Abstract
Purpose
Abdominoperineal resection of the rectum has evolved over the last century, with few modifications until 2007, when extralevator abdominoperineal resection was introduced, which improved local disease control but resulted in a significant rise in perineal complications. We adopted a modified approach in which dissection was tailored according to magnetic resonance-defined tumour involvement. The aim of this study was to assess short-term and long-term oncological outcomes following a tailored abdominoperineal resection (APR) approach.
Methods
This study was a retrospective review of prospectively maintained databases at three centres: Portsmouth NHS Trust (UK), Poole General Hospital (UK) and Champalimaud’s Cancer Foundation, Portugal. The study included consecutive patients who underwent abdominoperineal resection from October 2008 until April 2018 under the supervision of the senior author. Oncological outcomes, including overall survival and disease-free survival, were used as the main outcome measures.
Results
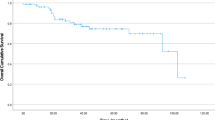
A total of 584 patients underwent rectal cancer surgery during the study period. The APR ratio was 65/584 (11%). The median age was 66 years. Neoadjuvant treatment was administered to 74% of patients. Of the patients, 91% underwent surgery via a minimally invasive approach. The median hospital stay was 7 days. Patients were followed up for a median of 41 months. Only four patients had positive resection margins. The 5-year overall and disease-free survival rates were 64% and 62%, respectively.
Conclusion
Our data suggest that tailored APR has similar short-term and long-term oncological outcomes compared with extralevator abdominoperineal resection but reduced perineal wound complications. We believe this approach could be a safe alternative but recommend a larger sample size to accurately assess its effectiveness.

Similar content being viewed by others
References
Perry WB, Connaughton JC (2007) Abdominoperineal resection: how is it done and what are the results? Clin Colon Rectal Surg 20:213–220. https://doi.org/10.1055/s-2007-984865
Miles WE (1908) A method of performing abdomino-perineal excision for carcinoma of the rectum and of the terminal portion of the pelvic colon. CA Cancer J Clin 21:361–364. https://doi.org/10.3322/canjclin.21.6.361
Näsvall P, Dahlstrand U, Löwenmark T, Rutegård J, Gunnarsson U, Strigård K (2017) Quality of life in patients with a permanent stoma after rectal cancer surgery. Qual Life Res 26:55–64. https://doi.org/10.1007/s11136-016-1367-6
Guillou PJ, Quirke P, Thorpe H et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726. https://doi.org/10.1016/S0140-6736(05)66545-2
Morris EJA, Birch R, West NP, Finan PJ, Forman D, Fairley L, Quirke P (2011) Low abdominoperineal excision rates are associated with high-workload surgeons and lower tumour height. Is further specialization needed? Colorectal Dis 13:755–761. https://doi.org/10.1111/j.1463-1318.2010.02263.x
Tekkis PP, Heriot AG, Smith J, Thompson MR, Finan P, Stamatakis JD, the Association of Coloproctology of Great Britain and Ireland (2005) Comparison of circumferential margin involvement between restorative and nonrestorative resections for rectal cancer. Colorectal Dis 7:369–374. https://doi.org/10.1111/j.1463-1318.2005.00767.x
Heald RJ, Smedh RK, Kald A et al (1997) Abdominoperineal excision of the rectum--an endangered operation. Norman Nigro Lectureship. Dis Colon Rectum 40:747–751. https://doi.org/10.1007/BF02055425
Quirke P, Steele R, Monson J et al (2009) Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet 373:821–828. https://doi.org/10.1016/S0140-6736(09)60485-2
MERCURY Study Group (2007) Extramural depth of tumor invasion at thin-section MR in patients with rectal cancer: results of the MERCURY study. Radiology 243:132–139. https://doi.org/10.1148/radiol.2431051825
Peeters KCMJ, Marijnen CAM, Nagtegaal ID, Kranenbarg EK, Putter H, Wiggers T, Rutten H, Pahlman L, Glimelius B, Leer JW, van de Velde C, Dutch Colorectal Cancer Group (2007) The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg 246:693–701. https://doi.org/10.1097/01.sla.0000257358.56863.ce
Sebag-Montefiore D, Stephens RJ, Steele R et al (2009) Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet 373:811–820. https://doi.org/10.1016/S0140-6736(09)60484-0
Holm T, Ljung A, Häggmark T, Jurell G, Lagergren J (2007) Extended abdominoperineal resection with gluteus maximus flap reconstruction of the pelvic floor for rectal cancer. Br J Surg 94:232–238. https://doi.org/10.1002/bjs.5489
West NP, Finan PJ, Anderin C, Lindholm J, Holm T, Quirke P (2008) Evidence of the oncologic superiority of cylindrical abdominoperineal excision for low rectal cancer. J Clin Oncol 26:3517–3522. https://doi.org/10.1200/JCO.2007.14.5961
Tayyab M, Sharma A, Ragg JL, Macdonald AW, Gunn J, Hartley JE, Monson JR (2012) Evaluation of the impact of implementing the prone jackknife position for the perineal phase of abdominoperineal excision of the rectum. Dis Colon Rectum 55:316–321. https://doi.org/10.1097/DCR.0b013e31823e2424
