Abstract
Purpose
Transversus abdominis plane (TAP) block is a new option for reducing postoperative pain. This study investigated the effects of laparoscopic TAP block on postoperative adverse events and analgesia and antiemetics requirements after bariatric surgery.
Methods
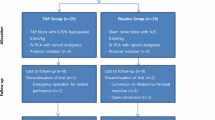
In this randomized clinical trial study, patients were randomly divided into control (N = 20) or TAP block (N = 20) groups. In the TAP block group, the block was performed under direct laparoscopic guidance after surgery and before the removal of trocars.
Results
Fifteen patients (75%) versus four patients (20%) received opioids within the first 6 h in the control and TAP groups, respectively (p-value < 0.001). The cumulative amount of opioids consumed in the 24 and 48 h after surgery was lower in the TAP group (p-value < 0.001). The visual analog scale (VAS) regarding general and wound-specific pain was significantly lower in the TAP group compared to the control group at 6 and 24 h both at rest and in movement. However, there was no significant difference at 48 h postoperatively. The percentages of patients having postoperative nausea and vomiting (PONV), pruritus, and resumption of bowel movement were not significantly different between the two groups at any time (6, 24, and 48 h) postoperatively.
Conclusion
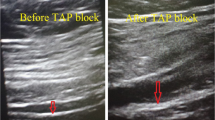
Laparoscopic-guided TAP block is a pragmatic, applicable, and minimally invasive regional technique and can be part of effective postoperative pain management in morbidly obese patients undergoing bariatric surgery. Applying it laparoscopically without the need for ultrasound is also useful and effective.
Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Eldar S, Heneghan HM, Brethauer SA, Schauer PR (2011) Bariatric surgery for treatment of obesity. Int J Obes 35:S16–S21. https://doi.org/10.1038/ijo.2011.142
Idra S, Modesti C, Punzo G, et al (2008) Postoperative analgesia in laparoscopic bariatric surgery: 14AP6–10. Eur J Anaesthesiol | EJA 25:
Nguyen NT, Lee SL, Goldman C et al (2001) Comparison of pulmonary function and postoperative pain after laparoscopic versus open gastric bypass: a randomized trial. J Am Coll Surg 192:467–469. https://doi.org/10.1016/s1072-7515(01)00822-5
Lopez PP, Stefan B, Schulman CI, Byers PM (2008) Prevalence of sleep apnea in morbidly obese patients who presented for weight loss surgery evaluation: more evidence for routine screening for obstructive sleep apnea before weight loss surgery. Am Surg 74:834–838
Sarandan M, Guragata-Balasa C, Papurica M et al (2011) Anesthesia in laparoscopic bariatric surgery (gastric sleeve) - preliminary experience. Timisoara Med J 61:26–31
Ramsay MA (2000) Acute postoperative pain management Proc (Bayl Univ Med Cent) 13:244–247. https://doi.org/10.1080/08998280.2000.11927683
de Beer J, de V, Winemaker MJ, Donnelly GAE, et al (2005) Efficacy and safety of controlled-release oxycodone and standard therapies for postoperative pain after knee or hip replacement. Can J Surg 48:277–283
Garimella V, Cellini C (2013) Postoperative pain control. Clin Colon Rectal Surg 26:191–196. https://doi.org/10.1055/s-0033-1351138
Macintyre PE, Loadsman JA, Scott DA (2011) Opioids, ventilation and acute pain management. Anaesth Intensive Care 39:545–558. https://doi.org/10.1177/0310057X1103900405
Schwartz AR, Patil SP, Squier S et al (2010) Obesity and upper airway control during sleep. J Appl Physiol 108:430–435. https://doi.org/10.1152/japplphysiol.00919.2009
Mafort TT, Rufino R, Costa CH, Lopes AJ (2016) Obesity: systemic and pulmonary complications, biochemical abnormalities, and impairment of lung function. Multidiscip Respir Med 11:28. https://doi.org/10.1186/s40248-016-0066-z
Nielsen KC, Guller U, Steele SM et al (2005) Influence of obesity on surgical regional anesthesia in the ambulatory setting: an analysis of 9,038 blocks. Anesthesiology 102:181–187. https://doi.org/10.1097/00000542-200501000-00027
