Abstract
Purpose
Loop ileostomy is performed in rectal cancer surgery to decrease the impact of anastomotic leak but it is associated with a significant complication rate. This study aimed to analyze the morbidity related to diverting ileostomy and to identify factors predictive of complications related to stoma management and reversal, as well as conversion into a permanent ileostomy.
Methods
A retrospective study was conducted on 112 patients submitted to oncological rectal resection and defunctioning ileostomy in a Portuguese colorectal unit between March 2012 and March 2019.
Results
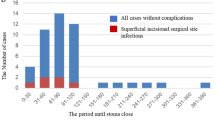
Loop ileostomy was responsible for 13% of index surgery morbidity and 15% of patients’ readmissions due to high output, stoma stenosis and parastomal hernia. Ileostomy was reversed in 89% cases with 7% Clavien-Dindo ≥ IIIb complications. An association was established between diabetes and higher stoma management morbidity (OR: 3.28 [95% CI: 1.039-10.426]. p = 0.041). Likewise, diabetes (OR: 0.17 [95% CI: 0.038; 6.90], p=0.015), oncological disease stage ≥ III (OR: 0.10 [95% CI: 0.005; 0.656], p=0.047) and index rectal surgery morbidity (OR: 0.23 [95% CI: 0.052; 0.955], p=0.041) were associated with less ileostomy closure. Complications of the index surgery also related to higher stoma reversal morbidity (OR: 5.11 [95% CI: 1.665; 16.346], p=0.005).
Conclusions
Diabetes and complications of index rectal surgery were identified as predictive of ileostomy morbidity, closure rate and associated complications. It is essential to adjust treatment decisions to patient’s morbidity risk and adopt a more selective approach concerning the use of an ileostomy.

Similar content being viewed by others
References
Rubinkiewicz M et al (2019) Investigating risk factors for complications after ileostomy reversal in low anterior rectal resection patients: an observational study. J Clin Med 8(10):1567
Gustafsson CP, Gunnarsson U, Dahlstrand U, Lindforss U (2018) Loop-ileostomy reversal—patient-related characteristics influencing time to closure. Int J Color Dis 33(5):593–600
Ahmad NZ, Abbas MH, Khan SU, Parvaiz A (2021) A meta-analysis of the role of diverting ileostomy after rectal cancer surgery. Int J Colorectal Dis 36(3):445–455
Ng ZQ, Levitt M, Platell C (2020) The feasibility and safety of early ileostomy reversal: a systematic review and meta-analysis. ANZ J Surg 90(9):1580–1587
Hanna MH, Vinci A, Pigazzi A (2015) Diverting ileostomy in colorectal surgery: when is it necessary? Langenbeck's Arch Surg 400(2):145–152
Garfinkle R, Filion KB, Bhatnagar S, Sigler G, Banks A, Letarte F, Liberman S, Brown CJ, Boutros M (2019) Prediction model and web-based risk calculator for postoperative ileus after loop ileostomy closure. Br J Surg 106(12):1676–1684
Prassas D, Vossos V, Rehders A, Knoefel WT, Krieg A (2020) Loop ileostomy versus loop colostomy as temporary deviation after anterior resection for rectal cancer. Langenbeck's Arch Surg 405(8):1147–1153
Fielding A, Woods R, Moosvi SR, Wharton RQ, Speakman CTM, Kapur S, Shaikh I, Hernon JM, Lines SW, Stearns AT (2020) Renal impairment after ileostomy formation: a frequent event with long-term consequences. Color Dis 22(3):269–278
Clausen FB, Dohrn N, Hölmich ER, Klein M, Gögenur I (2021) Safety of early ileostomy closure: a systematic review and meta-analysis of randomized controlled trials. Int J Color Dis 36(2):203–212
Farag S, Rehman S, Sains P, Baig MK, Sajid MS (2017) Early vs delayed closure of loop defunctioning ileostomy in patients undergoing distal colorectal resections: an integrated systematic review and meta-analysis of published randomized controlled trials. Color Dis 19(12):1050–1057
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tiret E, Moriya Y, Laurberg S, den Dulk M, van de Velde C, Büchler MW (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147(3):339–351
Chambers WM, Mortensen NJM (2004) Postoperative leakage and abscess formation after colorectal surgery. Best Pract Res Clin Gastroenterol 18(5):865–880
Messaris E et al (2015) Is a diverting ostomy needed in mid-high rectal cancer patients undergoing a low anterior resection after neoadjuvant chemoradiation? An NSQIP analysis. Surg (United States) 158(3):686–691
Sherman KL, Wexner SD (2017) Considerations in stoma reversal. Clin Colon Rectal Surg 30(3):172–177
Luglio G (2011) Loop ileostomy reversal after colon and rectal surgery. Arch Surg 146(10):1191
Tao K, Gao J (2018) Risk factors for anastomotic leakage after rectal cancer surgery. Zhonghua Wei Chang Wai Ke Za Zhi 21(4):384–387
O’Leary DP, Fide CJ, Foy C, Lucarotti ME (2001) Quality of life after low anterior resection with total mesorectal excision and temporary loop ileostomy for rectal carcinoma. Br J Surg 88(9):1216–1220
Hallböök O, Matthiessen P, Leinsköld T, Nyström PO, Sjödahl R (2002) Safety of the temporary loop ileostomy. Color Dis 4(5):361–364
García-Botello SA, García-Armengol J, García-Granero E, Espí A, Juan C, López-Mozos F, Lledó S (2004) A prospective audit of the complications of loop ileostomy construction and takedown. Dig Surg 21(5–6):440–446
Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E, Purkayastha S (2009) The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Color Dis 24(6):711–723
