Abstract
Purpose
This retrospective, single-center study aimed to investigate the importance of chemotherapy and to come up with the optimal liver resection margin length for patients with resectable colorectal liver metastasis (CRLM).
Methods
Patients who had undergone any form of liver resection for CRLM were reviewed and analyzed. The analyses were broken down into three parts: (1) overall effect of chemotherapy, (2) effect of chemotherapy with positive/negative resection margin, and (3) result of discriminative analysis with optimal margin length analysis.
Results
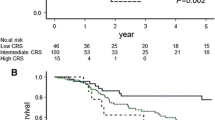
In total, 381 patients were studied. Among them, 279 received chemotherapy whereas 102 did not. Survival was significantly better in patients with chemotherapy (5-year, 43.6% vs. 25.8%) (p < 0.001). Patients who received chemotherapy (n = 93) with negative margins had better survival than patients (n = 8) with positive margins (5-year, 28.1% vs. 0%) (p = 0.019). On multivariate analysis, margin involvement was the poor prognostic factor for survival. Patients who had chemotherapy (n = 238) with negative margin showed a trend of better survival than patients (n = 41) with positive margins (5-year, 45.7% vs. 29.3%) (p = 0.085). Patients (n = 93) with negative margin and no chemotherapy and patients (n = 41) with positive margin and chemotherapy had comparable survival at 5 years (p = 0.422). On multivariate analysis, tumor number was the prognostic factor for survival. By the discriminant method, 1.09 cm (sensitivity 0.242, specificity 0.718) was determined as the cut-off for optimal margin length. Patients who had margin ≥ 1.09 cm (n = 81) enjoyed significantly better survival (5-year, 54.3% vs. 33.5%) (p = 0.041). On multivariate analysis, margin length ≥ 1.09 cm was the prognostic factor for favorable survival.
Conclusion
The results demonstrated the important effect of perioperative chemotherapy and negative margin liver resection in management of patients suffered from CRLM.





Similar content being viewed by others
References
Abdalla EK, Vauthey JN, Ellis LM, Ellis V, Pollock R, Broglio KR, Hess K, Curley SA (2004) Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg 239(6):818–825 discussion 825-7
Minagawa M, Makuuchi M, Torzilli G, Takayama T, Kawasaki S, Kosuge T, Yamamoto J, Imamura H (2000) Extension of the frontiers of surgical indications in the treatment of liver metastases from colorectal cancer: long-term results. Ann Surg 231(4):487–499
Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, Curley SA, Loyer EM, Muratore A, Mentha G, Capussotti L, Vauthey JN (2005) Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg 241(5):715–722 discussion 722-4
Spelt L, Andersson B, Nilsson J, Andersson R (2012) Prognostic models for outcome following liver resection for colorectal cancer metastases: a systematic review. Eur J Surg Oncol 38(1):16–24
Shirabe K, Takenaka K, Gion T, Fujiwara Y, Shimada M, Yanaga K, Maeda T, Kajiyama K, Sugimachi K (1997) Analysis of prognostic risk factors in hepatic resection for metastatic colorectal carcinoma with special reference to the surgical margin. Br J Surg 84(8):1077–1080
Cady B, Jenkins RL, Steele GD Jr, Lewis WD, Stone MD, McDermott WV, Jessup JM, Bothe A, Lalor P, Lovett EJ, Lavin P, Linehan DC (1998) Surgical margin in hepatic resection for colorectal metastasis: a critical and improvable determinant of outcome. Ann Surg 227(4):566–571
Elias D, Cavalcanti A, Sabourin JC, Lassau N, Pignon JP, Ducreux M, Coyle C, Lasser P (1998) Resection of liver metastases from colorectal cancer: the real impact of the surgical margin. Eur J Surg Oncol 24(3):174–179
Kato T, Yasui K, Hirai T, Kanemitsu Y, Mori T, Sugihara K, Mochizuki H, Yamamoto J (2003) Therapeutic results for hepatic metastasis of colorectal cancer with special reference to effectiveness of hepatectomy: analysis of prognostic factors for 763 cases recorded at 18 institutions. Dis Colon Rectum 46(10 Suppl):S22–S31
Capussotti L, Muratore A, Mulas MM, Massucco P, Aglietta M (2006) Neoadjuvant chemotherapy and resection for initially irresectable colorectal liver metastases. Br J Surg 93(8):1001–1006
de Haas RJ, Wicherts DA, Flores E, Azoulay D, Castaing D, Adam R (2008) R1 resection by necessity for colorectal liver metastases: is it still a contraindication to surgery? Ann Surg 248(4):626–637
Fan ST (2010) Liver functional reserve estimation: state of the art and relevance for local treatments: the Eastern perspective. J Hepatobiliary Pancreat Sci 17(4):380–384
