Abstract
Background
Although a temporary stoma can mitigate the severity of anastomotic leakage, some rectal cancer patients retain a permanent stoma after sphincter-preserving surgery. Therefore, this study aimed to identify independent preoperative risk factors for permanent stoma and establish a prediction model for mid-and low-rectal cancer patients who underwent sphincter-preserving surgery and temporary stoma.
Methods
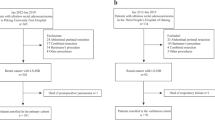
We retrospectively reviewed consecutive patients with non-metastatic rectal cancer between 2000 and 2015. The risk factors for permanent stomas were collected and analyzed.
Results
A total of 1020 rectal cancer patients with temporary stoma were included. The overall rate of permanent stoma was 17.5% (n = 179). Cancer progression and anastomotic complications are major causes of permanent stomas. Multivariate analysis showed that preoperative risk factors such as advanced age, male sex, preoperative CEA ≥ 10 ng/ml, T4 stage, N stage, low rectal tumor, and ASA ≥ III were independent preoperative risk factors after adjustment. The ROC curve of the risk factors and permanent stoma showed an AUC of 0.689, a cut-off value of 2.5, a sensitivity of 0.689, and a specificity of 0.622. The permanent stoma rates were significantly higher between risk scores ≤ 2 and > 2 (29.9% vs. 11.3%, p < 0.001).
Conclusion
Preoperative CEA ≥ 10 ng/ml, T4 stage, N stage, low rectal tumor, advanced age, ASA ≥ III, and male sex were independent preoperative prognostic factors for a permanent stoma. The risk was higher with a score greater than two. Therefore, the risk of subsequent permanent stoma should be evaluated and informed to the patient prior to the primary surgery.




Similar content being viewed by others
Availability of data and material
The de-identified data and material are available after the approval of the Chang Gung Medical Foundation Institutional Review Board.
Code availability
There is no software application or custom code.
References
Onaitis MW, Noone RB, Hartwig M et al (2001) Neoadjuvant chemoradiation for rectal cancer: analysis of clinical outcomes from a 13-year institutional experience. Ann Surg 233(6):778. https://doi.org/10.1097/00000658-200106000-00007
Matthiessen P, Hallbook O, Andersson M et al (2004) Risk factors for anastomotic leakage after anterior resection of the rectum. Colorectal Dis 6(6):462–469. https://doi.org/10.1111/j.1463-1318.2004.00657.x
Eberl T, Jagoditsch M, Klingler A et al (2008) Risk factors for anastomotic leakage after resection for rectal cancer. Am J Surg 196(4):592–598. https://doi.org/10.1016/j.amjsurg.2007.10.023
Huser N, Michalski CW, Erkan M et al (2008) Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg 248(1):52–60. https://doi.org/10.1097/SLA.0b013e318176bf65
Tan WS, Tang CL, Shi L et al (2009) Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Br J Surg 96(5):462–472. https://doi.org/10.1002/bjs.6594
Neuman HB, Patil S, Fuzesi S et al (2011) Impact of a temporary stoma on the quality of life of rectal cancer patients undergoing treatment. Ann Surg Oncol 18(5):1397–1403. https://doi.org/10.1245/s10434-010-1446-9
Seo SI, Yu CS, Kim GS et al (2013) Characteristics and risk factors associated with permanent stomas after sphincter-saving resection for rectal cancer. World J Surg 37(10):2490–2496. https://doi.org/10.1007/s00268-013-2145-z
den Dulk M, Smit M, Peeters KC et al (2007) A multivariate analysis of limiting factors for stoma reversal in patients with rectal cancer entered into the total mesorectal excision (TME) trial: a retrospective study. Lancet Oncol 8(4):297–303. https://doi.org/10.1016/S1470-2045(07)70047-5
Junginger T, Gonner U, Trinh TT et al (2010) Permanent stoma after low anterior resection for rectal cancer. Dis Colon Rectum 53(12):1632–1639. https://doi.org/10.1007/DCR.0b013e3181ed0aae
David G, Slavin J, Willmott S et al (2010) Loop ileostomy following anterior resection: is it really temporary? Colorectal Dis 12(5):428–432. https://doi.org/10.1111/j.1463-1318.2009.01815.x
Lindgren R, Hallböök O, Rutegård J et al (2011) What is the risk for a permanent stoma after low anterior resection of the rectum for cancer? A six-year follow-up of a multicenter trial. Dis Colon Rectum 54(1):41–47. https://doi.org/10.1007/DCR.0b013e3181fd2948
