Abstract
Purpose
Proper transection of the distal rectum is important for reconstruction of bowel continuity in rectal cancer surgery. In this study, we introduced a modified technique for ligation of the distal rectum, and investigated its safety and efficiency to facilitate the rectum transection.
Methods
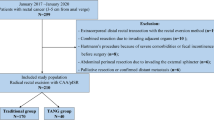
After complete mobilization and transection of the mesorectum, a cable tie was carefully positioned distal to the tumor, followed by washout and transecting the rectum with a linear stapler. From September 2017 to June 2018, consecutive 67 mid-low rectal cancer patients with laparoscopic anterior resection underwent this technique. Clinical data of these patients, including number of firings, pathological and operative variables, and postoperative outcomes, were compared with those of 132 consecutive patients who underwent traditional surgery from January 2016 to August 2017.
Results
Compared with the traditional method, cable tie ligation significantly reduced the number of firings (1.1 ± 0.32 vs. 1.3 ± 0.52, p < 0.001). A very high ratio of one firing transection of rectum was observed in the cable tie group (94.0% vs. 68.9%, p < 0.001), even in patients with tumor at or below the peritoneal reflection (90.2% vs. 54.4%, p < 0.001), in male patients (95.5% vs. 65.8%, p < 0.001), and in obese patients (93.8% vs. 64.9%, p = 0.005). The mean distal margin was longer in the cable tie group (3.19 ± 1.77 cm vs. 2.54 ± 1.36 cm, p = 0.005), with no positive distal margin observed. The operation time, quality of mesorectum, and morbidity between two groups were comparable. Two leaks (3.0%) in the cable tie group were observed, similar to 3.8% in the control.
Conclusions
Ligation of the rectum with a cable tie reduces the number of cartridges, and increases the rate of one stapler firing for rectal transection, even in those difficult cases like male, overweight, and low rectal cancer patients. It is also useful for occlusion of the rectum before washout. It is safe, feasible, and worthwhile for popularization.
Trial registration
Registered at ClinicalTrial.gov, number NCT03570684




Similar content being viewed by others
References
Martinez-Perez A, Carra MC, Brunetti F, de’ Angelis N (2017) Pathologic outcomes of laparoscopic vs open mesorectal excision for rectal cancer: a systematic review and meta-analysis. JAMA Surg 152 (4):e165665. doi:https://doi.org/10.1001/jamasurg.2016.5665
Hida K, Okamura R, Sakai Y, Konishi T, Akagi T, Yamaguchi T, Akiyoshi T, Fukuda M, Yamamoto S, Yamamoto M, Nishigori T, Kawada K, Hasegawa S, Morita S, Watanabe M, Japan Society of Laparoscopic Colorectal S (2017) Open versus laparoscopic surgery for advanced low rectal cancer: a large, multicenter, propensity score matched cohort study in Japan. Ann Surg. https://doi.org/10.1097/SLA.0000000000002329
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Davies L, Wilson K, Hague W, Simes J, Investigators AL (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314(13):1356–1363. https://doi.org/10.1001/jama.2015.12009
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, Peters WR Jr, Maun D, Chang G, Herline A, Fichera A, Mutch M, Wexner S, Whiteford M, Marks J, Birnbaum E, Margolin D, Larson D, Marcello P, Posner M, Read T, Monson J, Wren SM, Pisters PW, Nelson H (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314(13):1346–1355. https://doi.org/10.1001/jama.2015.10529
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, Lacy AM, Bemelman WA, Andersson J, Angenete E, Rosenberg J, Fuerst A, Haglind E, Group CIS (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372 (14):1324–1332. doi:https://doi.org/10.1056/NEJMoa1414882
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, Choi HS, Kim DW, Chang HJ, Kim DY, Jung KH, Kim TY, Kang GH, Chie EK, Kim SY, Sohn DK, Kim DH, Kim JS, Lee HS, Kim JH, Oh JH (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15(7):767–774. https://doi.org/10.1016/S1470-2045(14)70205-0
van der Pas MHGM, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WCJ, Bonjer HJ (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14(3):210–218. https://doi.org/10.1016/s1470-2045(13)70016-0
Park SJ, Choi SI, Lee SH, Lee KY (2010) Endo-Satinsky clamp for rectal transection during laparoscopic total mesorectal excision. Dis Colon Rectum 53(3):355–359. https://doi.org/10.1007/DCR.0b013e3181c388e9
Kuroyanagi H, Oya M, Ueno M, Fujimoto Y, Yamaguchi T, Muto T (2008) Standardized technique of laparoscopic intracorporeal rectal transection and anastomosis for low anterior resection. Surg Endosc 22(2):557–561. https://doi.org/10.1007/s00464-007-9626-9
Park JS, Choi GS, Kim SH, Kim HR, Kim NK, Lee KY, Kang SB, Kim JY, Lee KY, Kim BC, Bae BN, Son GM, Lee SI, Kang H (2013) Multicenter analysis of risk factors for anastomotic leakage after laparoscopic rectal cancer excision: the Korean laparoscopic colorectal surgery study group. Ann Surg 257(4):665–671. https://doi.org/10.1097/SLA.0b013e31827b8ed9