Chan SC, Liu CL, Lo CM, Lam BK, Lee EW, Wong Y, Fan ST (2006) Estimating liver weight of adults by body weight and gender. World J Gastroenterol 12(14):2217–2222
She WH, Chan ACY, Ma KW, Dai WC, Chok KSH, Cheung TT, Lo CM (2018) Anterior approach to major resection for colorectal liver metastasis. J Gastrointest Surg 22:1928–1938
She WH, Chan AC, Poon RT et al (2015) Defining an optimal surgical strategy for synchronous colorectal liver metastases: staged versus simultaneous resection? ANZ J Surg 85(11):829–833
Jonker DJ, Spithoff K, Maroun J, Gastrointestinal Cancer Disease Site Group of Cancer Care Ontario’s Program in Evidence-based Care (2011) Adjuvant systemic chemotherapy for stage II and III colon cancer after complete resection: an updated practice guideline. Clin Oncol (R Coll Radiol) 23(5):314–322
Meyers BM, Cosby R, Quereshy F, Jonker D (2016) Adjuvant systemic chemotherapy for stages II and III colon cancer after complete resection: a clinical practice guideline. Curr Oncol 23(6):418–424
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–4
Blazer DG 3rd, Kishi Y, Maru DM et al (2008) Pathologic response to preoperative chemotherapy: a new outcome end point after resection of hepatic colorectal metastases. J Clin Oncol 26(33):5344–5351
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, Bechstein WO, Primrose JN, Walpole ET, Finch-Jones M, Jaeck D, Mirza D, Parks RW, Mauer M, Tanis E, van Cutsem E, Scheithauer W, Gruenberger T, EORTC Gastro-Intestinal Tract Cancer Group, Cancer Research UK, Arbeitsgruppe Lebermetastasen und–tumoren in der Chirurgischen Arbeitsgemeinschaft Onkologie (ALM-CAO), Australasian Gastro-Intestinal Trials Group (AGITG), Fédération Francophone de Cancérologie Digestive (FFCD) (2013) Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol 14(12):1208–1215
Chan GHJ, Chee CE (2019) Making sense of adjuvant chemotherapy in colorectal cancer. J Gastrointest Oncol 10(6):1183–1192
Hasegawa K, Saiura A, Takayama T, Miyagawa S, Yamamoto J, Ijichi M, Teruya M, Yoshimi F, Kawasaki S, Koyama H, Oba M, Takahashi M, Mizunuma N, Matsuyama Y, Watanabe T, Makuuchi M, Kokudo N (2016) Adjuvant oral uracil-tegafur with leucovorin for colorectal cancer liver metastases: a randomized controlled trial. PLoS One 11(9):e0162400
Mitry E, Fields AL, Bleiberg H et al (2008) Adjuvant chemotherapy after potentially curative resection of metastases from colorectal cancer: a pooled analysis of two randomized trials. J Clin Oncol 26(30):4906–4911
Portier G, Elias D, Bouche O, Rougier P, Bosset JF, Saric J, Belghiti J, Piedbois P, Guimbaud R, Nordlinger B, Bugat R, Lazorthes F, Bedenne L (2006) Multicenter randomized trial of adjuvant fluorouracil and folinic acid compared with surgery alone after resection of colorectal liver metastases: FFCD ACHBTH AURC 9002 trial. J Clin Oncol 24(31):4976–4982
Kanemitsu Y, Shimizu Y, Mizusawa J et al (2020) A randomized phase II/III trial comparing hepatectomy followed by mFOLFOX6 with hepatectomy alone for liver metastasis from colorectal cancer: JCOG0603 study. J Clin Oncol 38(15_suppl):4005
Ayez N, Lalmahomed ZS, Eggermont AM et al (2012) Outcome of microscopic incomplete resection (R1) of colorectal liver metastases in the era of neoadjuvant chemotherapy. Ann Surg Oncol 19(5):1618–1627
Bodingbauer M, Tamandl D, Schmid K, Plank C, Schima W, Gruenberger T (2007) Size of surgical margin does not influence recurrence rates after curative liver resection for colorectal cancer liver metastases. Br J Surg 94(9):1133–1138
Andreou A, Aloia TA, Brouquet A, Dickson PV, Zimmitti G, Maru DM, Kopetz S, Loyer EM, Curley SA, Abdalla EK, Vauthey JN (2013) Margin status remains an important determinant of survival after surgical resection of colorectal liver metastases in the era of modern chemotherapy. Ann Surg 257(6):1079–1088
Hamady ZZ, Lodge JP, Welsh FK et al (2014) One-millimeter cancer-free margin is curative for colorectal liver metastases: a propensity score case-match approach. Ann Surg 259(3):543–548
Truant S, Sequier C, Leteurtre E et al (2015) Tumour biology of colorectal liver metastasis is a more important factor in survival than surgical margin clearance in the era of modern chemotherapy regimens. HPB (Oxford) 17(2):176–184
Makowiec F, Bronsert P, Klock A, Hopt UT, Neeff HP (2018) Prognostic influence of hepatic margin after resection of colorectal liver metastasis: role of modern preoperative chemotherapy. Int J Color Dis 33(1):71–78