Lim SW, Kim HJ, Kim CH et al (2013) Risk factors for permanent stoma after low anterior resection for rectal cancer. Langenbecks Arch Surg 398(2):259–264. https://doi.org/10.1007/s00423-012-1038-1
Dinnewitzer A, Jager T, Nawara C et al (2013) Cumulative incidence of permanent stoma after sphincter preserving low anterior resection of mid and low rectal cancer. Dis Colon Rectum 56(10):1134–1142. https://doi.org/10.1097/DCR.0b013e31829ef472
Pan HD, Peng YF, Wang L et al (2016) Risk factors for nonclosure of a temporary defunctioning ileostomy following anterior resection of rectal cancer. Dis Colon Rectum 59(2):94–100. https://doi.org/10.1097/DCR.0000000000000520
Kim MJ, Kim YS, Park SC et al (2016) Risk factors for permanent stoma after rectal cancer surgery with temporary ileostomy. Surgery 159(3):721–727. https://doi.org/10.1016/j.surg.2015.09.011
Celerier B, Denost Q, Van Geluwe B et al (2016) The risk of definitive stoma formation at 10 years after low and ultralow anterior resection for rectal cancer. Colorectal Dis 18(1):59–66. https://doi.org/10.1111/codi.13124
Zhou X, Wang B, Li F et al (2017) Risk factors associated with nonclosure of defunctioning stomas after sphincter-preserving low anterior resection of rectal cancer: a meta-analysis. Dis Colon Rectum 60(5):544–554. https://doi.org/10.1097/DCR.0000000000000819
Song O, Kim KH, Lee SY et al (2018) Risk factors of stoma re-creation after closure of diverting ileostomy in patients with rectal cancer who underwent low anterior resection or intersphincteric resection with loop ileostomy. Ann Surg Treat Res 94(4):203–208. https://doi.org/10.4174/astr.2018.94.4.203
Kim S, Kim MH, Oh JH et al (2020) Predictors of permanent stoma creation in patients with mid or low rectal cancer: results of a multicentre cohort study with preoperative evaluation of anal function. Colorectal Dis 22(4):399–407. https://doi.org/10.1111/codi.14898
Peeters KC, Tollenaar RA, Marijnen CA et al (2005) Risk factors for anastomotic failure after total mesorectal excision of rectal cancer. Br J Surg 92(2):211–216. https://doi.org/10.1002/bjs.4806
You J-F, Tang R, Changchien CR et al (2009) Effect of body mass index on the outcome of patients with rectal cancer receiving curative anterior resection: disparity between the upper and lower rectum. Ann Surg 249(5):783–787. https://doi.org/10.1097/SLA.0b013e3181a3e52b
Mirnezami A, Mirnezami R, Chandrakumaran K et al (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 253(5):890–899. https://doi.org/10.1097/SLA.0b013e3182128929
Yang J, Chen Q, Jindou L et al (2020) The influence of anastomotic leakage for rectal cancer oncologic outcome: a systematic review and meta-analysis. J Surg Oncol 121(8):1283–1297. https://doi.org/10.1002/jso.25921
Alonso S, Pascual M, Salvans S et al (2015) Postoperative intra-abdominal infection and colorectal cancer recurrence: a prospective matched cohort study of inflammatory and angiogenic responses as mechanisms involved in this association. Eur J Surg Oncol (EJSO) 41(2):208–214. https://doi.org/10.1016/j.ejso.2014.10.052
Peeters CF, de Waal RM, Wobbes T et al (2008) Metastatic dormancy imposed by the primary tumor: does it exist in humans? Ann Surg Oncol 15(11):3308–3315. https://doi.org/10.1245/s10434-008-0029-5
Klink CD, Lioupis K, Binnebösel M et al (2011) Diversion stoma after colorectal surgery: loop colostomy or ileostomy? Int J Colorectal Dis 26(4):431–436. https://doi.org/10.1007/s00384-010-1123-2
Chudner A, Gachabayov M, Dyatlov A et al (2019) The influence of diverting loop ileostomy vs. colostomy on postoperative morbidity in restorative anterior resection for rectal cancer: a systematic review and meta-analysis. Langenbeck’s Arch Surg 404(2):129–139. https://doi.org/10.1007/s00423-019-01758-1
Güenaga KF, Lustosa SA, Saad SS et al (2007) Ileostomy or colostomy for temporary decompression of colorectal anastomosis. Cochrane Database Syst Rev (1). https://doi.org/10.1002/14651858.CD004647.pub2
Law W, Chu K, Choi H (2002) Randomized clinical trial comparing loop ileostomy and loop transverse colostomy for faecal diversion following total mesorectal excision. J Br Surg 89(6):704–708. https://doi.org/10.1046/j.1365-2168.2002.02082.x
