AbstractQuery
Background
Lymph node (LN) dissection along left recurrent laryngeal nerve (RLN) is challenging in esophagectomy for esophageal cancer, and double-lumen endotracheal tube (DLT) impedes the exposure of this area. The aim of this study was to determine whether bronchial blockers (BB) could be a better choice for this procedure.
Methods
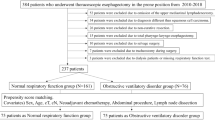
The clinical characteristics of patients who received McKeown esophagectomy with radical lymph node dissection in Wuhan Tongji Hospital between August 2017 and July 2019 were retrospectively analyzed. The 1:1 propensity score match analysis was performed to compare the short-term effectiveness, the numbers of lymph nodes dissected, and the patterns of recurrence and survival between the two groups.
Results
A total of 294 patients (192 and 102 in the DLT and BB group, respectively) were enrolled in the study. After matching, 204 patients (102 pairs) who underwent one-lung ventilation with DLT or BB displayed no significant variance in baseline characteristics. The BB group had higher number of LNs resected along left RLN (1.8 ± 2.3 vs. 2.5 ± 2.5, P = 0.001). For patients with metastatic left RLN LN, the BB group had longer medium survival time (15 vs. 32 months, P = 0.045), and tended to have longer medium recurrence-free survival time (6 vs. 15 months, P = 0.079), and lower rate of upper mediastinal and cervical LN recurrence (30.00% vs. 66.67%, P = 0.198). The postoperative complications were similar in both groups.
Conclusions
Compared with DLT, using BB in esophagectomy may allow more radical lymphadenectomy along left RLN.


Similar content being viewed by others
Availability of data and materials
This data and materials are available.
Abbreviations
- AP:
-
Artificial pneumothorax
- ASA:
-
American Association of Anesthesiologists
- BB:
-
Bronchial blockers
- BMI:
-
Body mass index
- CCI:
-
Charlson Comorbidity Index
- DLT:
-
Double-lumen tube
- LN:
-
Lymph node
- OS:
-
Overall survival
- RLN:
-
Recurrent laryngeal nerve
- VATS:
-
Video-assisted thoracoscopic surgery
References
Rizk NP, Ishwaran H, Rice TW, Chen L, Schipper PH, Kesler KA et al (2010) Optimum lymphadenectomy for esophageal cancer. Ann Surg 251(1):46–50
Visser E, Markar SR, Ruurda JP, Hanna GB, van Hillegersberg R (2019) Prognostic value of lymph node yield on overall survival in esophageal cancer patients. Ann Surg 269(2):261–268
Kitagawa Y, Uno T, Oyama T, Kato K, Kato H, Kawakubo H et al (2019) Esophageal cancer practice guidelines 2017 edited by the Japan Esophageal Society: part 2. Esophagus-Tokyo 16(1):25–43
Ajani JA, D Amico TA, Bentrem DJ, Chao J, Corvera C, Das P, Denlinger CS, Enzinger PC, Fanta P, Farjah F, Gerdes H, Gibson M, Glasgow RE, Hayman JA, Hochwald S, Hofstetter WL, Ilson DH, Jaroszewski D, Johung KL, Keswani RN, Kleinberg LR, Leong S, Ly QP, Matkowskyj KA, McNamara M, Mulcahy MF, Paluri RK, Park H, Perry KA, Pimiento J, Poultsides GA, Roses R, Strong VE, Wiesner G, Willett CG, Wright CD, McMillian NR, Pluchino LA (2019) Esophageal and esophagogastric junction cancers, version 2.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw 17:855–883
Baba M, Aikou T, Yoshinaka H, Natsugoe S, Fukumoto T, Shimazu H et al (1994) Long-term results of subtotal esophagectomy with three-field lymphadenectomy for carcinoma of the thoracic esophagus. Ann Surg 219(3):310–316
Ye K, Xu JH, Sun YF, Lin JA, Zheng ZG (2014) Characteristics and clinical significance of lymph node metastases near the recurrent laryngeal nerve from thoracic esophageal carcinoma. Genet Mol Res 13(3):6411–6419
Tan Z, Ma G, Zhao J, Bella AE, Rong T, Fu J et al (2014) Impact of thoracic recurrent laryngeal node dissection: 508 patients with tri-incisional esophagectomy. J Gastrointest Surg 18(1):187–193
