Abstract
Purpose
Increased model for end-stage liver disease (MELD) score measured in the early postoperative course is associated with one-year mortality and graft loss. However, the correlation with postoperative complications has not been investigated. The aim of this study was to investigate the association between postoperative MELD score and subsequent complications.
Methods
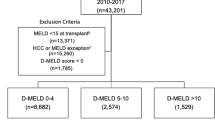
Adult liver transplant recipients transplanted from January 2011 until December 2016 were included. MELD score days 1–5 were correlated with complications day 6–30, subdivided into type and severity according to Clavien-Dindo classification.
Results
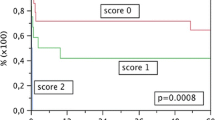
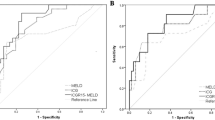
We included 246 adult liver transplant recipients. Between days 6 and 30, 671 complications occurred in 201 of the patients (82%) corresponding to 64% of all postoperative complications in the whole postoperative period (days 0–30). In multivariate analyses adjusted for recipient gender and age, preoperative MELD score, and Eurotransplant Donor Risk Index, postoperative MELD score was significantly associated with having one or more complications, any type of complication except cardiovascular and renal complications, and complication severity.
Conclusions
Postoperative MELD score days 1–5 were associated with complications arising in the subsequent period 6–30 days after transplantation. An increased MELD score should heighten the clinician’s awareness of a possible complication.



Similar content being viewed by others
Data Availability
Data available upon request.
References
Daugaard TR, Pommergaard HC, Rostved AA, Rasmussen A (2018) Postoperative complications as a predictor for survival after liver transplantation—proposition of a prognostic score. HPB 20(9):815–822. https://doi.org/10.1016/j.hpb.2018.03.001
Chawla YK, Kashinath RC, Duseja A, Dhiman RK (2011) Predicting mortality across a broad spectrum of liver disease—an assessment of model for end-stage liver disease (MELD), Child-Turcotte-Pugh (CTP), and creatinine-modified CTP scores. J Clin Exp Hepatol 1(3):161–168. https://doi.org/10.1016/s0973-6883(11)60233-8
Elwir S, Lake J (2016) Current status of liver allocation in the United States. Gastroenterol Hepatol 12(3):166–170
Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, Kremers W, Lake J, Howard T, Merion RM, Wolfe RA, Krom R (2003) Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 124(1):91–96. https://doi.org/10.1053/gast.2003.50016
Habib S, Berk B, Chang CC, Demetris AJ, Fontes P, Dvorchik I, Eghtesad B, Marcos A, Shakil AO (2006) MELD and prediction of post-liver transplantation survival. Liver Transpl 12(3):440–447. https://doi.org/10.1002/lt.20721
Jacob M, Copley LP, Lewsey JD, Gimson A, Toogood GJ, Rela M, van der Meulen JH (2004) Pretransplant MELD score and post liver transplantation survival in the UK and Ireland. Liver Transpl 10(7):903–907. https://doi.org/10.1002/lt.20169
Nagler E, Van Vlierberghe H, Colle I, Troisi R, de Hemptinne B (2005) Impact of MELD on short-term and long-term outcome following liver transplantation: a European perspective. Eur J Gastroenterol Hepatol 17(8):849–856
Wong CS, Lee WC, Jenq CC, Tian YC, Chang MY, Lin CY, Fang JT, Yang CW, Tsai MH, Shih HC, Chen YC (2010) Scoring short-term mortality after liver transplantation. Liver Transpl 16(2):138–146. https://doi.org/10.1002/lt.21969
Wagener G, Raffel B, Young AT, Minhaz M, Emond J (2013) Predicting early allograft failure and mortality after liver transplantation: the role of the postoperative model for end-stage liver disease score. Liver Transpl 19(5):534–542. https://doi.org/10.1002/lt.23634
Khandoga A, Iskandarov E, Angele M, Gerbes A, Frey L, Agayev B, Jauch KW, Werner J, Guba M (2016) Model for end-stage liver disease score in the first 3 weeks after liver transplantation as a predictor for long-term outcome. Eur J Gastroenterol Hepatol 28(2):153–158. https://doi.org/10.1097/MEG.0000000000000505
Kim JD, Choi JY, Kwon JH, Jang JW, Bae SH, Yoon SK, You YK, Kim DG (2009) Performance of posttransplant Model for End-Stage Liver Disease (MELD) and delta-MELD scores on short-term outcome after living donor liver transplantation. Transplant Proc 41(9):3766–3768. https://doi.org/10.1016/j.transproceed.2009.10.006
Rostved AA, Lundgren JD, Hillingso J, Peters L, Mocroft A, Rasmussen A (2016) MELD score measured day 10 after orthotopic liver transplantation predicts death and re-transplantation within the first year. Scand J Gastroenterol 51(11):1360–1366. https://doi.org/10.1080/00365521.2016.1196497