Huang S-H, Tsai W-S, You J-F et al (2019) Preoperative carcinoembryonic antigen as a poor prognostic factor in stage I-III colorectal cancer after curative-intent resection: a propensity score matching analysis. Ann Surg Oncol 26(6):1685–1694. https://doi.org/10.1245/s10434-019-07184-3
Yoon SM, Kim DY, Kim TH et al (2007) Clinical parameters predicting pathologic tumor response after preoperative chemoradiotherapy for rectal cancer. Int J Radiat Oncol Biol Phys 69(4):1167–1172. https://doi.org/10.1016/j.ijrobp.2007.04.047
Park YA, Lee KY, Kim NK et al (2006) Prognostic effect of perioperative change of serum carcinoembryonic antigen level: a useful tool for detection of systemic recurrence in rectal cancer. Ann Surg Oncol 13(5):645–650. https://doi.org/10.1245/ASO.2006.03.090
García VM, Cejas P, Codesido MB et al (2009) Prognostic value of carcinoembryonic antigen level in rectal cancer treated with neoadjuvant chemoradiotherapy. Int J Colorectal Dis 24(7):741–748. https://doi.org/10.1007/s00384-009-0682-6
Hong Y, Ghuman A, Poh KS et al (2021) Can normalized carcinoembryonic antigen following neoadjuvant chemoradiation predict tumour recurrence after curative resection for locally advanced rectal cancer? Colorectal Dis. https://doi.org/10.1111/codi.15583
van Gijn W, Marijnen CA, Nagtegaal ID et al (2011) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 12(6):575–582. https://doi.org/10.1016/S1470-2045(11)70097-3
Sauer R, Becker H, Hohenberger W et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351(17):1731–1740. https://doi.org/10.1056/NEJMoa040694
Qin Q, Ma T, Deng Y et al (2016) Impact of preoperative radiotherapy on anastomotic leakage and stenosis after rectal cancer resection: post hoc analysis of a randomized controlled trial. Dis Colon Rectum 59(10):934–942. https://doi.org/10.1097/DCR.0000000000000665
Petrelli F, Trevisan F, Cabiddu M et al (2020) Total neoadjuvant therapy in rectal cancer: a systematic review and meta-analysis of treatment outcomes. Ann Surg 271(3):440–448. https://doi.org/10.1097/SLA.0000000000003471
Bahadoer RR, Dijkstra EA, van Etten B et al (2021) Short-course radiotherapy followed by chemotherapy before total mesorectal excision (TME) versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO): a randomised, open-label, phase 3 trial. Lancet Oncol 22(1):29–42. https://doi.org/10.1016/S1470-2045(20)30555-6
Ngan SY, Burmeister B, Fisher RJ et al (2012) Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group trial 01.04. J Clin Oncol 30(31):3827–33. https://doi.org/10.1200/JCO.2012.42.9597
Kim DJ, Kim JH, Lim JS et al (2010) Restaging of rectal cancer with MR imaging after concurrent chemotherapy and radiation therapy. Radiographics 30(2):503–516. https://doi.org/10.1148/rg.302095046
Funding
This study was supported by the Chang Gung Medical Research Fund (CORPG3F0321).
Author information
Authors and Affiliations
Contributions
Wen-Sy Tsai and Shu-Huan Huang had full access to all the data in the study and took responsibility for the integrity of the data and accuracy of the data analysis. Study concept and design: Shu-Huan Huang, Kun-Yu Tsai, and Wen-Sy Tsai. Acquisition of data: all the authors. Drafting of the manuscript: Kun-Yu Tsai and Shu-Huan Huang. Critical revision of the manuscript for important: intellectual content: Jeng-Fu You and Chien-Yuh Yeh. Statistical analysis: Shu-Huan Huang and Kun-Yu Tsai. Administrative, technical, or material support: Tzongyun Tsai and Jeng-Fu You. Study supervision: Wen-Sy Tsai.
Corresponding author
Ethics declarations
Ethics approval
IRB approval was obtained from the Chang Gung Medical Foundation Institutional Review Board (IRB No. 202001577B0).
Consent to participate
A retrospective study with de-identified data required no consent to participate.
Consent for publication
All the authors reviewed and approved the final version of the manuscript.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Huang, SH., Tsai, KY., Tsai, Ty. et al. Preoperative risk stratification of permanent stoma in patients with non-metastatic mid and low rectal cancer undergoing curative resection and a temporary stoma. Langenbecks Arch Surg 407, 1991–1999 (2022). https://doi.org/10.1007/s00423-022-02503-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02503-x