Kato H, Tachimori Y, Watanabe H, Iizuka T, Terui S, Itabashi M et al (1991) Lymph node metastasis in thoracic esophageal carcinoma. J Surg Oncol 48(2):106–111
Fujita H, Kakegawa T, Yamana H, Shima I, Tanaka H, Ikeda S, Nogami S, Toh Y (1994) Lymph node metastasis and recurrence in patients with a carcinoma of the thoracic esophagus who underwent three-field dissection. World J Surg 18:266–272
Sharma S, Fujita H, Yamana H, Kakegawa T (1994) Patterns of lymph node metastasis in 3-field dissection for carcinoma in the thoracic esophagus. Surg Today 24(5):410–414
Chen J, Liu S, Pan J, Zheng X, Zhu K, Zhu J et al (2009) The pattern and prevalence of lymphatic spread in thoracic oesophageal squamous cell carcinoma. Eur J Cardio-Thorac 36(3):480–486
Liu Y, Zou Z, Xiao J, Zhang M, Yuan L, Zhao X (2019) A nomogram prediction model for recurrent laryngeal nerve lymph node metastasis in thoracic oesophageal squamous cell carcinoma. J Thorac Dis 11(7):2868–2877
Zhang S, Zhang P, Guo S, Lian J, Chen Y, Chen A et al (2020) Comparative study of three types of lymphadenectomy along the left recurrent laryngeal nerve by minimally invasive esophagectomy. Thorac Cancer 11(2):224–231
Xu J, Zheng B, Zhang S, Zeng T, Chen H, Zheng W et al (2019) The clinical significance of the intraoperative pathological examination of bilateral recurrent laryngeal nerve lymph nodes using frozen sections in cervical field lymph node dissection of thoracic esophageal squamous cell carcinoma. J Thorac Dis 11(8):3525–3533
Li C, Zhang F, Wang Y, Han C, Sun G, Liu Q et al (2013) Characteristics of recurrence after radical esophagectomy with two-field lymph node dissection for thoracic esophageal cancer. Oncol Lett 5(1):355–359
Kanemura T, Makino T, Miyazaki Y, Takahashi T, Kurokawa Y, Yamasaki M et al (2016) Distribution patterns of metastases in recurrent laryngeal nerve lymph nodes in patients with squamous cell esophageal cancer. Dis Esophagus 30(1):1–7
Taniyama Y, Miyata G, Kamei T, Nakano T, Abe S, Katsura K, Sakurai T, Teshima J, Hikage M, Ohuchi N (2014) Complications following recurrent laryngeal nerve lymph node dissection in oesophageal cancer surgery. Interact Cardiovasc Thorac Surg 20:41–46
Oshikiri T, Takiguchi G, Hasegawa H, Yamamoto M, Kanaji S, Yamashita K et al (2021) Postoperative recurrent laryngeal nerve palsy is associated with pneumonia in minimally invasive esophagectomy for esophageal cancer. Surg Endosc 35(2):837–844
Baba Y, Yoshida N, Shigaki H, Iwatsuki M, Miyamoto Y, Sakamoto Y et al (2016) Prognostic impact of postoperative complications in 502 patients with surgically resected esophageal squamous cell carcinoma. Ann Surg 264(2):305–311
Nakagawa A, Nakamura T, Oshikiri T, Hasegawa H, Yamamoto M, Kanaji S et al (2017) The surgical Apgar score predicts not only short-term complications but also long-term prognosis after esophagectomy. Ann Surg Oncol 24(13):3934–3946
Cuesta MA (2019) Review of different approaches of the left recurrent laryngeal nerve area for lymphadenectomy during minimally invasive esophagectomy. J Thorac Dis 11(S5):S766–S770
Noshiro H, Iwasaki H, Kobayashi K, Uchiyama A, Miyasaka Y, Masatsugu T et al (2010) Lymphadenectomy along the left recurrent laryngeal nerve by a minimally invasive esophagectomy in the prone position for thoracic esophageal cancer. Surg Endosc 24(12):2965–2973
Brodsky JB (2009) Lung separation and the difficult airway. Brit J Anaesth 103:i66-75
Ashok V, Francis J (2018) A practical approach to adult one-lung ventilation. BJA Education 18(3):69–74
