Abstract
Purpose
Multimodal prehabilitation aims to prepare frail older patients for major surgery. The objective of this review is to determine the benefits of pre-operative multimodal prehabilitation compared to standard care in older patients.
Methods
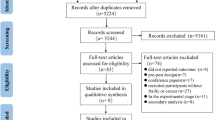
Data sources included MEDLINE, EMBASE, CENTRAL, CINAHL and PsychINFO. They were searched from inception to September 2021. Only randomized controlled trials (RCT) with an average study population age ≥ 65 that had undergone major abdominal operation with at least two components (physical, nutritional, psychological) of prehabilitation programs were included.
Results
Nine RCTs were included with a total of 823 patients, of whom 705 completed the study with 358 undergoing prehabilitation and 347 were controls. Significantly lower complications were observed in the prehabilitation group compared to control (OR 0.67; 95% CI 0.46 to 0.99; p = 0.04; I2 = 32%). A significant increase in 6-min walking distance (6MWD) from baseline to immediately prior to surgery (mean difference 35.1 m; 95%CI 11.6–58.4; p = 0.003; I2 = 67%) and 8 weeks post-surgery (mean difference 44.9 m; 95%CI 6.0–83.8; p = 0.02; I2 = 75%) was noted in the prehabilitation group. No difference was observed in length of stay (OR 0.59; 95% CI − 0.23 to 1.40; p = 0.16; I2 = 91%) or 30-day emergency department visit (OR 0.72; 95% CI 0.41 to 1.26; p = 0.25; I2 = 0%). Patient reported outcome measures were not significantly different.
Conclusions
Amongst older patients, multimodal prehabilitation increases peri-operative functional capacity and may potentially decrease post-operative complications. Future studies should continue to focus on older patients who are frail as this is the group that prehabilitation would likely have a clinically significant impact on.





Similar content being viewed by others
References
World Health Organization, Geneva: Switzerland (2015) Ageing and health. Accessed 17 April 2021. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health#:~:text=People%20worldwide%20are%20living%20longer,aged%2080%20years%20or%20older
You W, Henneberg M (2017) Cancer incidence increasing globally: the role of relaxed natural selection. Evol Appl 11(2):140–152
Takahashi K, Matsumoto H, Yamaguchi T et al (2010) Surgery for colorectal cancer in elderly patients. Gan To Kagaku Ryoho 37(13):2823–2828
Tan KY, Kawamura YJ, Tokomitsu A et al (2012) Assessment for frailty is useful for predicting morbidity in elderly patients undergoing colorectal cancer resection whose comorbidities are already optimized. Am J Surg 204(2):139–143
Kolarsick PA, Sacchi M, Spinelli A et al (2020) Minimizing the impact of colorectal surgery in the older patient: the role of minimally invasive surgery in the geriatric population. Eur J Surg Oncol 46(3):333–337
Ryan AM, Power DG, Daly et al (2016) Cancer-associated malnutrition, cachexia and sarcopenia: the skeleton in the hospital closet 40 years later. Proc Nutr Soc 75(2):199–211
Al-Refaie WB, Parsons HM, Henderson WG et al (2010) Major cancer surgery in the elderly: results from the American College of Surgeons National Surgical Quality Improvement Program. Ann Surg 251(2):311–318
Morley JE, Vellas B, van Kan GA et al (2013) Frailty consensus: a call to action. J Am Med Dir Assoc 14(6):392–397
Kow AW (2019) Prehabilitation and its role in geriatric surgery. Ann Acad Med Singap 48(11):386–392
Howard R, Yin YS, McCandless L et al (2019) Taking control of your surgery: impact of a prehabilitation program on major abdominal surgery. J Am Coll Surg 228(1):72–80
Santa Mina D, Clarke H, Ritvo P et al (2014) Effect of total-body prehabilitation on postoperative outcomes: a systematic review and meta-analysis. Physiotherapy 100(3):196–207
Silver JK (2015) Cancer prehabilitation and its role in improving health outcomes and reducing health care costs. Semin Oncol Nurs 31(1):13–30
Gonçalves CG, Groth AK (2019) Prehabilitation: how to prepare our patients for elective major abdominal surgeries? Rev Col Bras Cir 46(5):e20192267
Clegg A, Young J, Iliffe S et al (2013) Frailty in elderly people. Lancet 381(9868):752–762
