Abstract
Purpose
Intraoperative fluid restriction is reported to be associated with reduced postoperative tissue edema and decreased incidence of postoperative pancreatic fistula (POPF) in pancreatic surgery. However, there is limited information regarding the postoperative approach to prevent postoperative tissue edema and reduce POPF.
Methods
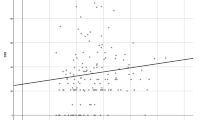
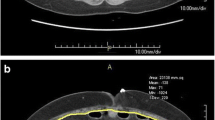
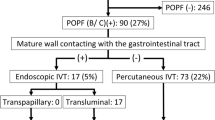
Patients undergoing distal pancreatectomy from 2013 to 2018 in our institute were retrospectively enrolled (n = 128). The patients were classified into the two groups: an early diuresis group (ED group: patients administered diuretic agents on postoperative day 2 or earlier between 2016 and 2018, n = 69) and a conventional diuresis group (CD group: patients administered diuretic agents on postoperative day 3 or later between 2013 and 2015, n = 59). Postoperative tissue edema assessed by CT imaging and the incidence of clinically relevant POPF (CR-PF; grade B or C) were compared.
Results
Postoperative tissue edema was significantly reduced in the ED group (p < 0.0001). The incidence of CR-PF was lower in the ED group (19% vs. 32%, p = 0.082), especially in patients with postoperative diuresis on POD 1 (12%, p = 0.044).
Conclusion
Early and aggressive postoperative diuresis potentially reduced postoperative visceral tissue edema. This postoperative approach to prevent tissue edema may reduce the incidence of CR-PF in pancreatic surgery.

Similar content being viewed by others
Data availability
The data and material presented in our study is available from the corresponding author.
Code availability
Not applicable.
References
Fagniez PL, Kracht M, Rotman N (1988) Limited conservative pancreatectomy for benign tumours: a new technical approach. Br J Surg 75(7):719. https://doi.org/10.1002/bjs.1800750733
Shin CH, Long DR, McLean D et al (2018) Effects of intraoperative fluid management on postoperative outcomes: a hospital registry study. Ann Surg 267(6):1084–1092. https://doi.org/10.1097/sla.0000000000002220
Myles PS, Bellomo R, Corcoran T et al (2018) Restrictive versus liberal fluid therapy for major abdominal surgery. N Engl J Med 378(24):2263–2274. https://doi.org/10.1056/nejmoa1801601
Fischer M, Matsuo K, Gonen M et al (2010) Relationship between intraoperative fluid administration and perioperative outcome after pancreaticoduodenectomy: results of a prospective randomized trial of acute normovolemic hemodilution compared with standard intraoperative management. Ann Surg 252(6):952–958. https://doi.org/10.1097/sla.0b013e3181ff36b1
Bruns H, Kortendieck V, Raab HR et al (2016) Intraoperative fluid excess is a risk factor for pancreatic fistula after partial pancreaticoduodenectomy. HPB Surg 2016:1601340. https://doi.org/10.1155/2016/1601340
Shimizu A, Kawai M, Hirono S et al (2018) Postoperative visceral tissue edema assessed by computed tomography is a predictor for severe complications after pancreaticoduodenectomy. J Gastrointest Surg 22(1):77–87. https://doi.org/10.1007/s11605-017-3608-6
Han IW, Kim H, Heo J et al (2017) Excess intraoperative fluid volume administration is associated with pancreatic fistula after pancreaticoduodenectomy: a retrospective multicenter study. Medicine (Baltimore) 96(22):e6893. https://doi.org/10.1097/md.0000000000006893
Japan Pancreas Society (1996) Classification of pancreatic carcinoma (Fourth English edition). Kanehara, Tokyo
Akita H, Takahashi H, Gotoh K et al (2015) Closure method for thick pancreas stump after distal pancreatectomy: soft coagulation and polyglycolic acid felt with fibrin glue. Langenbecks Arch Surg 400(7):843–848. https://doi.org/10.1007/s00423-015-1339-2