Sayers AE, Patel RK, Hunter IA (2015) Perineal hernia formation following extralevator abdominoperineal excision. Colorectal Dis 17:351–355. https://doi.org/10.1111/codi.12843
Miskovic D, Foster J, Agha A, Delaney CP, Francis N, Hasegawa H, Karachun A, Kim SH, Law WL, Marks J, Morino M, Panis Y, Uriburu JCP, Wexner SD, Parvaiz A (2015) Standardization of laparoscopic total mesorectal excision for rectal cancer: a structured international expert consensus. Ann Surg 261:716–722. https://doi.org/10.1097/SLA.0000000000000823
Panteleimonitis S, Harper M, Hall S, Figueiredo N, Qureshi T, Parvaiz A (2018) Precision in robotic rectal surgery using the da Vinci Xi system and integrated table motion, a technical note. J Robot Surg 12:433–436. https://doi.org/10.1007/s11701-017-0752-7
Kehlet H, Wilmore DW (2002) Multimodal strategies to improve surgical outcome. Am J Surg 183:630–641. https://doi.org/10.1016/s0002-9610(02)00866-8
Holm T, Rutqvist LE, Johansson H, Cedermark B (1995) Abdominoperineal resection and anterior resection in the treatment of rectal cancer: results in relation to adjuvant preoperative radiotherapy. Br J Surg 82:1213–1216. https://doi.org/10.1002/bjs.1800820920
Lee M-TG, Chiu C-C, Wang C-C, Chang CN, Lee SH, Lee M, Hsu TC, Lee CC (2017) Trends and outcomes of surgical treatment for colorectal cancer between 2004 and 2012-an analysis using national inpatient database. Sci Rep 7:2006. https://doi.org/10.1038/s41598-017-02224-y
Pascual M, Salvans S, Pera M (2016) Laparoscopic colorectal surgery: current status and implementation of the latest technological innovations. World J Gastroenterol 22:704–717. https://doi.org/10.3748/wjg.v22.i2.704
Klein M, Fischer A, Rosenberg J, Gögenur I, Danish Colorectal Cancer Group (DCCG) (2015) Extralevatory abdominoperineal excision (ELAPE) does not result in reduced rate of tumor perforation or rate of positive circumferential resection margin: a nationwide database study. Ann Surg 261:933–938. https://doi.org/10.1097/SLA.0000000000000910
Lu S, Chang X, Yang X, Yu D, Huang Q, Wang F (2017) A meta-analysis on risk factors of postoperative perineal wound complications after abdominoperineal resection for rectal cancer. Zhonghua Wei Chang Wai Ke Za Zhi 20:1180–1187
Eriksen MT, Wibe A, Syse A, Haffner J, Wiig JN, on behalf of the Norwegian Rectal Cancer Group the Norwegian Gastrointestinal Cancer Group (2004) Inadvertent perforation during rectal cancer resection in Norway. Br J Surg 91:210–216. https://doi.org/10.1002/bjs.4390
Nagtegaal ID, van de Velde CJH, Marijnen CAM, van Krieken J, Quirke P, Dutch Colorectal Cancer Group, Pathology Review Committee (2005) Low rectal cancer: a call for a change of approach in abdominoperineal resection. J Clin Oncol 23:9257–9264. https://doi.org/10.1200/JCO.2005.02.9231
den Dulk M, Putter H, Collette L, Marijnen CAM, Folkesson J, Bosset JF, Rödel C, Bujko K, Påhlman L, van de Velde CJH (2009) The abdominoperineal resection itself is associated with an adverse outcome: the European experience based on a pooled analysis of five European randomised clinical trials on rectal cancer. Eur J Cancer 45:1175–1183. https://doi.org/10.1016/j.ejca.2008.11.039
Shihab OC, Brown G, Daniels IR, Heald RJ, Quirke P, Moran BJ (2010) Patients with low rectal cancer treated by abdominoperineal excision have worse tumors and higher involved margin rates compared with patients treated by anterior resection. Dis Colon Rectum 53:53–56. https://doi.org/10.1007/DCR.0b013e3181c70465
Kusters M, Marijnen CAM, van de Velde CJH, Rutten HJT, Lahaye MJ, Kim JH, Beets-Tan RGH, Beets GL (2010) Patterns of local recurrence in rectal cancer; a study of the Dutch TME trial. Eur J Surg Oncol 36:470–476. https://doi.org/10.1016/j.ejso.2009.11.011
De Nardi P, Summo V, Vignali A, Capretti G (2015) Standard versus extralevator abdominoperineal low rectal cancer excision outcomes: a systematic review and meta-analysis. Ann Surg Oncol 22:2997–3006. https://doi.org/10.1245/s10434-015-4368-8
Author information
Authors and Affiliations
Contributions
Muhammad Tayyab: conception, data collection/analysis, writing of the paper. Hammad Zaidi FRCS: conception, data collection/analysis, writing of the paper. Pedro Vieira MD: conception, data collection/analysis, writing of the paper. Tahseen Qureshi: conception, data collection/analysis, writing of the paper. Nuno Figueiredo: conception, data collection/analysis, writing of the paper. Amjad Parvaiz MD, FRCS: conception, data collection/analysis, writing of the paper, supervision.
Corresponding author
Ethics declarations
There are no conflicts of interest from any authors. Local institution ethical approval was obtained prior to data collection. The project did not require informed consent from patients, as no confidential information was used.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tayyab, M., Zaidi, H., Vieira, P. et al. A tailored approach to abdominoperineal resection for rectal cancer: multicentre analysis of short-term outcomes and impact on oncological survival. Langenbecks Arch Surg 406, 813–819 (2021). https://doi.org/10.1007/s00423-021-02122-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02122-y