186 patients underwent Roux-en-Y hepaticojejunostomy (IS: 789, CS: 397) and the remaining 431 patients underwent duct-to-duct choledochocholedochostomy (IS: 168, CS: 263). Although use of IS for hepaticojejunostomy was associated with significantly longer anastomosis time (MD: 14.15 min, p=0.0002) compared to CS, there was no significant difference in overall biliary complications (OR: 1.34, p=0.11), bile leak (OR: 1.64, p=0.14), biliary stricture (OR: 0.84, p=0.65), cholangitis (OR: 1.54, p=0.35), or liver abscess (OR: 0.58, p=0.40) between two groups. Similarly, use of IS for choledochocholedochostomy was associated with no significant difference in risk of overall biliary complications (OR: 0.92, p=0.90), bile leak (OR: 1.70, p=0.28), or biliary stricture (OR: 1.07, p=0.92) compared to CS.
Conclusions
Interrupted and continuous suturing techniques for Roux-en-Y hepaticojejunostomy or duct-to-duct choledochocholedochostomy seem to have comparable clinical outcomes. The available evidence may be subject to confounding by indication with respect to diameter of bile duct. Future high-quality research is encouraged to report the outcomes with respect to duct diameter and suture material.





Similar content being viewed by others
References
Hirano S, Tanaka E, Tsuchikawa T et al (2012) Techniques of biliary reconstruction following bile duct resection (with video). J Hepatobiliary Pancreat Sci. 19(3):203–209. https://doi.org/10.1007/s00534-011-0475-5
Akamatsu N, Sugawara Y, Hashimoto D (2011) Biliary reconstruction, its complications and management of biliary complications after adult liver transplantation: a systematic review of the incidence, risk factors and outcome. Transpl Int. 24:379–392
Chok KS, Ng KK, Poon RT et al (2009) Impact of postoperative complications on long-term outcome of curative resection for hepatocellular carcinoma. Br J Surg. 96:81–87
Sondenaa K, Kubota K, Sano K et al (2004) Successful reconstruction of segmental or subsegmental bile ducts after resection of hilar bile ducts: short- and long-term results. Hepatogastroenterology. 51:1278–1281
Nagino M, Nishio H, Ebata T et al (2007) Intrahepatic cholangiojejunostomy following hepatobiliary resection. Br J Surg. 94:70–77
Antolovic D, Koch M, Galindo L et al (2007) Hepaticojejunostomy—analysis of risk factors for postoperative bile leaks and surgical complications. J Gastrointest Surg. 11:555–561
Hasegawa K, Kokudo N, Imamura H et al (2004) Bilioenteric reconstruction for small bile ducts without mucosa-to-mucosa alignment: long-term results. Arch Surg. 139:1050–1054
Tsui TY, Schlitt HJ, Obed A (2011) Prospective evaluation of biliary reconstruction with duct-to-duct continuous suture in adult live donor liver transplantation. Langenbecks Arch Surg. 396(2):209–215
Brunner M, Stockheim J, Krautz C et al (2018) Continuous or interrupted suture technique for hepaticojejunostomy? A national survey. BMC Surg. 18(1):84
Asano T, Natsume S, Senda Y et al (2016) Incidence and risk factors for anastomotic stenosis of continuous hepaticojejunostomy after pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 23(10):628–635
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 339:b2700
DeMatteo RP, Büchler MW, Weitz J (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 149(5):680–688
Kalkum E, Klotz R, Seide S et al (2021) Systematic reviews in surgery-recommendations from the Study Center of the German Society of Surgery. Langenbecks Arch Surg. 406(6):1723–1731
Sterne JA, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919
Wan X, Wang W, Liu J et al (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135
Higgins JPT, Thomas J, Chandler J et al (2020) Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook. Last Accessed: 15/10/2021
Saxena R, Ghosh NK, Galodha S (2021) Economics and safety of continuous and interrupted suture hepaticojejunostomy: an audit of 556 surgeries. Ann Hepatobiliary Pancreat Surg. 25(4):472–476
Natsume S, Shimizu Y, Okuno M et al (2021) Continuous suture is a risk factor for benign hepaticojejunostomy stenosis after pancreatoduodenectomy in patients with a non-dilated bile duct. HPB (Oxford). S1365-182X(21)00110-6
Hamid MA, Rady MA, Abd-El Razik MA (2020) Interrupted versus continuous suturing techniques in hepaticojejunostomy, a retrospective study. J Am Sci. 16(2)
Tatsuguchi T, Takahashi H, Akita H et al (2018) Short- and long-term outcomes of choledochojejunostomy during pancreaticoduodenectomy and total pancreatectomy: interrupted suture versus continuous suture. Langenbecks Arch Surg. 403(8):959–966
Galodha S, Saxena R (2016) Economic and safety implications of continuous versus interrupted suturing method of hepaticojejunostomy: a prospective study. HPB 18:e495
Leiting J, Arain M, Freeman ML et al (2016) Minerva Chir. 71(1):15–24
Castaldo ET, Pinson CW, Feurer ID et al (2007) Continuous versus interrupted suture for end-to-end biliary anastomosis during liver transplantation gives equal results. Liver Transpl. 13(2):234–238. https://doi.org/10.1002/lt.20986