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335(7624):806–808. https://doi.org/10.1136/bmj.39335.541782.AD
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Braat AE, Blok JJ, Putter H, Adam R, Burroughs AK, Rahmel AO, Porte RJ, Rogiers X, Ringers J, European L, Intestine Transplant A, Eurotransplant Liver Intestine Advisory C (2012) The Eurotransplant donor risk index in liver transplantation: ET-DRI. Am J Transplant 12(10):2789–2796. https://doi.org/10.1111/j.1600-6143.2012.04195.x
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Matthews JN, Altman DG, Campbell MJ, Royston P (1990) Analysis of serial measurements in medical research. BMJ 300(6719):230–235
Saab S, Wang V, Ibrahim AB, Durazo F, Han S, Farmer DG, Yersiz H, Morrisey M, Goldstein LI, Ghobrial RM, Busuttil RW (2003) MELD score predicts 1-year patient survival post-orthotopic liver transplantation. Liver Transpl 9(5):473–476. https://doi.org/10.1053/jlts.2003.50090
Desai NM, Mange KC, Crawford MD, Abt PL, Frank AM, Markmann JW, Velidedeoglu E, Chapman WC, Markmann JF (2004) Predicting outcome after liver transplantation: utility of the model for end-stage liver disease and a newly derived discrimination function. Transplantation 77(1):99–106. https://doi.org/10.1097/01.TP.0000101009.91516.FC
Fosby B, Melum E, Bjoro K, Bennet W, Rasmussen A, Andersen IM, Castedal M, Olausson M, Wibeck C, Gotlieb M, Gjertsen H, Toivonen L, Foss S, Makisalo H, Nordin A, Sanengen T, Bergquist A, Larsson ME, Soderdahl G, Nowak G, Boberg KM, Isoniemi H, Keiding S, Foss A, Line PD, Friman S, Schrumpf E, Ericzon BG, Hockerstedt K, Karlsen TH (2015) Liver transplantation in the Nordic countries—an intention to treat and post-transplant analysis from The Nordic Liver Transplant Registry 1982-2013. Scand J Gastroenterol 50(6):797–808. https://doi.org/10.3109/00365521.2015.1036359
Adam R, Karam V, Delvart V, O'Grady J, Mirza D, Klempnauer J, Castaing D, Neuhaus P, Jamieson N, Salizzoni M, Pollard S, Lerut J, Paul A, Garcia-Valdecasas JC, Rodriguez FS, Burroughs A, All contributing c, European L, Intestine Transplant A (2012) Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol 57(3):675–688. https://doi.org/10.1016/j.jhep.2012.04.015
Olthoff KM, Kulik L, Samstein B, Kaminski M, Abecassis M, Emond J, Shaked A, Christie JD (2010) Validation of a current definition of early allograft dysfunction in liver transplant recipients and analysis of risk factors. Liver Transpl 16(8):943–949. https://doi.org/10.1002/lt.22091
Bolondi G, Mocchegiani F, Montalti R, Nicolini D, Vivarelli M, De Pietri L (2016) Predictive factors of short term outcome after liver transplantation: a review. World J Gastroenterol 22(26):5936–5949. https://doi.org/10.3748/wjg.v22.i26.5936
Xu X, Ling Q, Wu J, Chen J, Gao F, Feng XN, Zheng SS (2007) A novel prognostic model based on serum levels of total bilirubin and creatinine early after liver transplantation. Liver Int 27(6):816–824. https://doi.org/10.1111/j.1478-3231.2007.01494.x
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Hans-Christian Pommergaard contributed in the conception and design, data analysis and interpretation of results, writing the first draft, critical revision, and final approval. Thomas Røjkjær Daugaard contributed in the conception and design, interpretation of results, critical revision, and final approval. Andreas Arendtsen Rostved contributed in the conception and design, interpretation of results, critical revision, and final approval. Nicolai Aagaard Schultz contributed in the interpretation of results, critical revision, and final approval. Jens Hillingsø contributed in the interpretation of results, critical revision, and final approval. Paul Suno Krohn contributed in the interpretation of results, critical revision, and final approval. Allan Rasmussen contributed in the conception and design, interpretation of results, acquisition of data, critical revision, and final approval.
Corresponding author
Ethics declarations
Conflicts of interest
There were no conflicts of interest for any of the authors.
Ethical approval
The study was approved by the Danish Data Protection Agency (2012-58-0004) and the Danish Patient Safety Authority (3-3013-1948-1).
Consent to participate
Not applicable.
Consent for publication
All authors fulfill the four criteria for authorship of the ICMJE.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pommergaard, HC., Daugaard, T.R., Rostved, A.A. et al. Model for end-stage liver disease score predicts complications after liver transplantation. Langenbecks Arch Surg 406, 55–65 (2021). https://doi.org/10.1007/s00423-020-02018-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-02018-3