Watt DG, McSorley ST, Horgan PG et al (2015) Enhanced recovery after surgery: which components, if any, impact on the systemic inflammatory response following colorectal surgery?: A systematic review. Medicine (Baltimore) 94(36):e1286
World Health Organization, Geneva: Switzerland (2001) Men ageing and health. Accessed 21 May 2021. https://apps.who.int/iris/bitstream/handle/10665/66941/WHO_NMH_NPH_01.2.pdf;jsessioni
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med 18(3):e1003583
Kalkum E, Klotz R, Seide S, Hüttner FJ, Kowalewski KF, Nickel F, Khajeh E, Knebel P, Diener MK, Probst P (2021) Systematic reviews in surgery—recommendations from the Study Center of the German Society of Surgery. Langenbecks Arch Surg 406(6):1723–1731
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H-Y, Corbett MS, Eldridge SM, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF (2019) Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O’Connell D, Oxman AD, Phillips B, Schünemann HJ, Edejer T, Varonen H, Vist GE, Williams JW Jr, Zaza S, GRADE Working Group (2004) Grading quality of evidence and strength of recommendations. BMJ 328(7454):1490
Ausania F, Senra P, Meléndez R et al (2019) Prehabilitation in patients undergoing pancreaticoduodenectomy: a randomized controlled trial. Rev Esp Enferm Dig 111(8):603–608
Barberan-Garcia A, Ubré M, Roca J et al (2018) Personalised prehabilitation in high-risk patients undergoing elective major abdominal surgery: a randomized blinded controlled trial. Ann Surg 267(1):50–56
Bousquet-Dion G, Awasthi R, Loiselle SÈ et al (2018) Evaluation of supervised multimodal prehabilitation programme in cancer patients undergoing colorectal resection: a randomized control trial. Acta Oncol 57(6):849–859
Carli F, Bousquet-Dion G, Awasthi R et al (2020) Effect of multimodal prehabilitation vs postoperative rehabilitation on 30-day postoperative complications for frail patients undergoing resection of colorectal cancer: a randomized clinical trial. JAMA Surg 155(3):233–242
Gillis C, Li C, Lee L et al (2014) Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology 121(5):937–947
López-Rodríguez-Arias F, Sánchez-Guillén L, Aranaz-Ostáriz V, Triguero-Cánovas D, Lario-Pérez S, Barber-Valles X, Lacueva FJ, Ramirez JM, Arroyo A (2021) Effect of home-based prehabilitation in an enhanced recovery after surgery program for patients undergoing colorectal cancer surgery during the COVID-19 pandemic. Support Care Cancer 29(12):7785–7791
Fulop A, Lakatos L, Susztak N, Szijarto A, Banky B (2021) The effect of trimodal prehabilitation on the physical and psychological health of patients undergoing colorectal surgery: a randomised clinical trial. Anaesthesia 76(1):82–90
Minnella EM, Awasthi R, Loiselle SE et al (2018) Effect of exercise and nutrition prehabilitation on functional capacity in esophagogastric cancer surgery: a randomized clinical trial. JAMA Surg 153(12):1081–1089
Minnella EM, Awasthi R, Bousquet-Dion G et al (2021) Multimodal prehabilitation to enhance functional capacity following radical cystectomy: a randomized controlled trial. Eur Urol Focus 7(1):132–138
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) Cochrane bias methods group; cochrane statistical methods group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Probst P, Zaschke S, Heger P, Harnoss JC, Hüttner FJ, Mihaljevic AL, Knebel P, Diener MK (2019) Evidence-based recommendations for blinding in surgical trials. Langenbecks Arch Surg 404(3):273–284. https://doi.org/10.1007/s00423-019-01761-6 (Epub 2019 Mar 1)
Milder DA, Pillinger NL, Kam PCA (2018) The role of prehabilitation in frail surgical patients: a systematic review. Acta Anaesthesiol Scand 62(10):1356–1366
Cabilan CJ, Hines S, Munday J (2016) The impact of prehabilitation on postoperative functional status, healthcare utilization, pain, and quality of life: a systematic review. Orthop Nurs 35(4):224–37
Gillis C, Buhler K, Bresee L et al (2018) Effects of nutritional prehabilitation, with and without exercise, on outcomes of patients who undergo colorectal surgery: a systematic review and meta-analysis. Gastroenterology 155(2):391-410.e4
Liu C, Lu Z, Zhu M, Lu X (2021 ) Trimodal prehabilitation for older surgical patients: a systematic review and meta-analysis. Aging Clin Exp Res.
