Abstract
Purpose
Metabolic and bariatric surgery (MBS) remains a safe and effective treatment for morbid obesity with a low-risk profile. Venous thromboembolism (VTE) remains the most common cause of mortality. There is increasing consensus that inferior vena cava (IVC) filter use is associated with more harm than benefit. Our study aim was to determine if the timing of IVC filter placement correlates with VTE complications.
Methods
The 2015–2019 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program databases were used to identify Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) patients who had an IVC filter at the time of bariatric procedure. Selected cases were stratified by IVC placement timing. Propensity-score matching estimated the probabilities of receiving pre-existing vs. prophylactic IVC placement. Resultant models were then used to assess VTE complications. Statistical analyses were performed with Stata MP version 16. A p-value < 0.05 was considered significant.
Results
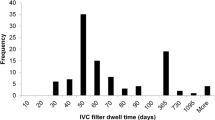
In total, 228,986 RYGB and 568,386 SG cases were analyzed, and 0.6% and 0.5% had an IVC filter. Prophylactic IVC filter use declined annually, but not pre-existing filters. VTE and VTE-related mortality were significantly higher in filter vs. no filter cohorts (p<0.001). Propensity matching reduced biases between RYGB and SG IVC filter cohorts (pre-existing vs. prophylactic). There were no differences in the RYGB pre-existing and prophylactic IVC filter cohorts; however; for SG cases, pre-existing IVC filters compared to prophylactic IVC filters were associated with decreased odds of having a VTE (OR: 0.97, 95% CI: 0.95, 0.99).
Conclusion
Compared to a pre-existing filter, the presence of a prophylactic IVC filter in SG patients was associated with a higher likelihood of VTE.
Highlights
1. Annual use of prophylactic IVC filter is bariatric surgery patients is decreasing.
2. The presence of a pre-existing IVC filter remain constant.
3. Any IVC filter presence at time of MBS increased VTE and VTE-related mortality and morbidity.
4. In SG cases, prophylactic IVC filter was associated with higher rates of VTE and VTE-related mortality.


Similar content being viewed by others
References
Arterburn D et al (2018) Comparative effectiveness and safety of bariatric procedures for weight loss: a PCORnet cohort study. Ann Intern Med 169(11):741–750
Bilha SC et al (2018) The effects of bariatric surgery on renal outcomes: a systematic review and meta-analysis. Obes Surg 28(12):3815–3833
Chang SH et al (2014) The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012. JAMA Surg 149(3):275–87
Inge TH et al (2018) Comparative effectiveness of bariatric procedures among adolescents: the PCORnet bariatric study. Surg Obes Relat Dis 14(9):1374–1386
McTigue KM et al (2020) Comparing the 5-year diabetes outcomes of sleeve gastrectomy and gastric bypass: the National Patient-Centered Clinical Research Network (PCORNet) Bariatric Study. JAMA Surg 155(5):e200087
Sheng B et al (2017) The long-term effects of bariatric surgery on type 2 diabetes remission, microvascular and macrovascular complications, and mortality: a systematic review and meta-analysis. Obes Surg 27(10):2724–2732
Froehling DA et al (2013) Incidence of venous thromboembolism after bariatric surgery: a population-based cohort study. Obes Surg 23(11):1874–9
Winegar DA et al (2011) Venous thromboembolism after bariatric surgery performed by Bariatric Surgery Center of Excellence Participants: analysis of the Bariatric Outcomes Longitudinal Database. Surg Obes Relat Dis 7(2):181–8
Stein PD, Matta F (2013) Pulmonary embolism and deep venous thrombosis following bariatric surgery. Obes Surg 23(5):663–8
Dang JT et al (2019) Predicting venous thromboembolism following laparoscopic bariatric surgery: development of the BariClot tool using the MBSAQIP database. Surg Endosc 33(3):821–831
Altieri MS et al (2018) Evaluation of VTE prophylaxis and the impact of alternate regimens on postoperativepost-operative bleeding and thrombotic complications following bariatric procedures. Surg Endosc 32(12):4805–4812
Daigle CR et al (2018) Which postoperativepostoperative complications matter most after bariatric surgery? Prioritizing quality improvement efforts to improve national outcomes. Surg Obes Relat Dis 14(5):652–657
Kaw R et al (2014) Inferior vena cava filters and postoperativepostoperative outcomes in patients undergoing bariatric surgery: a meta-analysis. Surg Obes Relat Dis 10(4):725–33
Obeid FN, et al. (2007) Efficacy of prophylactic inferior vena cava filter placement in bariatric surgery. Surg Obes Relat Dis 3(6):606–608 discussion 609-10
Trigilio-Black CM et al (2007) Inferior vena cava filter placement for pulmonary embolism risk reduction in super morbidly obese undergoing bariatric surgery. Surg Obes Relat Dis 3(4):461–4
