Abstract
Purpose
A Roux-en-Y hepaticojejunostomy (HJ) is the preferred method for repairing bile duct injuries (BDIs). The American College of Surgeons (ACS) established the National Surgical Quality Improvement Program (NSQIP) online risk calculator to predict risks for morbidity and mortality. The objective of the study is to assess the use of the ACS NSQIP calculator for patients undergoing HJ for BDI repairs outside the NSQIP cohort.
Methods
An IRB-approved retrospective study of Bismuth-Strasberg type E BDI HJ (2008-2020) was performed. Clinical data was introduced in the NSQIP calculator, and morbidity and mortality were determined. Perioperative risk factors were obtained. Comparisons of postoperative complications and NSQIP-predicted complication rate were carried out.
Results
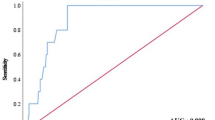
Eighty-two patients were included (age: 42.2 ± 15.7 years; 81% female; BMI 27.1 ± 4.4 kg/m2). The most common injury was E4 (36.3%). A total of 40.2% patients had a 30-day complication. Mortality was 2.4%. Preoperative sepsis and high body mass index (p = 0.01) were significantly related to complications (p = 0.01) (univariate analysis). Older age (p = 0.01) and higher ASA class (p = 0.02) were significantly related to mortality (univariate analysis). None was statistically significant in multivariate analysis. Comparison between morbidity and mortality and the calculated NSQIP was not statistically significant. Postoperative mortality had a statistically significant trend (C-value = 0.72, p = 0.055).
Conclusion
Preoperative sepsis, high body mass index, age, and ASA classification were associated with worse outcomes in HJ BDI repair. The ACS NSQIP calculator did not have a good performance in a population outside the NSQIP data. Further larger studies will need to corroborate these results.
Similar content being viewed by others
Data availability
Yes.
References
Gouma DJ, Go PM (1994) Bile duct injury during laparoscopic and conventional cholecystectomy. J Am Coll Surg 178(3):229–233
Tantia O, Jain M, Khanna S, Sen B (2008) Iatrogenic biliary injury: 13,305 cholecystectomies experienced by a single surgical team over more than 13 years. Surg Endosc 22(4):1077–1086
Dominguez-Rosado I, Mercado MA, Kauffman C, Ramirez-del Val F, Elnecavé-Olaiz A, Zamora-Valdés D (2014) Quality of life in bile duct injury: 1-, 5-, and 10-year outcomes after surgical repair. J Gastrointest Surg 18(12):2089–2094
Flores-Rangel GA, Chapa-Azuela O, Rosales AJ, Roca-Vasquez C, Böhm-González ST (2018) Quality of life in patients with background of iatrogenic bile duct injury. World J Surg 42(9):2987–2991
Bismuth H, Majno PE (2001) Biliary strictures: classification based on the principles of surgical treatment. World J Surg 25(10):1241–1244
Strasberg SM, Hertl M, Soper NJ (1995) An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180(1):101–125
Mercado MA, Dominguez I (2011) Classification and management of bile duct injuries. World J Gastrointest Surg (4):43–48
Díaz-Martínez J, Chapa-Azuela O, Roldan-García JA, Flores-Rangel GA (2020) Bile duct injuries after cholecystectomy, analysis of constant risk. Annals of hepato-biliary-pancreatic surgery 24(2):150–155
Mercado MA, Franssen B, Dominguez I, Arriola-Cabrera JC, Ramirez-Del Val F, Elnecave-Olaiz A et al (2011) Transition from a low: to a high-volume centre for bile duct repair: changes in technique and improved outcome. HPB (Oxford) (11):767–773
Sicklick JK, Camp MS, Lillemoe KD, Melton GB, Yeo CJ, Campbell KA et al (2005) Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann Surg (5):786–792 discussion 93-5
Walsh RM, Henderson JM, Vogt DP, Brown N (2007) Long-term outcome of biliary reconstruction for bile duct injuries from laparoscopic cholecystectomies. Surgery 142(4):450–456 discussion 6-7
Cho JY, Baron TH, Carr-Locke DL, Chapman WC, Costamagna G, de Santibanes E et al (2018) Proposed standards for reporting outcomes of treating biliary injuries. HPB (Oxford) (4):370–378
Bilimoria KY, Liu Y, Paruch JL, Zhou L, Kmiecik TE, Ko CY et al (2013) Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg 217(5):833-42.e1-3
Liu Y, Cohen ME, Hall BL, Ko CY, Bilimoria KY (2016) Evaluation and enhancement of calibration in the American College of Surgeons NSQIP surgical risk calculator. J Am Coll Surg 223(2):231–239
Kneuertz PJ, Pitt HA, Bilimoria KY, Smiley JP, Cohen ME, Ko CY, Pawlik TM (2012) Risk of morbidity and mortality following hepato-pancreato-biliary surgery. J Gastrointest Surg 16(9):1727–1735