Lo Gullo R, Mishra S, Lira DA et al (2015) Quantification of interstitial fluid on whole body CT: comparison with whole body autopsy. Forensic Sci Med Pathol 11(4):488–496. https://doi.org/10.1007/s12024-015-9728-y
Massalou D, Baqué-Juston M, Foti P et al (2013) CT quantification of hemoperitoneum volume in abdominal haemorrhage: a new method. Surg Radiol Anat 35(6):481–486. https://doi.org/10.1007/s00276-012-1057-1
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. https://doi.org/10.1097/sla.0b013e3181b13ca2
Bassi C, Marchegiani G, Dervenis C et al (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery 161(3):584–591. https://doi.org/10.1016/j.surg.2016.11.014
Simões CM, Carmona MJC, Hajjar LA et al (2018) Predictors of major complications after elective abdominal surgery in cancer patients. BMC Anesthesiol 18(1):49. https://doi.org/10.1186/s12871-018-0516-6
Brandstrup B, Tønnesen H, Beier-Holgersen R et al (2003) Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg 238(5):641–648. https://doi.org/10.1097/01.sla.0000094387.50865.23
Kulemann B, Timme S, Seifert G et al (2013) Intraoperative crystalloid overload leads to substantial inflammatory infiltration of intestinal anastomoses-a histomorphological analysis. Surgery 154(3):596–603. https://doi.org/10.1016/j.surg.2013.04.010
Akerberg D, Ansari D, Bergenfeldt M et al (2019) Early postoperative fluid retention is a strong predictor for complications after pancreatoduodenectomy. HPB (Oxford) 21(12):1784–1789. https://doi.org/10.1016/j.hpb.2019.05.003
Danelich IM, Bergquist JR, Bergquist WJ et al (2018) Early diuresis after colon and rectal surgery does not reduce length of hospital stay: results of a randomized trial. Dis Colon Rectum 61(10):1187–1195. https://doi.org/10.1097/DCR.0000000000001183
Peng YP, Zhu XL, Yin LD et al (2017) Risk factors of postoperative pancreatic fistula in patients after distal pancreatectomy: a systematic review and meta-analysis. Sci Rep 7(1):185. https://doi.org/10.1038/s41598-017-00311-8
Goh BK, Tan YM, Chung YF et al (2008) Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch Surg 143(10):956–965. https://doi.org/10.1001/archsurg.143.10.956
Mech K, Wysocki L, Guzel T et al (2018) a review of methods for preventing pancreatic fistula after distal pancreatectomy. Pol Przegl Chir 90(2):38–44. https://doi.org/10.5604/01.3001.0011.7491
Winer LK, Dhar VK, Wima K et al (2018) Perioperative net fluid balance predicts pancreatic fistula after pancreaticoduodenectomy. J Gastrointest Surg 22(10):1743–1751. https://doi.org/10.1007/s11605-018-3813-y
Kawai M, Tani M, Terasawa H et al (2006) Early removal of prophylactic drains reduces the risk of intra-abdominal infections in patients with pancreatic head resection: prospective study for 104 consecutive patients. Ann Surg 244(1):1–7. https://doi.org/10.1097/01.sla.0000218077.14035.a6
Author information
Authors and Affiliations
Contributions
H. Imamura and H. Takahashi drafted the first manuscript. All the authors individually made substantial contributions to conception and design, and acquisition of data, and analysis and interpretation of data, and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by research ethics committee of Osaka International Cancer Institute with approval number of 18033–3.
Consent to participate
Appropriate consent was obtained from all research participants.
Consent for publication
All the authors read through the final version of the manuscript and approved for its publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Imamura, H., Takahashi, H., Wada, H. et al. Postoperative aggressive diuresis prevents postoperative tissue edema and complications in patients undergoing distal pancreatectomy. Langenbecks Arch Surg 407, 645–654 (2022). https://doi.org/10.1007/s00423-021-02357-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02357-9