Abstract
Purpose
The efficacy of pre or postoperative chemotherapy for resectable colorectal cancer liver metastases (CRLM) is disputed. This study aimed to examine the risk factors for time to surgical failure (TSF) and analyze the efficacy of pre or postoperative chemotherapy prior to liver resection for CRLM.
Methods
The clinicopathological factors of 567 patients who underwent initial hepatectomy for CRLM at 7 university hospitals between April 2007 and March 2013 were retrospectively analyzed. The prognostic factors were identified and then stratified into two groups according to the number of preoperative prognostic factors: the high-score group (H-group, score 2–4) and the low-score group (L-group, score 0 or 1).
Results
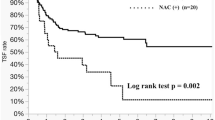
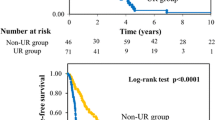
Patients who experienced unresectable recurrence within 12 months after initial treatment had a significantly shorter prognosis than other patients (p < 0.001). Multivariate analysis identified age ≥ 70 (p = 0.001), pT4 (p = 0.015), pN1 (p < 0.001), carbohydrate antigen 19–9 ≥ 37 U/ml (p = 0.002), Clavien-Dindo grade ≥ IIIa (p = 0.013), and postoperative chemotherapy (p = 0.006) as independent prognostic factors. In the H-group, patients who received chemotherapy had a better prognosis than those who did not (p = 0.001).
Conclusion
Postoperative chemotherapy is beneficial in colorectal cancer patients with more than two of the following factors: age ≥ 70, carbohydrate antigen 19–9–positivity, pT4, and lymph node metastasis.




Similar content being viewed by others
Data availability
Reasonable requests for access to the data may be directed to the corresponding author.
Code availability
Not applicable.
References
Hackl C, Neumann P, Gerken M, Loss M, Klinkhammer-Schalke M, Schlitt HJ (2014) Treatment of colorectal liver metastases in Germany: a ten-year population-based analysis of 5772 cases of primary colorectal adenocarcinoma. BMC Cancer 14:810
Manfredi S, Lepage C, Hatem C, Coatmeur O, Faivre J, Bouvier AM (2006) Epidemiology and management of liver metastases from colorectal cancer. Ann Surg 244(2):254–259
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230(3):309–18 (discussion 18 21)
Tournigand C, Andre T, Achille E, Lledo G, Flesh M, Mery-Mignard D et al (2004) FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol 22(2):229–237
Kodeda K, Nathanaelsson L, Jung B, Olsson H, Jestin P, Sjovall A et al (2013) Population-based data from the Swedish Colon Cancer Registry. Br J Surg 100(8):1100–1107
van der Pool AE, Damhuis RA, Ijzermans JN, de Wilt JH, Eggermont AM, Kranse R et al (2012) Trends in incidence, treatment and survival of patients with stage IV colorectal cancer: a population-based series. Colorectal Dis 14(1):56–61
Fong Y, Cohen AM, Fortner JG, Enker WE, Turnbull AD, Coit DG et al (1997) Liver resection for colorectal metastases. J Clin Oncol 15(3):938–946
Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P et al (1996) Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer 77(7):1254–62
Minagawa M, Yamamoto J, Kosuge T, Matsuyama Y, Miyagawa S, Makuuchi M (2007) Simplified staging system for predicting the prognosis of patients with resectable liver metastasis: development and validation. Arch Surg 142(3):269–76 (discussion 77)
Schrodter S, Hakenberg OW, Manseck A, Leike S, Wirth MP (2002) Outcome of surgical treatment of isolated local recurrence after radical nephrectomy for renal cell carcinoma. J Urol 167(4):1630–1633
de Jong MC, Pulitano C, Ribero D, Strub J, Mentha G, Schulick RD et al (2009) Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg 250(3):440–448
Mise Y, Imamura H, Hashimoto T, Seyama Y, Aoki T, Hasegawa K et al (2010) Cohort study of the survival benefit of resection for recurrent hepatic and/or pulmonary metastases after primary hepatectomy for colorectal metastases. Ann Surg 251(5):902–909
Park JS, Kim HK, Choi YS, Kim K, Shim YM, Jo J et al (2010) Outcomes after repeated resection for recurrent pulmonary metastases from colorectal cancer. Ann Oncol 21(6):1285–1289
Wicherts DA, de Haas RJ, Salloum C, Andreani P, Pascal G, Sotirov D et al (2013) Repeat hepatectomy for recurrent colorectal metastases. Br J Surg 100(6):808–818
Oba M, Hasegawa K, Matsuyama Y, Shindoh J, Mise Y, Aoki T et al (2014) Discrepancy between recurrence-free survival and overall survival in patients with resectable colorectal liver metastases: a potential surrogate endpoint for time to surgical failure. Ann Surg Oncol 21(6):1817–1824
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L et al (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149(5):680–688
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R et al (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149(5):713–724
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology. 2012;ver 2.