Magoon R, Choudhury A (2019) Opioid free anesthesia: is it too early to bid adieu? Can J Anaesth 66(10):1268–1269
1007/s12630–019–01446–0
Miller AD, Smith KM (2006) Medication and nutrient administration considerations after bariatric surgery. Am J Heal Pharm AJHP Off J Am Soc Heal Pharm 63:1852–1857. https://doi.org/10.2146/ajhp060033
Rafi AN (2001) Abdominal field block: a new approach via the lumbar triangle. Anaesthesia 56:1024–1026
Hebbard P, Fujiwara Y, Shibata Y, Royse C (2007) Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care 35:616–617
Tran TMN, Ivanusic JJ, Hebbard P, Barrington MJ (2009) Determination of spread of injectate after ultrasound-guided transversus abdominis plane block: a cadaveric study. Br J Anaesth 102:123–127. https://doi.org/10.1093/bja/aen344
O’Donnell BD (2006) The transversus abdominis plane (TAP) block in open retropubic prostatectomy. Reg Anesth Pain Med 31:91
Gluck O, Barber E, Feldstein O et al (2021) The effect of subcutaneous and intraperitoneal anesthesia on post laparoscopic pain: a randomized controlled trial. Sci Rep 11:81. https://doi.org/10.1038/s41598-020-80130-6
Bisgaard T (2006) Analgesic treatment after laparoscopic cholecystectomy: a critical assessment of the evidence. Anesthesiology 104:835–846. https://doi.org/10.1097/00000542-200604000-00030
Mittal T, Dey A, Siddhartha R et al (2018) Efficacy of ultrasound-guided transversus abdominis plane (TAP) block for postoperative analgesia in laparoscopic gastric sleeve resection: a randomized single blinded case control study. Surg Endosc 32:4985–4989. https://doi.org/10.1007/s00464-018-6261-6
Carney J, McDonnell JG, Ochana A et al (2008) The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg 107:2056–2060. https://doi.org/10.1213/ane.0b013e3181871313
Stuhldreher JM, Adamina M, Konopacka A et al (2012) Effect of local anesthetics on postoperative pain and opioid consumption in laparoscopic colorectal surgery. Surg Endosc 26:1617–1623. https://doi.org/10.1007/s00464-011-2079-1
Abrishami A, Chan J, Chung F, Wong J (2011) Preoperative pain sensitivity and its correlation with postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology 114:445–457. https://doi.org/10.1097/ALN.0b013e3181f85ed2
Jakobsson J, Wickerts L, Forsberg S, Ledin G (2015) Transversus abdominal plane (TAP) block for postoperative pain management: a review. F1000Research 4:. https://doi.org/10.12688/f1000research.7015.1
El-Dawlatly AA, Turkistani A, Kettner SC et al (2009) Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth 102:763–767. https://doi.org/10.1093/bja/aep067
Yu N, Long X, Lujan-Hernandez JR et al (2014) Transversus abdominis-plane block versus local anesthetic wound infiltration in lower abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol 14:121. https://doi.org/10.1186/1471-2253-14-121
Johns N, O’Neill S, Ventham NT et al (2012) Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: a systematic review and meta-analysis. Color Dis Off J Assoc Coloproctology Gt Britain Irel 14:e635–e642. https://doi.org/10.1111/j.1463-1318.2012.03104.x
Keller DS, Ermlich BO, Delaney CP (2014) Demonstrating the benefits of transversus abdominis plane blocks on patient outcomes in laparoscopic colorectal surgery: review of 200 consecutive cases. J Am Coll Surg 219:1143–1148. https://doi.org/10.1016/j.jamcollsurg.2014.08.011
Ruiz-Tovar J, Garcia A, Ferrigni C et al (2018) Laparoscopic-guided transversus abdominis plane (TAP) block as part of multimodal analgesia in laparoscopic Roux-en-Y gastric bypass within an enhanced recovery after surgery (ERAS) program: a prospective randomized clinical trial. Obes Surg 28:3374–3379. https://doi.org/10.1007/s11695-018-3376-8
Aissou M, Ghalayini M, Yazid L et al (2011) Ultrasound control of local anaesthetic location after TAP block performed using landmark-based technique: a cohort study. Ann Fr Anesth Reanim 30:641–644. https://doi.org/10.1016/j.annfar.2011.03.020