Kasahara M, Egawa H, Takada Y et al (2006) Biliary reconstruction in right lobe living-donor liver transplantation: comparison of different techniques in 321 recipients. Ann Surg. 243(4):559–566
Soejima Y, Taketomi A, Yoshizumi T et al (2006) Biliary strictures in living donor liver transplantation: incidence, management, and technical evolution. Liver Transpl. 12(6):979–986
Ishiko T, Egawa H, Kasahara M et al (2002) Duct-to-duct biliary reconstruction in living donor liver transplantation utilizing right lobe graft. Ann Surg. 236(2):235–240
Antolovic D, Koch M, Galindo L et al (2007) Hepaticojejunostomy--analysis of risk factors for postoperative bile leaks and surgical complications. J Gastrointest Surg. 11(5):555–561
de Castro SM, Kuhlmann KF, Busch OR et al (2005) Incidence and management of biliary leakage after hepaticojejunostomy. J Gastrointest Surg 9(8):1163–71. discussion 1171-3
Hisatsune H, Yazumi S, Egawa H et al (2003) Endoscopic management of biliary strictures after duct-to-duct biliary reconstruction in right-lobe living donor liver transplantation. Transplantation. 76:810–815
Trotter JF, Wachs M, Everson GT et al (2002) Adult-to-adult transplantation of the right hepatic lobe from a living donor. N Engl J Med. 346:1074–1082
Qian YB, Liu CL, Lo CM et al (2004) Risk factors for biliary reconstructions after liver transplantation. Arch Surg. 139:1101–1105
Abdullah K, Abdeldayem H, Hali WO (2005) Incidence and management of biliary complications after orthotopic liver transplantation: ten years’ experience at King Fahad National Guard Hospital. Transplant Proc. 37:3179–3181
Salahi H, Razmkon A, Mehdizadeh AR et al (2005) Biliary tract complications after liver transplantation at a single center. Transplant Proc 37:3177–3178
Thuluvath PJ, Pfau PR, Kimmey MB et al (2005) Biliary complications after liver transplantation: the role of endoscopy. Endoscopy 37:857-863
Duconseil P, Turrini O, Ewald J et al (2014) Biliary complications after pancreaticoduodenectomy: skinny bile ducts are surgeons’ enemies. World J Surg. 38(11):2946–2951
Ito T, Sugiura T, Okamura Y et al (2018) Late benign biliary complications after pancreatoduodenectomy. Surgery. 163(6):1295–1300
Kim JM, Cho W, Kwon CHD et al (2014) Bile duct reconstruction by a young surgeon in living donor liver transplantation using right liver graft. Medicine (Baltimore) 93(14):e84
Author information
Authors and Affiliations
Contributions
Shahin Hajibandeh and Shahab Hajibandeh equally contributed to this paper and joined first authorship is proposed.
Corresponding author
Ethics declarations
Ethical approval
Considering the design of our study, ethical approval and consent were not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Search No | Search strategy* |
|---|---|
#1 | MeSH descriptor: [hepaticojejunostomy] explode all trees |
#2 | hepaticojejunostomy : TI,AB,KW |
#3 | MeSH descriptor: [choledochocholedochostomy] explode all trees |
#4 | choledochocholedochostomy : TI,AB,KW |
#5 | #1 OR #2 OR #3 OR #4 |
#6 | MeSH descriptor: [interrupted ] explode all trees |
#7 | interrupted : TI,AB,KW |
#8 | MeSH descriptor: [continuous] explode all trees |
#9 | continuous: TI,AB,KW |
#10 | suture: TI,AB,KW |
#11 | suturing : TI,AB,KW |
#12 | #6 OR #7 OR #8 OR #9 OR 10 OR #11 |
#13 | #5 AND #12 |
Appendix 2. Excluded studies
-
1-
Brunner M, Stockheim J, Krautz C, et al. (2018) Continuous or interrupted suture technique for hepaticojejunostomy? A national survey. BMC Surg. 11;18(1):84.
-
2-
Ando H, Kaneko K, Ono Y, et al. (2011). Biliary reconstruction with wide-interval interrupted suture to prevent biliary complications in pediatric living-donor liver transplantation. J Hepatobiliary Pancreat Sci. 18(1):26-31.
-
3-
Ikegami T, Nishizaki T, Kishikawa K, Nomoto K, Uchiyama H, Ohta R, Hiroshige S, Sugimachi K. Biliary reconstruction in living donor liver transplantation with dye injection leakage test and without stent use. Hepatogastroenterology. 2001 Nov-Dec;48(42):1582-4.
-
4-
Nagakawa Y, Kozono S, Takishita C, et al. (2021) Incidence of anastomotic stricture after hepaticojejunostomy with continuous sutures in patients who underwent laparoscopic pancreaticoduodenectomy. Surg Today. 2021 Jul;51(7):1212-1219.
-
5-
Li G, Yuan L, Yu G, Xu Y, Liu J (2020) A Modified Suture Technique in Hepaticojejunostomy. Med Sci Monit.;26:e921896. doi: 10.12659/MSM.921896. PMID: 32189715.
-
6-
Asano T, Natsume S, Senda Y, et al. (2016) Incidence and risk factors for anastomotic stenosis of continuous hepaticojejunostomy after pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci 23:628–635
-
7-
Jafari A, Stoffels B, Kalff JC, Manekeller S. An Improved Suture Technique for Perform Biliary Reconstruction in Orthotopic Liver Transplantation. Ann Transplant. 2016 Jan 14;21:25-9. doi: 10.12659/aot.894692. PMID: 26763574.
Rights and permissions
About this article
Cite this article
Hajibandeh, S., Hajibandeh, S., Parente, A. et al. Meta-analysis of interrupted versus continuous suturing for Roux-en-Y hepaticojejunostomy and duct-to-duct choledochocholedochostomy. Langenbecks Arch Surg 407, 1817–1829 (2022). https://doi.org/10.1007/s00423-022-02548-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02548-y