Van Cutsem E, Nordlinger B, Cervantes A, Group EGW (2010) Advanced colorectal cancer: ESMO Clinical Practice Guidelines for treatment. Ann Oncol 21(Suppl 5):v93–v97
Chen Q, Wu C, Zhao H, Wu J, Zhao J, Bi X et al (2020) Neo-adjuvant chemotherapy-induced neutropenia is associated with histological responses and outcomes after the resection of colorectal liver metastases. J Gastrointest Surg 24(3):659–670
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P et al (2013) Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol 14(12):1208–1215
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P et al (2008) Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet 371(9617):1007–1016
Kanemitsu Y, Kato T, Shimizu Y, Inaba Y, Shimada Y, Nakamura K et al (2009) A randomized phase II/III trial comparing hepatectomy followed by mFOLFOX6 with hepatectomy alone as treatment for liver metastasis from colorectal cancer: Japan Clinical Oncology Group Study JCOG0603. Jpn J Clin Oncol 39(6):406–409
Jang JY, Han Y, Lee H, Kim SW, Kwon W, Lee KH et al (2018) Oncological benefits of neoadjuvant chemoradiation with gemcitabine versus upfront surgery in patients with borderline resectable pancreatic cancer: a prospective, randomized, open-label, multicenter phase 2/3 trial. Ann Surg 268(2):215–222
Kuerer HM, Rauch GM, Krishnamurthy S, Adrada BE, Caudle AS, DeSnyder SM et al (2018) A clinical feasibility trial for identification of exceptional responders in whom breast cancer surgery can be eliminated following neoadjuvant systemic therapy. Ann Surg 267(5):946–951
Iwatsuki S, Dvorchik I, Madariaga JR, Marsh JW, Dodson F, Bonham AC et al (1999) Hepatic resection for metastatic colorectal adenocarcinoma: a proposal of a prognostic scoring system. J Am Coll Surg 189(3):291–299
Kato T, Yasui K, Hirai T, Kanemitsu Y, Mori T, Sugihara K et al (2003) Therapeutic results for hepatic metastasis of colorectal cancer with special reference to effectiveness of hepatectomy: analysis of prognostic factors for 763 cases recorded at 18 institutions. Dis Colon Rectum 46(10 Suppl):S22-31
Nagashima I, Takada T, Matsuda K, Adachi M, Nagawa H, Muto T et al (2004) A new scoring system to classify patients with colorectal liver metastases: proposal of criteria to select candidates for hepatic resection. J Hepatobiliary Pancreat Surg 11(2):79–83
Liu JM, Wang YY, Liu W, Xu D, Wang K, Xing BC (2021) Preoperative CA19–9: a competitive predictor of recurrence in patients with colorectal cancer liver metastases after hepatectomy. Int J Colorectal Dis 36(4):767–778
Sakamoto Y, Miyamoto Y, Beppu T, Nitta H, Imai K, Hayashi H et al (2015) Post-chemotherapeutic CEA and CA19-9 are prognostic factors in patients with colorectal liver metastases treated with hepatic resection after oxaliplatin-based chemotherapy. Anticancer Res 35(4):2359–2368
Sawada Y, Sahara K, Endo I, Sakamoto K, Honda G, Beppu T et al (2020) Long-term outcome of liver resection for colorectal metastases in the presence of extrahepatic disease: a multi-institutional Japanese study. J Hepatobiliary Pancreat Sci 27(11):810–818
Zorzi D, Laurent A, Pawlik TM, Lauwers GY, Vauthey JN, Abdalla EK (2007) Chemotherapy-associated hepatotoxicity and surgery for colorectal liver metastases. Br J Surg 94(3):274–286
Nakano H, Oussoultzoglou E, Rosso E, Casnedi S, Chenard-Neu MP, Dufour P et al (2008) Sinusoidal injury increases morbidity after major hepatectomy in patients with colorectal liver metastases receiving preoperative chemotherapy. Ann Surg 247(1):118–124
Hirokawa F, Asakuma M, Komeda K, Shimizu T, Inoue Y, Kagota S et al (2019) Is neoadjuvant chemotherapy appropriate for patients with resectable liver metastases from colorectal cancer? Surg Today 49(1):82–89
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study and the associated protocol received approval from the Ethics Committee of each institution (approval number: 2734, Osaka Medical College). We have obtained consent to participate.
Consent to publication
We have obtained consent to publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hirokawa, F., Ueno, M., Nakai, T. et al. Treatment strategy for resectable colorectal cancer liver metastases from the viewpoint of time to surgical failure. Langenbecks Arch Surg 407, 699–706 (2022). https://doi.org/10.1007/s00423-021-02372-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02372-w