Abstract
Purpose
Minimally invasive esophagectomy (MIE) has been increasingly used, but many reports have stated that recurrent laryngeal nerve (RLN) palsy after MIE is a major complication associated with postoperative pneumonia. Prevention of RLN palsy clearly has been a challenging task. The study aim was to determine if a three-dimensional (3-D) stereoscopic vision system can reduce the RLN palsy rate after MIE.
Methods
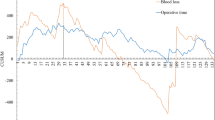
This was a retrospective study of MIE (McKeown esophagectomy) using a 3-D or 2-D stereoscopic vision system to treat 358 patients in the prone position between April 2010 and March 2019. The patients who underwent 3-D MIE (3-D group) or 2-D MIE (2-D group) were matched by using propensity score matching. After matching, the perioperative outcomes were compared between the groups.
Results
After propensity score matching, 154 patients were analyzed (77 patients, 3-D group; 77 patients, 2-D group). There were no significant differences in the patients’ baseline characteristics in the matched cohort. There were no significant differences in the rates of pneumonia (Clavien–Dindo (C–D) grade ≥ II, 3-D vs. 2-D, 11 (14%) vs. 12 (16%)), anastomotic leakage (C–D grade ≥ II, 10 (13%) vs. 18 (23%)) and mortality. The rates of left RLN palsy (C–D grade ≥ IIIa, 1 (1.3%) vs. 7 (9.1%), P = 0.029), right RLN palsy (C–D grade ≥ I, 2 (3%) vs. 8 (10%), P = 0.049), comprehensive complication index (CCI®) (8.5 vs. 14.3, P = 0.011), and postoperative hospital stay period (median: 25 vs. 30 days, P = 0.034) were significantly lower in the 3-D group than in the 2-D group, respectively.
Conclusions
In MIE, the 3-D viewing system was one of the factors that reduced postoperative morbidities such as the rates of each RLN palsy and CCI®, leading to shorter postoperative hospital stay.



Similar content being viewed by others
Data availability
The datasets generated during and analyzed during the current study are not publicly available due to medical data included participants’ personal data.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Watson A (1994) Operable esophageal cancer: current results from the West. World J Surg 18:361–366
Cuschieri A, Shimi S, Banting S (1992) Endoscopic oesophagectomy through a right thoracoscopic approach. J R Coll Surg Edinb 37:7–11
Oshikiri T, Takiguchi G, Hasegawa H, Yamamoto M, Kanaji S, Yamashita K, Matsuda T, Nakamura T, Suzuki S, Kakeji Y (2020) Postoperative recurrent laryngeal nerve palsy is associated with pneumonia in minimally invasive esophagectomy for esophageal cancer. Surg Endosc. https://doi.org/10.1007/s00464-020-07455-1
Liu J, Zhou H, Qin H, Ru H, Huang J, Liang S, Mo X, Tang W (2018) Comparative study of clinical efficacy using three dimensional and two-dimensional laparoscopies in the treatment of distal gastric cancer. Onco Targets Ther. Volume 11:301–306. https://doi.org/10.2147/OTT.S153520
Kanaji S, Suzuki S, Harada H, Nishi M, Yamamoto M, Matsuda T, Oshikiri T, Nakamura T, Fujino Y, Tominaga M, Kakeji Y (2017) Comparison of two- and three-dimensional display for performance of laparoscopic total gastrectomy for gastric cancer. Langenbecks Arch Surg 402(3):493–500
McKeown KC (1976) Total three-stage oesophagectomy for cancer of the oesophagus. Br J Surg 63:259–262
Rice TW, Blackstone EH, Rusch VW (2010) 7th edition of the AJCC Cancer Staging Manual: esophagus and esophagogastric junction. Ann Surg Oncol 17:1721–1724
Mori T, Kimura T, Kitajima M (2010) Skill accreditation system for laparoscopic gastroenterologic surgeons in Japan. Minim Invasive Ther Allied Technol 19:18–23
van Workum F, Fransen L, Luyer MD, Rosman C (2018) Learning curves in minimally invasive esophagectomy. World J Gastroenterol. 24(44):4974–4978
van Workum F, Stenstra MHBC, Berkelmans GHK, Slaman AE, van Berge Henegouwen MI, Gisbertz SS, van den Wildenberg FJH, Polat F, Irino T, Nilsson M, Nieuwenhuijzen GAP, Luyer MD, Adang EM, Hannink G, Rovers MM, Rosman C (2019) Learning curve and associated morbidity of minimally invasive esophagectomy: a retrospective multicenter study. Ann Surg. 269(1):88–94
Oshikiri T, Yasuda T, Harada H, Goto H, Oyama M, Hasegawa H, Ohara T, Sendo T, Nakamura T, Fujino Y, Tominaga M, Kakeji Y (2015) A new method (the “Bascule method”) for lymphadenectomy along the left recurrent laryngeal nerve during prone esophagectomy for esophageal cancer. Surg Endosc 29:2442–2450