Bruns ER, van den Heuvel B, Buskens CJ et al (2016) The effects of physical prehabilitation in elderly patients undergoing colorectal surgery: a systematic review. Colorectal Dis 18(8):O267–O277
Cabilan CJ, Hines S, Munday J (2015) The effectiveness of prehabilitation or preoperative exercise for surgical patients: a systematic review. JBI Database System Rev Implement Rep 13(1):146–187
Heger P, Probst P, Wiskemann J et al (2020) A systematic review and meta-analysis of physical exercise prehabilitation in major abdominal surgery (PROSPERO 2017 CRD42017080366). J Gastrointest Surg 24(6):1375–1385
Hughes MJ, Hackney RJ, Lamb PJ et al (2019) Prehabilitation before major abdominal surgery: a systematic review and meta-analysis. World J Surg 43(7):1661–1668
Luther A, Gabriel J, Watson RP et al (2018) The impact of total body prehabilitation on post-operative outcomes after major abdominal surgery: a systematic review. World J Surg 42(9):2781–2791
Bolshinsky V, Li MH, Ismail H et al (2018) Multimodal prehabilitation programs as a bundle of care in gastrointestinal cancer surgery: a systematic review. Dis Colon Rectum 61(1):124–138
Minnella EM, Bousquet-Dion G, Awasthi R et al (2017) Multimodal prehabilitation improves functional capacity before and after colorectal surgery for cancer: a five-year research experience. Acta Oncol 56(2):295–300
Waterland JL, McCourt O, Edbrooke L, Granger CL, Ismail H, Riedel B, Denehy L (2021) Efficacy of prehabilitation including exercise on postoperative outcomes following abdominal cancer surgery: a systematic review and meta-analysis. Front Surg 19(8):628848
Li C, Carli F, Lee L et al (2013) Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc 27(4):1072–1082
Tomás MT, Galán-Mercant A, Carnero EA et al (2018) Functional capacity and levels of physical activity in aging: a 3-year follow-up. Front Med (Lausanne) 9(4):244
Shinall MC Jr, Arya S, Youk A, Varley P, Shah R, Massarweh NN, Shireman PK, Johanning JM, Brown AJ, Christie NA, Crist L, Curtin CM, Drolet BC, Dhupar R, Griffin J, Ibinson JW, Johnson JT, Kinney S, LaGrange C, Langerman A, Loyd GE, Mady LJ, Mott MP, Patri M, Siebler JC, Stimson CJ, Thorell WE, Vincent SA, Hall DE (2020) Association of preoperative patient frailty and operative stress with postoperative mortality. JAMA Surg. 155(1):e194620
Sioutas G, Tsoulfas G (2020) Frailty assessment and postoperative outcomes among patients undergoing general surgery. Surgeon 18(6):e55–e66
Flexman AM, Street J, Charest-Morin R (2019) The impact of frailty and sarcopenia on patient outcomes after complex spine surgery. Curr Opin Anaesthesiol 32(5):609–615
Hijazi Y, Gondal U, Aziz O (2017) A systematic review of prehabilitation programs in abdominal cancer surgery. Int J Surg 39:156–162
Daniels SL, Lee MJ, George J et al (2020) Prehabilitation in elective abdominal cancer surgery in older patients: systematic review and meta-analysis. BJS Open 4(6):1022–1041
Author information
Authors and Affiliations
Contributions
NQP is the first author of this paper and was involved in the study design, acquisition of data, analysis and interpretation of data, writing up of the first draft of the paper and critical revision of manuscript. YXT is the second author of this paper and was involved in the study design, acquisition of data, analysis and interpretation of data and critical revision of manuscript. MS was involved in the study design, acquisition of data, analysis and interpretation of data and critical revision of manuscript. KKT, GKB and HY were involved in the study design, analysis and interpretation of data and critical revision of manuscript. WCAK is the senior author of this paper and was involved in the study design, analysis and interpretation of data and critical revision of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pang, N.Q., Tan, Y.X., Samuel, M. et al. Multimodal prehabilitation in older adults before major abdominal surgery: a systematic review and meta-analysis. Langenbecks Arch Surg 407, 2193–2204 (2022). https://doi.org/10.1007/s00423-022-02479-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02479-8