Kim JS, Cho SY, Min BS, Kim NK (2009) Risk factors for anastomotic leakage after laparoscopic intracorporeal colorectal anastomosis with a double stapling technique. J Am Coll Surg 209(6):694–701. https://doi.org/10.1016/j.jamcollsurg.2009.09.021
Kawada K, Hasegawa S, Hida K, Hirai K, Okoshi K, Nomura A, Kawamura J, Nagayama S, Sakai Y (2014) Risk factors for anastomotic leakage after laparoscopic low anterior resection with DST anastomosis. Surg Endosc 28(10):2988–2995. https://doi.org/10.1007/s00464-014-3564-0
Qu H, Liu Y, Bi DS (2015) Clinical risk factors for anastomotic leakage after laparoscopic anterior resection for rectal cancer: a systematic review and meta-analysis. Surg Endosc 29(12):3608–3617. https://doi.org/10.1007/s00464-015-4117-x
Salerno G, Sinnatamby C, Branagan G, Daniels IR, Heald RJ, Moran BJ (2006) Defining the rectum: surgically, radiologically and anatomically. Color Dis 8(Suppl 3):5–9. https://doi.org/10.1111/j.1463-1318.2006.01062.x
Wu QB, Deng XB, Zhang XB, Kong LH, Zhou ZG, Wang ZQ (2018) Short-term and long-term outcomes of laparoscopic versus open surgery for low rectal cancer. J Laparoendosc Adv Surg Tech A 28(6):637–644. https://doi.org/10.1089/lap.2017.0630
Watanabe J, Ota M, Suwa Y, Ishibe A, Masui H, Nagahori K (2016) Single-incision laparoscopic anterior resection using a curved stapler. Dis Colon Rectum 59(11):1105–1109. https://doi.org/10.1097/dcr.0000000000000687
Alevizos L, Lirici MM (2012) Laparoscopic intracorporeal distal rectal transection with the CONTOUR((R)) device. Tech Coloproctol 16(5):379–383. https://doi.org/10.1007/s10151-012-0818-5
Bulut O (2013) Ligation of the rectum with an extracorporeal sliding knot facilitating laparoscopic cross-stapling: a procedure revisited. J Laparoendosc Adv Surg Tech A 23(11):938–941. https://doi.org/10.1089/lap.2013.0064
Furuhata T, Hata F, Tsuruma T, Nishimori H, Yamaguchi K, Mizuguchi T, Kimura Y, Katsuramaki T, Mukaiya M, Sasaki K, Hirata K (2004) Endo-bowel clamp (PL540S) for safe rectal irrigation in laparoscopy-assisted rectal resection. Surg Today 34(10):882–884. https://doi.org/10.1007/s00595-004-2838-x
Hotta T, Takifuji K, Yokoyama S, Matsuda K, Yamaue H (2012) Rectal transection using a curved cutter stapler with an endo-Satinsky clamp during a laparoscopic low anterior resection. Langenbeck's Arch Surg 397(7):1149–1155. https://doi.org/10.1007/s00423-012-0955-3
Simillis C, Mistry K, Prabhudesai A (2013) Intraoperative rectal washout in rectal cancer surgery: a survey of current practice in the UK. Int J Surg 11(9):993–997. https://doi.org/10.1016/j.ijsu.2013.06.002
Rondelli F, Trastulli S, Cirocchi R, Avenia N, Mariani E, Sciannameo F, Noya G (2012) Rectal washout and local recurrence in rectal resection for cancer: a meta-analysis. Color Dis 14(11):1313–1321. https://doi.org/10.1111/j.1463-1318.2011.02903.x
Moran B, Cunningham C, Singh T, Sagar P, Bradbury J, Geh I, Karandikar S (2017) Association of Coloproctology of Great Britain & Ireland (ACPGBI): guidelines for the management of cancer of the colon, rectum and anus (2017) - surgical management. Color Dis 19(Suppl 1):18–36. https://doi.org/10.1111/codi.13704
Lohsiriwat V, Lohsiriwat D, Thavichaigarn P (2009) Current practices in rectal cancer surgery: a survey of Thai colorectal surgeons. J Med Assoc Thail 92(8):1009–1015
Heald RJ (2012) Rectal cancer in the 21St century—radical operations: anterior resection and abdominoperineal excision. In: Fischer JE (ed) Fischer’s mastery of surgery, 6th edn. Williams & Wilkins, Lippincott, pp 1714–1731
Thomas WM, Hewett PJ (1996) A novel method of rectal occlusion during anterior resection of the rectum. Aust NZ J Surg 66(3):181–182. https://doi.org/10.1111/j.1445-2197.1996.tb01153.x
Funding
This study was funded by the Ministry of Science and Technology of the People’s Republic of China (grant No. 2017YFC0908200) and Scientific and Technology Department of Sichuan Province (grant No. 2018SZ0242).
Author information
Authors and Affiliations
Contributions
Minyang Ren and Ziqiang Wang contributed to the study conception and design; Xiangbing Deng, Liang Bi, Xuyang Yang, Mingtian Wei, and Qingbin Wu contributed to the acquisition of data, analysis, and interpretation of data for the submission; Xiangbing Deng drafted the submission; Xia Meng made the video; Liang Bi, Xiangbing Deng, Xia Meng, and Ziqiang Wang revised the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consents were obtained from all individual participants whom receive the cable tie procedure; for the patients with grasping forceps, as a retrospective control group and common practice, the informed consents were not obtained.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Bi, L., Deng, X., Meng, X. et al. Ligating the rectum with cable tie facilitates rectum transection in laparoscopic anterior resection of rectal cancer. Langenbecks Arch Surg 405, 233–239 (2020). https://doi.org/10.1007/s00423-020-01863-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01863-6