Wang Y, Chang C, Wang Y, Huang C, Lin P, Cheng Y (2020) A survey of one-lung ventilation device in lung resection surgeries in Taiwan—a population-based nationwide cohort study. J Formos Med Assoc 119(1):449–454
Bussières JS, Somma J, Del Castillo JLC, Lemieux J, Conti M, Ugalde PA et al (2016) Bronchial blocker versus left double-lumen endotracheal tube in video-assisted thoracoscopic surgery: a randomized-controlled trial examining time and quality of lung deflation. Can J Anesth/Journal canadien d’anesthésie 63(7):818–827
Grocott HP (2018) Optimizing lung collapse with a bronchial blocker: it’s not what you use, but how you use it. J Cardiothor Vasc An 32(4):e93–e94
Bussières JS, Moreault O, Couture EJ, Provencher S (2019) Optimizing lung collapse with a bronchial blocker: it’s not what you use, but how you use it, part II. J Cardiothor Vasc An 33(1):255
Clayton-Smith A, Bennett K, Alston RP, Adams G, Brown G, Hawthorne T et al (2015) A comparison of the efficacy and adverse effects of double-lumen endobronchial tubes and bronchial blockers in thoracic surgery: a systematic review and meta-analysis of randomized controlled trials. J Cardiothor Vasc AN 29(4):955–966
Zhong T, Wang W, Chen J, Ran L, Story DA (2009) Sore throat or hoarse voice with bronchial blockers or double-lumen tubes for lung isolation: a randomised, prospective trial. Anaesth Intensive Care 37:441–446
Zheng M, Niu Z, Chen P, Feng D, Wang L, Nie Y, Wang B, Zhang Z, Shan S (2019) Effects of bronchial blockers on one-lung ventilation in general anesthesia. Medicine 98:e17387
Lu Y, Dai W, Zong Z, Xiao Y, Wu D, Liu X et al (2018) Bronchial blocker versus left double-lumen endotracheal tube for one-lung ventilation in right video-assisted thoracoscopic surgery. J Cardiothor Vasc An 32(1):297–301
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, pp 373–83
Tu D, Qu R, Wang Q, Fu X (2021) After-hours esophagectomy may pose additional risk to patients with esophageal cancer. J Thorac Dis 13(2):1118–1129
Cai L, Li Y, Sun L, Yang X, Wang W, Feng F et al (2017) Better perioperative outcomes in thoracoscopic-esophagectomy with two-lung ventilation in semi-prone position. J Thorac Dis 9(1):117–122
Nomura S, Tsujimoto H, Ishibashi Y, Fujishima S, Kouzu K, Harada M et al (2020) Efficacy of artificial pneumothorax under two-lung ventilation in video-assisted thoracoscopic surgery for esophageal cancer. Surg Endosc 34(12):5501–5507
Biere SSAY, van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C, Garcia JR et al (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial, pp 1887–92
Lin M, Shen Y, Wang H, Fang Y, Qian C, Xu S et al (2018) A comparison between two lung ventilation with CO2 artificial pneumothorax and one lung ventilation during thoracic phase of minimally invasive esophagectomy. J Thorac Dis. 2018–01–01;10(3):1912–8
Neustein SM (2015) Pro: bronchial blockers should be used routinely for providing one-lung ventilation. J Cardiothor Vasc An 29(1):234–236
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by all authors. Material analysis was performed by DHT. DHT wrote the manuscript. RQ, WP, GY, XF, and YC participated in revising the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the institutional review board of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology. All patients signed informed consent.
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Conflict of interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tu, DH., Qu, R., Ping, W. et al. Double-lumen tube versus bronchial blocker in lymphadenectomy along the left recurrent laryngeal nerve for esophageal cancer: a propensity-matched analysis. Langenbecks Arch Surg 407, 1891–1900 (2022). https://doi.org/10.1007/s00423-022-02475-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02475-y