Oshikiri T, Nakamura T, Hasegawa H, Yamamoto M, Kanaji S, Yamashita K, Matsuda T, Sumi Y, Fujino Y, Tominaga M, Suzuki S, Kakeji Y (2018) Standardizing procedures improves and homogenizes short-term outcomes after minimally invasive esophagectomy. Langenbecks Arch Surg 403:221–234
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258:1–7
Clavien PA, Vetter D, Staiger RD, Slankamenac K, Mehra T, Graf R, Puhan MA (2017) The Comprehensive Complication Index (CCI®): added value and clinical perspectives 3 years “Down the Line”. Ann Surg 265:1045–1050
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55
Choi DH, Jeong WK, Lim SW, Chung TS, Park JI, Lim SB, Choi HS, Nam BH, Chang HJ, Jeong SY (2009) Learning curves for laparoscopic sigmoidectomy used to manage curable sigmoid colon cancer: single-institute, three-surgeon experience. Surg Endosc 23:622628
Oshikiri T, Yasuda T, Yamamoto M, Kanaji S, Yamashita K, Matsuda T, Sumi Y, Nakamura T, Fujino Y, Tominaga M, Suzuki S, Kakeji Y (2016) Trainee competence in thoracoscopic esophagectomy in the prone position: evaluation using cumulative sum techniques. Langenbecks Arch Surg 401:797–804
Arezzo A, Vettoretto N, Francis NK, Bonino MA, Curtis NJ, Amparore D, Arolfo S, Barberio M, Boni L, Brodie R, Bouvy N, Cassinotti E, Carus T, Checcucci E, Custers P, Diana M, Jansen M, Jaspers J, Marom G, Momose K, Müller-Stich BP, Nakajima K, Nickel F, Perretta S, Porpiglia F, Sánchez-Margallo F, Sánchez-Margallo JA, Schijven M, Silecchia G, Passera R, Mintz Y (2019) The use of 3D laparoscopic imaging systems in surgery: EAES consensus development conference 2018. Surg Endosc 33:3251–3274
Yazawa H, Takiguchi K, Imaizumi K, Wada M, Ito F (2018) Surgical outcomes of total laparoscopic hysterectomy with 2-dimensional versus 3-dimensional laparoscopic surgical systems. Fukushima J Med Sci 64:38–45
Charalabopoulos A, Lorenzi B, Kordzadeh A, Tang CB, Kadirkamanathan S, Jayanthi NV (2017) Role of 3D in minimally invasive esophagectomy. Langenbecks Arch Surg 402:555–561
Cuesta MA, van der Wielen N, Weijs TJ, Bleys RL, Gisbertz SS, van Duijvendijk P, van Hillegersberg R, Ruurda JP, van Berge Henegouwen MI, Straatman J, Osugi H, van der Peet DL (2017) Surgical anatomy of the supracarinal esophagus based on a minimally invasive approach: vascular and nervous anatomy and technical steps to resection and lymphadenectomy. Surg Endosc 31:1863–1870
Otsuka K, Murakami M, Goto S, Ariyoshi T, Yamashita T, Saito A, Kohmoto M, Kato R, Lefor AK, Aoki T (2020) Minimally invasive esophagectomy and radical lymph node dissection without recurrent laryngeal nerve paralysis. Surg Endos. 34:2749–2757. https://doi.org/10.1007/s00464-020-07372-3
Nishi M, Kanaji S, Otake Y, Harada H, Yamamoto M, Oshikiri T, Nakamura T, Suzuki S, Suzuki Y, Hiasa Y, Sato Y, Kakeji Y (2017) Quantitative comparison of operative skill using 2-and 3-dimensional monitors during laparoscopic phantom tasks. Surgery 161:1334–1340
Harada H, Kanaji S, Hasegawa H, Yamamoto M, Matsuda Y, Yamashita K, Matsuda T, Oshikiri T, Sumi Y, Nakamura T, Suzuki S, Kakeji Y (2018) The effect on surgical skills of expert surgeons using 3D/HD and 2D/4K resolution monitors in laparoscopic phantom tasks. Surg Endosc 32:4228–4234
Harada H, Kanaji S, Nishi M, Otake Y, Hasegawa H, Yamamoto M, Matsuda Y, Yamashita K, Matsuda T, Oshikiri T, Sumi Y, Nakamura T, Suzuki S, Sato Y, Kakeji Y (2018) The learning effect of using stereoscopic vision in the early phase of laparoscopic surgical training for novices. Surg Endosc 32:582–588
Whitman R (1970) Stereopsis and stereoblindness. Exp Brain Res 10:380–388
Taffinder N, Smith SG, Huber J, Russell RC, Darzi A (1999) The effect of a second-generation 3D endoscope on the laparoscopic precision of novices and experienced surgeons. Surg Endosc 13:1087–1092
Fergo C, Burcharth J, Pommergaard HC, Rosenberg J (2016) Age is highly associated with stereo blindness among surgeons: a cross-sectional study. Surg Endosc 30:4889–4894
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Takuya Kudo and Oshikiri Taro. The first draft of the manuscript was written by Takuya Kudo and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Approval was obtained from the ethics committee of Kobe University. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kudo, T., Oshikiri, T., Takiguchi, G. et al. Three-dimensional visualization system is one of the factors that improve short-term outcomes after minimally invasive esophagectomy. Langenbecks Arch Surg 406, 631–639 (2021). https://doi.org/10.1007/s00423-020-02028-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-02028-1