Memeo R, de Blasi V, Adam R et al (2018) Margin status is still an important prognostic factor in hepatectomies for colorectal liver metastases: a propensity score matching analysis. World J Surg 42(3):892–901
Pandanaboyana S, White A, Pathak S, Hidalgo EL, Toogood G, Lodge JP, Prasad KR (2015) Impact of margin status and neoadjuvant chemotherapy on survival, recurrence after liver resection for colorectal liver metastasis. Ann Surg Oncol 22(1):173–179
Eveno C, Karoui M, Gayat E, Luciani A, Auriault ML, Kluger MD, Baumgaertner I, Baranes L, Laurent A, Tayar C, Azoulay D, Cherqui D (2013) Liver resection for colorectal liver metastases with peri-operative chemotherapy: oncological results of R1 resections. HPB (Oxford) 15(5):359–364
Laurent C, Adam JP, Denost Q, Smith D, Saric J, Chiche L (2016) Significance of R1 resection for advanced colorectal liver metastases in the era of modern effective chemotherapy. World J Surg 40(5):1191–1199
Tranchart H, Chirica M, Faron M, Balladur P, Lefevre LB, Svrcek M, de Gramont A, Tiret E, Paye F (2013) Prognostic impact of positive surgical margins after resection of colorectal cancer liver metastases: reappraisal in the era of modern chemotherapy. World J Surg 37(11):2647–2654
Procopio F, Vigano L, Cimino M et al (2020) Does KRAS mutation status impact the risk of local recurrence after R1 vascular resection for colorectal liver metastasis? An observational cohort study. Eur J Surg Oncol 46(5):818–824
Torzilli G, Procopio F, Vigano L et al (2018) Hepatic vein management in a parenchyma-sparing policy for resecting colorectal liver metastases at the caval confluence. Surgery 163(2):277–284
Vigano L, Procopio F, Cimino MM et al (2016) Is tumor detachment from vascular structures equivalent to R0 resection in surgery for colorectal liver metastases? An observational cohort. Ann Surg Oncol 23(4):1352–1360
Hosokawa I, Allard MA, Gelli M, Ciacio O, Vibert E, Cherqui D, Sa Cunha A, Castaing D, Miyazaki M, Adam R (2016) Long-term survival benefit and potential for cure after R1 resection for colorectal liver metastases. Ann Surg Oncol 23(6):1897–1905
Sadot E, Groot Koerkamp B, Leal JN et al (2015) Resection margin and survival in 2368 patients undergoing hepatic resection for metastatic colorectal cancer: surgical technique or biologic surrogate? Ann Surg 262(3):476–485 discussion 483-5
Dhir M, Lyden ER, Wang A, Smith LM, Ullrich F, Are C (2011) Influence of margins on overall survival after hepatic resection for colorectal metastasis: a meta-analysis. Ann Surg 254(2):234–242
Wakai T, Shirai Y, Sakata J, Valera VA, Korita PV, Akazawa K, Ajioka Y, Hatakeyama K (2008) Appraisal of 1 cm hepatectomy margins for intrahepatic micrometastases in patients with colorectal carcinoma liver metastasis. Ann Surg Oncol 15(9):2472–2481
Peloso A, Franchi E, Canepa MC, Barbieri L, Briani L, Ferrario J, Bianco C, Quaretti P, Brugnatelli S, Dionigi P, Maestri M (2013) Combined use of intraoperative ultrasound and indocyanine green fluorescence imaging to detect liver metastases from colorectal cancer. HPB (Oxford) 15(12):928–934
Acknowledgements
The authors would like to thank Mr. Kim Yuen (BSc (Hons), Stat and Comp) for all the statistical work for the study.
Author information
Authors and Affiliations
Contributions
She WH was responsible for study design, literature search, collection, analysis and interpretation of data, and manuscript drafting; Cheung TT was responsible for study design, analysis and interpretation of data, and writing and critical revision of manuscript; Ma KW, Tsang SHY, Dai WC, and Chan ACY were responsible for study design and critical revision of manuscript; Lo CM was responsible for study design; Cheung TT is the guarantor.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The use of the data set was previously approved by the Ethics Committee of the Queen Mary Hospital of the University of Hong Kong. Informed consent was obtained from all individual participants included in the study. Due to the nature of this retrospective analysis, further institutional approval was not necessary.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
She, W.H., Cheung, T.T., Ma, K.W. et al. Relevance of chemotherapy and margin status in colorectal liver metastasis. Langenbecks Arch Surg 406, 2725–2737 (2021). https://doi.org/10.1007/s00423-021-02205-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02205-w