Abstract
Purpose
Recent shift to radical extralevator abdominoperineal excision (ELAPE) approach has seen an increased incidence of post-operative perineal hernia. However, there is no standardised surgical approach for its repair. The aim of this study was to report intra and post-operative results of the perineal hernia repair by the novel trans-abdominal PERineal Laparoscopic Sling (PERLS) Technique in patients who developed post-operative perineal hernia following ELAPE.
Methods
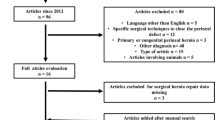
This is a retrospective analysis of consecutive patients who underwent perineal hernia repair by laparoscopic PERLS approach. All patients had undergone ELAPE with vertical rectus abdominis muscle (VRAM) flap reconstruction during the index surgery for treatment of rectal cancer. Post-operative complications, operative time, conversion rate to open surgery and incidence of recurrent perineal hernia were noted.
Results
Seven patients were operated for perineal hernia. The mean operative time was 105 min (range: 87 to 131 min). One case needed conversion to the open approach. The incidence of early complications was 57.1% including just single Clavien-Dindo I and two Clavien-Dindo II complications, while recurrence rate was 14.3%.
Conclusion
PERLS perineal hernia repair is safe, performed in convenient time duration (mean = 105 min) and has reasonably less recurrence rate.


Similar content being viewed by others
References
Yu HC, Peng H, He XS, Zhao RS (2014) Comparison of short- and long-term outcomes after extralevator abdominoperineal excision and standard abdominoperineal excision for rectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis 29(2):183–191 (Epub 2013 Nov 23)
Zhang Y, Wang D, Zhu L, et al. Standard versus extralevator abdominoperineal excision and oncologic outcomes for patients with distal rectal cancer: a meta-analysis. Medicine (Baltimore). 2017;96(52):e9150.
Sayers AE, Patel RK, Hunter IA. Perineal hernia formation following extraelevator abdominoperineal excision. Colorectal Dis(2015). 17(4):351–355.
Stamatiou D, Skandalakis JE, Skandalakis LJ, Mirilas P (2010) Perineal hernia: surgical anatomy, embryology, and technique of repair. Am Surg 76(5):474–479
Balla A, Batista Rodríguez G, Buonomo N et al (2017) Perineal hernia repair after abdominoperineal excision or extralevator abdominoperineal excision: a systematic review of the literature. Tech Coloproctol - 21:329–336. https://doi.org/10.1007/s10151-017-1634-8
Tollens T, Topal H, Vermeiren K, Aelvoet C (2014) Prospective analysis of laparoscopic ventral hernia repair using the Ventralight™ ST hernia patch with or without the ECHO PS™ positioning system. Surg Technol Int 24:149–154
England N. NHS England. Patient initiated follow up: giving patients greater control over their hospital follow-up care [Internet]. England.nhs.uk. (2021) [Accessed: 1 December 2021]. Available from: https://www.england.nhs.uk/outpatient-transformation-programme/patient-initiated-follow-up-giving-patients-greater-control-over-their-hospital-follow-up-care/
Katayama H, Kurokawa Y, Nakamura K et al (2016) Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today 46:668–685. https://doi.org/10.1007/s00595-015-1236-x
Narang SK, Alam NN, Köckerling F, Daniels IR, Smart NJ (2016) Repair of perineal hernia following abdominoperineal excision with biological mesh: a systematic review. Front Surg 5(3):49. https://doi.org/10.3389/fsurg.2016.00049.PMID:27656644;PMCID:PMC5011127
Yang X, Jin C, Deng X, Wang M, Zhang Y, Wei M, Meng W, Wang Z (2016) Laparoscopic extralevator abdominoperineal excision of the rectum with primary suturing: short-term outcomes from single-institution study. J Laparoendosc Adv Surg Tech A 26(1):40–46. https://doi.org/10.1089/lap.2015.0325
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, Choi HS, Kim DW, Chang HJ, Kim DY, Jung KH, Kim TY, Kang GH, Chie EK, Kim SY, Sohn DK, Kim DH, Kim JS, Lee HS, Kim JH, Oh JH. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol. 2014 Jun;15(7):767–74. doi: https://doi.org/10.1016/S1470-2045(14)70205-0. Epub 2014 May 15. Erratum in: Lancet Oncol. 2016 Jul;17 (7):e270. PMID: 24837215.
Baird DLH, Simillis C, Kontovounisios C, Sheng Q, Nikolaou S, Law WL, Rasheed S, Tekkis PP. A systematic review of transabdominal levator division during abdominoperineal excision of the rectum (APER). Tech Coloproctol. 2017 Sep;21(9):701–707. doi: https://doi.org/10.1007/s10151-017-1682-0. Epub 2017 Sep 11. PMID: 28891039.
Barker T, Branagan G, Wright E, Crick A, McGuiness C, Chave H (2013) Vertical rectus abdominis myocutaneous flap reconstruction of the perineal defect after abdominoperineal excision is associated with low morbidity. Colorectal Dis 15(9):1177–1183. https://doi.org/10.1111/codi.12286 (PMID: 23672636)
Teramura K, Watanabe Y, Takeuchi S, Nakamura F, Hirano S (2018) Laparoscopic repair with cone-shaped mesh implantation for perineal hernia occurred after laparoscopic abdominoperineal resection. Int J Surg Case Rep 49:115–117. https://doi.org/10.1016/j.ijscr.2018.06.032
Goedhart-de Haan AM, Langenhoff BS, Petersen D, Verheijen PM (2016) Laparoscopic repair of perineal hernia after abdominoperineal excision. Hernia 20(5):741–746
Casasanta M, Moore LJ (2012) Laparoscopic repair of a perineal hernia. Hernia 16:363–367. https://doi.org/10.1007/s10029-010-0756-y
Author information
Authors and Affiliations
Contributions
Both authors have equally contributed for the paper with substantial contributions to the conception and design of the study, the acquisition, analysis and interpretation of data for the work. Both have finally approved the version to be published.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Samar, A.M., Branagan, G. Perineal hernia repair after extralevator abdominoperineal excision, how we do it (PERineal Laparoscopic Sling: PERLS Technique). Langenbecks Arch Surg 407, 2187–2191 (2022). https://doi.org/10.1007/s00423-022-02457-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02457-0