Sheu AY et al (2018) Prophylactic IVC filter placement in bariatric surgery patients: results from a prospective filter registry. CVIR Endovasc 1(1):13
Birkmeyer NJ et al (2013) Risks and benefits of prophylactic inferior vena cava filters in patients undergoing bariatric surgery. J Hosp Med 8(4):173–7
Reddy S et al (2019) Prophylactic inferior vena cava filters prior to bariatric surgery: insights from the national inpatient sample. JACC Cardiovasc Interv 12(12):1153–1160
Mechanick JI, Apovian C, Bretehauer S et al (2019) Clinical practice guidelines for perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures - 2019 update: co-sponsored by american association of clnical endocrinologist/american college of endocrinology, the obesity society, american society for metabolic & bariatric surgery, obesity medicine association, and american society of anesthesiologist- executive summary. Endocr Pract. 25(12):1346–1359
Edwards MA, Mazzei M, Zhao H, Reddy S, Bashir R (2021) Racial disparities in inferior vena cava filter use in metabolic and bariatric surgery patients: nationwide insights from the MBSAQIP database. Am J Surg. 221(4):749–758
U.S. Food and Drug Administration. Inferior vena cava (IVC) filters: initial communication: risk of adverse events with long term use. Available at: https://wayback.archiveit.org/7993/20170112165620/http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm221707.htm, Accessed 24th Apr 2018
U.S. Food and Drug Administration. Removing retrievable inferior vena cava filters: FDA safety communication. Available at:https://wayback.archiveit.org/7993/20170404182212/https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm396377.htm, Accessed 27th Apr 2018
Mohapatra A, Liang NL, Chaer RA, Tzeng E (2019) Persistently low inferior vena cava filter retrieval rates in a population-based cohort. J Vasc Surg 7(1):38–44
Angel LF, Tapson V, Galgon RE, Restrepo MI, Kaufman JM (2011) Systematic review of the use of retrievable inferior vena cava filters. J Vasc Interv Radiol 22:1522–1530
Lambe BD, Bedway JJ, Friedell ML (2013) Percutaneous femoral vein access for inferior vena cava filter placement does not cause insertion-site thrombosis. Ann Vasc Surg 27:1169
Gorman PH, Qadri SF, Rao-Patel A (2009) Prophylactic inferior vena cava (IVC) filter placement may increase the relative risk of deep venous thrombosis after acute spinal cord injury. J Trauma 66:707
Decousus H, Leizorovicz A, Parent F, et al. (1998) A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d’Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med 338:409
PREPIC Study Group (2005) Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d’Embolie Pulmonaire par Interruption Cave) randomized study. Circulation 112:416
Blebea J, Wilson R, Waybill P et al (1999) Deep venous thrombosis after percutaneous insertion of vena caval filters. J Vasc Surg 30:821
Garrido MM, KA, Paris J, et al. (2014) Methods for constructing and assessing propensity scores. Health Serv Res 49(5):1701–1720
Reeve BB, Smith AW, Arora NK, Hays RD (2008) Reducing bais in cancer research: application of propensity score matching. Health Care Financ Rev 29(4):69080
Comes RF, Mismetti P, Afshari A, ESA VTE Task Force (2018) European guideline on perioperative venous thromboembolism prophylaxis: inferior vena cava filters. Eur J Anaesthesiol 35(2):108–111
Mesmetti P, Laporte S, Pellerin O et al (2015) Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism: a randomized clinical trial. JAMA 313(16):1627–35
Kearon C, Akl EA, Ornelas J et al (2016) Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 149(2):315–325
Haskins IN, Rivas L, Ju T et al (2019) The association of IVC filter placement with the incidence of postoperative pulmonary embolism following laparoscopic bariatric surgery: an analysis of the the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Project. Surg Obes Relat Dis. 15(1):109–115
Acevedo E, Mazzei M, Zhao H, Lu X, Soans R, Edwards MA (2020) Outcomes in conventional laparoscopic versus robotic-assisted primary bariatric surgery: a retrospective, case–controlled study of the MBSAQIP database. Surg Endosc 34:1353–1365
Author information
Authors and Affiliations
Contributions
Study conception and design: Dr. Michael Edwards. Acquisition of data: Dr. Michael Edwards. Analysis and interpretation of data: Dr. Aaron Spaulding and Dr. Michael Edwards. Drafting of manuscript: Dr. Michael Edwards. Critical revision of manuscript: Dr. Aaron Spaulding.
Corresponding author
Ethics declarations
Statement of human and animal rights
For this type of study using a national deidentified dataset, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Edwards, M.A., Spaulding, A.C. Does timing of IVC filter placement in bariatric surgery patients impact perioperative outcomes?. Langenbecks Arch Surg 407, 2327–2335 (2022). https://doi.org/10.1007/s00423-022-02532-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02532-6