Pitt HA, Kilbane M, Strasberg SM, Pawlik TM, Dixon E, Zyromski NJ et al (2009) ACS-NSQIP has the potential to create an HPB-NSQIP option. HPB (Oxford) 11(5):405–413
Beal EW, Lyon E, Kearney J, Wei L, Ethun CG, Black SM, Dillhoff M, Salem A, Weber SM, Tran TB, Poultsides G, Shenoy R, Hatzaras I, Krasnick B, Fields RC, Buttner S, Scoggins CR, Martin RCG, Isom CA, Idrees K, Mogal HD, Shen P, Maithel SK, Pawlik TM, Schmidt CR (2017) Evaluating the American College of Surgeons National Surgical Quality Improvement project risk calculator: results from the U.S. Extrahepatic Biliary Malignancy Consortium. HPB (Oxford) 19(12):1104–1111
Ismael HN, Cox S, Cooper A, Narula N, Aloia T (2017) The morbidity and mortality of hepaticojejunostomies for complex bile duct injuries: a multi-institutional analysis of risk factors and outcomes using NSQIP. HPB (Oxford) 19(4):352–358
Martinez-Mier G, Luna-Ortiz HJ, Hernandez-Herrera N, Zilli-Hernandez S (2018) Lajud-Barquin FA. [Factores de riesgo asociados a las complicaciones y a la falla terapeutica en las reconstrucciones de lesiones de via biliar secundarias a colecistectomia]. Cir Cir 86(6):491–498
Martínez-Mier G, Moreno-Ley PI, Mendez-Rico D (2020) Factors associated with patency loss and actuarial patency rate following post-cholecystectomy bile duct injury repair: long-term follow-up. Langenbecks Arch Surg 405(7):999–1006
Cho JY, Jaeger AR, Sanford DE, Fields RC, Strasberg SM (2015) Proposal for standardized tabular reporting of observational surgical studies illustrated in a study on primary repair of bile duct injuries J. Am Coll Surg 221(3):678–688
Tang ST, Yang Y, Wang Y, Mao YZ, Li SW, Tong QS et al (2015) Laparoscopic choledochal cyst excision, hepaticojejunostomy, and extracorporeal Roux-en-Y anastomosis: a technical skill and intermediate-term report in 62 cases. Surg Endosc (2):416–422
Jackson N, Dugan A, Davenport D, Daily M, Shah M, Berger J et al (2016) Risk factors for increased resource utilization and critical care complications in patients undergoing hepaticojejunostomy for biliary injuries. HPB (Oxford) 18(9):712–717
Rueda-De-Leon A, Dominguez-Rosado I, Contreras AG, Vilatoba M, Mercado MA (2020) Disparities in bile duct injury care. Surg Endosc 34(3):1324–1329
Cuendis-Velazquez A, Trejo-Avila M, Bada-Yllan O, Cardenas-Lailson E, Morales-Chavez C, Fernandez-Alvarez L et al (2019) A new era of bile duct repair: robotic-assisted versus laparoscopic hepaticojejunostomy. J Gastrointest Surg. 23(3):451–459
Martínez-Mier G, Moreno-Ley PI, Esquivel-Torres S, Gonzalez-Grajeda JL, Mendez-Rico D (2020) Differences in post-cholecystectomy bile duct injury care: a comparative analysis of 2 different health-care public institutions in a low- and middle-income country: Southeast Mexico. Dig Surg Aug 23:1–8. https://doi.org/10.1159/000509706 Epub ahead of print
Schreuder AM, Nunez Vas BC, Booij KAC, van Dieren S, Besselink MG, Busch OR et al (2020) Optimal timing for surgical reconstruction of bile duct injury: meta-analysis. BJS Open 4(5):776–786
Authors´ contributions
Gustavo Martinez-Mier: design of the work, data acquisition, data analysis, interpretation of the data, manuscript draft, critical revision of the manuscript, and final approval of the manuscript. Pedro I. Moreno-Ley: data acquisition, data analysis, interpretation of the data, manuscript draft, critical revision of the manuscript, and final approval of the manuscript. Daniel Mendez-Rico: data acquisition, data analysis, critical revision of the manuscript, and final approval of the manuscript. Fortino Gonzalez-Gonzalez: data acquisition, data analysis, interpretation of the data, and final approval of the manuscript. Andrea Nachon-Acosta: data acquisition, data analysis, interpretation of the data, and final approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
IRB committees (IMSS: R-3001-2015-54 and SESVER: R:18/01/2012).
Consent to participate
Signed by patients.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martínez-Mier, G., Moreno-Ley, P.I., Mendez-Rico, D. et al. Performance of the American College of Surgeons National Surgical Quality Improvement calculator for early postoperative outcomes following bile duct repair hepaticojejunostomy. Langenbecks Arch Surg 406, 1935–1942 (2021). https://doi.org/10.1007/s00423-021-02133-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02133-9