Abegg RM, Brokelman W, Van Bebber IP, Bosscha K, Prins HA, Lips DJ (2014) Results of construction of protective loop ileostomies and reversal surgery for colorectal surgery. Eur Surg Res 52(1–2):63–72
Platell C, Barwood N, Makin G (2005) Clinical utility of a de-functioning loop ileostomy. ANZ J Surg 75(3):147–151
Gadan S, Lindgren R, Floodeen H, Matthiessen P (2019) Reversal of defunctioning stoma following rectal cancer surgery: are we getting better? A population-based single centre experience. ANZ J Surg 89(4):403–407
Alqahtani M, Garfinkle R, Zhao K, Vasilevsky CA, Morin N, Ghitulescu G, Faria J, Boutros M (2020) Can we better predict readmission for dehydration following creation of a diverting loop ileostomy: development and validation of a prediction model and web-based risk calculator. Surg Endosc 34(7):3118–3125
Kaidar-Person O, Person B, Wexner SD (2005) Complications of construction and closure of temporary loop ileostomy. J Am Coll Surg 201(5):759–773
Silva MA, Ratnayake G, Deen KI (2003) Quality of life of stoma patients: temporary ileostomy versus colostomy. World J Surg 27(4):421–424
Wexner SD, Taranow DA, Johansen OB, Itzkowitz F, Daniel N, Nogueras JJ, Jagelman DG (1993) Loop ileostomy is a safe option for fecal diversion. Dis Colon Rectum 36(4):349–354
Köckerling F, Geers P, Schneider C, Scheidbach H, Rose J, Yildirim C (2005) Complications in laparoscopic colorectal surgery: results of a multicentre trial. Tech Coloproctol 8(S1):s25–s28
Schneider V, Lee LD, Stroux A, Buhr HJ, Ritz JP, Kreis ME, Lauscher JC (2016) Risk factors for reoperation after ileostomy reversal – results from a prospective cohort study. Int J Surg 36:233–239
Sharma A, Deeb AP, Rickles AS, Iannuzzi JC, Monson JRT, Fleming FJ (2013) Closure of defunctioning loop ileostomy is associated with considerable morbidity. Color Dis 15(4):458–462
Park J, Angenete E, Bock D, Correa-Marinez A, Danielsen AK, Gehrman J, Haglind E, Jansen JE, Skullman S, Wedin A, Rosenberg J (2020) Cost analysis in a randomized trial of early closure of a temporary ileostomy after rectal resection for cancer (EASY trial). Surg Endosc 34(1):69–76
Hacim NA, Akbas A, Meric S, Altinel Y, Karabay O, Yavuz E (2020) Diverting ileostomy duration is the main determinant of ileostomy-related complications after surgical treatment of rectum cancer. J Oncol 2020:6–11
Wang L et al (2020) Early versus late closure of temporary ileostomy after rectal cancer surgery: a meta-analysis. Surg Today
Menahem B, Lubrano J, Vallois A, Alves A (2018) Early closure of defunctioning loop ileostomy: is it beneficial for the patient? A meta-analysis. World J Surg 42(10):3171–3178
Copaescu C, Smeu B, Catanescu E, Andrei D, Tomulescu V (2019) Early laparoscopic ileostomy reversal after rectal cancer surgery - technique and outcomes. Chir. 114(3):392–400
Pedrazzani C, Secci F, Fernandes E, Jelovskijs I, Turri G, Conti C, Ruzzenente A, Guglielmi A (2019) Early ileostomy reversal after minimally invasive surgery and ERAS program for mid and low rectal cancer. Updat Surg 71(3):485–492
Lasithiotakis K, Aghahoseini A, Alexander D (2016) Is early reversal of defunctioning ileostomy a shorter, easier and less expensive operation? World J Surg 40(7):1737–1740
Sebastian A, Stupart D, Watters DA (2019) Loop ileostomy reversal after laparoscopic versus open rectal resection. ANZ J Surg 89(3):E52–E55
Abrisqueta J, Abellan I, Luján J, Hernández Q, Parrilla P (2014) Stimulation of the efferent limb before ileostomy closure: a randomized clinical trial. Dis Colon Rectum 57(12):1391–1396
Availability of data and material
The datasets analyzed during the current study are available in the Hospital Beatriz Ângelo informatics hospital database (Soarien), available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author information
Authors and Affiliations
Contributions
Susana Ourô: study conception and design, acquisition, analysis and interpretation of the data, drafting of the article, critical revision of the article for important intellectual content, final approval of the article; Marisa P Ferreira: study conception and design, acquisition, analysis and interpretation of the data, drafting of the article, critical revision of the article for important intellectual content, final approval of the article; Diogo Albergaria: critical revision of the article for important intellectual content, final approval of the article; Rui Maio: critical revision of the article for important intellectual content, final approval of the article.
Corresponding author
Ethics declarations
Ethics approval/Consent to participate/Consent for publication
The present study was approved by the Ethics Committee and Institutional Review Board of Hospital Beatriz Ângelo with no formal Informed consent required due to its methodology and anonymity. The study protocol was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Susana Ourô and Marisa P. Ferreira are co-first authors
Supplementary Information
ESM 1
(DOCX 43 kb)
Rights and permissions
About this article
Cite this article
Ourô, S., Ferreira, M.P., Albergaria, D. et al. Loop ileostomy in rectal cancer surgery: factors predicting reversal and stoma related morbidity. Langenbecks Arch Surg 406, 843–853 (2021). https://doi.org/10.1007/s00423-021-02169-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02169-x