Kadam RV, Field JB (2011) Ultrasound-guided continuous transverse abdominis plane block for abdominal surgery. J Anaesthesiol Clin Pharmacol 27:333–336. https://doi.org/10.4103/0970-9185.83676
McDermott G, Korba E, Mata U et al (2012) Should we stop doing blind transversus abdominis plane blocks? Br J Anaesth 108:499–502. https://doi.org/10.1093/bja/aer422
Sinha A, Jayaraman L, Punhani D (2013) Efficacy of ultrasound-guided transversus abdominis plane block after laparoscopic bariatric surgery: a double blind, randomized, controlled study. Obes Surg 23:548–553. https://doi.org/10.1007/s11695-012-0819-5
Wassef M, Lee DY, Levine JL et al (2013) Feasibility and analgesic efficacy of the transversus abdominis plane block after single-port laparoscopy in patients having bariatric surgery. J Pain Res 6:837–841. https://doi.org/10.2147/JPR.S50561
Sherif A, Koptan H, Soliman S Feasibility and perioperative pain-relieving efficacy of ultrasound-guided transversus abdominis plane block in morbidly obese patients undergoing laparoscopic bariatric surgery YR - 2015/4/1. Res Opin Anesth Intensive Care 50 OP-56 VO–2. https://doi.org/10.4103/2356-9115.161334
Owen DJ, Harrod I, Ford J et al (2011) The surgical transversus abdominis plane block–a novel approach for performing an established technique. BJOG 118:24–27. https://doi.org/10.1111/j.1471-0528.2010.02779.x
Hamid HKS, Ahmed AY, Saber AA et al (2020) Transversus abdominis plane block using a short-acting local anesthetic reduces pain and opioid consumption after laparoscopic bariatric surgery: a meta-analysis. Surg Obes Relat Dis 16:1349–1357. https://doi.org/10.1016/j.soard.2020.04.023
Grape S, Kirkham KR, Albrecht E (2020) The analgesic efficacy of transversus abdominis plane block after bariatric surgery: a systematic review and meta-analysis with trial sequential analysis. Obes Surg 30:4061–4070. https://doi.org/10.1007/s11695-020-04768-x
Aamir MA, Sahebally SM, Heneghan H (2021) Transversus abdominis plane block in laparoscopic bariatric surgery—a systematic review and meta-analysis of randomized controlled trials. Obes Surg 31:133–142. https://doi.org/10.1007/s11695-020-04898-2
Favuzza J, Delaney CP (2013) Outcomes of discharge after elective laparoscopic colorectal surgery with transversus abdominis plane blocks and enhanced recovery pathway. J Am Coll Surg 217:503–506. https://doi.org/10.1016/j.jamcollsurg.2013.03.030
Kishore K, Agarwal A (2011) Ultrasound-guided continuous transverse abdominis plane block for abdominal surgery. J Anaesthesiol Clin Pharmacol 27:336–338. https://doi.org/10.4103/0970-9185.83677
Author information
Authors and Affiliations
Contributions
Sayed Mehdi Jalali: conceptualization, methodology, and project administration; Mohammad Hadi Bahri: formal analysis, data curation, investigation, and writing—original draft; Seyed mostafa meshkati yazd: methodology, critical revision, and data analysis; Mohamadreza Karoobi: data gathering, writing—review and editing, and final approval of the version to be published; Niloufar Shababi: methodology, critical revision, and data analysis.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Ethics Committee of the Tehran University of Medical Sciences. Permission to carry out the study and access patient records was sought from the respective university administrators. Code: IR.TUMS.IKHC.REC.1396.3867.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• The amount of opioids administered after surgery was lower in the TAP group.
• VAS scores were significantly lower in the TAP group at 6 and 24 h after surgery.
• TAP block can be beneficial for postoperative pain management in bariatric surgeries.
Rights and permissions
About this article
Cite this article
Jalali, S.M., Bahri, M.H., Yazd, S.M.M. et al. Efficacy of laparoscopic transversus abdominis plane block on postoperative pain management and surgery side effects in laparoscopic bariatric surgeries. Langenbecks Arch Surg 407, 549–557 (2022). https://doi.org/10.1007/s00423-021-02400-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02400-9