Abstract
Background
Central pancreatectomy (CP) is the alternative to distal pancreatectomy (DP) for specific pathologies of the mid-pancreas. However, the benefits of CP over DP remain controversial. This study aims to compare the two procedures by conducting a meta-analysis of all published papers.
Methods
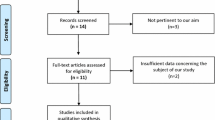
A systematic search of original studies comparing CP vs. DP was performed using PubMed, Scopus, and Cochrane Library databases up to June 2018. The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) checklist was followed.
Results
Twenty-one studies were included (596 patients with CP and 1070 patients with DP). Compared to DP, CP was associated with significantly higher rates of overall and severe morbidity (p < 0.0001), overall and clinically relevant pancreatic fistula (p < 0.0001), postoperative hemorrhage (p = 0.02), but with significantly lower incidences of new-onset (p < 0.0001) and worsening diabetes mellitus (p = 0.004). Furthermore, significantly longer length of hospital stay (p < 0.0001) was observed for CP patients.
Conclusions
CP is superior to DP regarding the preservation of pancreatic functions, but at the expense of significantly higher complication rates and longer hospital stay. Proper selection of patients is of utmost importance to maximize the benefits and mitigate the risks of CP.




Similar content being viewed by others
References
Iacono C, Bortolasi L, Facci E, Nifosi F, Pachera S, Ruzzenente A, Guglielmi A (2007) The Dagradi-Serio-Iacono operation central pancreatectomy. J Gastrointest Surg 11:364–376
Beger HG, Poch B, Vasilescu C (2014) Benign cystic neoplasm and endocrine tumours of the pancreas--when and how to operate--an overview. Int J Surg 12:606–614
Iacono C, Verlato G, Ruzzenente A, Campagnaro T, Bacchelli C, Valdegamberi A, Bortolasi L, Guglielmi A (2013) Systematic review of central pancreatectomy and meta-analysis of central versus distal pancreatectomy. Br J Surg 100:873–885
Xiao W, Zhu J, Peng L, Hong L, Sun G, Li Y (2018) The role of central pancreatectomy in pancreatic surgery: a systematic review and meta-analysis. HPB (Oxford) 20:896–904
Xu SB, Zhu YP, Zhou W, Xie K, Mou YP (2013) Patients get more long-term benefit from central pancreatectomy than distal resection: a meta-analysis. Eur J Surg Oncol 39:567–574
Dumitrascu T, Scarlat A, Ionescu M, Popescu I (2017) Central pancreatectomy: an oncologically safe option to treat metastases of other neoplasms of the mid-portion of the pancreas? Ann Hepatobiliary Pancreat Surg 21:76–79
Gao H, Liu T, Wang G, Gao Y, Yin L, Peng Y, Lyu N, Zhang K, Gao W, Wu J, Jiang K, Wei J, Miao Y (2019) Central pancreatectomy for early-stage pancreatic ductal adenocarcinoma: a single-center case-control study. Langenbeck's Arch Surg 404:175–182
Crippa S, Bassi C, Warshaw AL, Falconi M, Partelli S, Thayer SP, Pederzoli P, Fernandez-del Castillo C (2007) Middle pancreatectomy: indications, short- and long-term operative outcomes. Ann Surg 246:69–76
Goudard Y, Gaujoux S, Dokmak S, Cros J, Couvelard A, Palazzo M, Ronot M, Vullierme MP, Ruszniewski P, Belghiti J, Sauvanet A (2014) Reappraisal of central pancreatectomy a 12-year single-center experience. JAMA Surg 149:356–363
Paiella S, De Pastena M, Faustini F, Landoni L, Pollini T, Bonamini D, Giuliani T, Bassi C, Esposito A, Tuveri M, Salvia R (2019) Central pancreatectomy for benign or low-grade malignant pancreatic lesions - a single-center retrospective analysis of 116 cases. Eur J Surg Oncol 45:788–792
Lv A, Qian HG, Qiu H, Wu JH, Hao CY (2018) Is central pancreatectomy truly recommendable? A 9-year single-center experience. Dig Surg 35:532–538
Dokmak S, Fteriche FS, Aussilhou B, Levy P, Ruszniewski P, Cros J, Vullierme MP, Khoy EL, Belghiti J, Sauvanet A (2017) The largest European single-center experience: 300 laparoscopic pancreatic resections. J Am Coll Surg 225:226–234
Du ZY, Chen S, Han BS, Shen BY, Liu YB, Peng CH (2013) Middle segmental pancreatectomy: a safe and organ-preserving option for benign and low-grade malignant lesions. World J Gastroenterol 19:1458–1465
Dumitrascu T, Scarlat A, Ionescu M, Popescu I (2012) Central pancreatectomy versus spleen-preserving distal pancreatectomy: a comparative analysis of early and late postoperative outcomes. Dig Surg 29:400–407
Mise Y, Tanaka N, Furuya T, Nomura Y, Nagai M, Yoshida Y, Ishii H, Seo A (2014) The feasibility of central pancreatectomy for blunt pancreatic trauma: a comparative study of central and distal pancreatectomy. Hepatogastroenterology 61:1107–1112
Song KB, Kim SC, Park KM, Hwang DW, Lee JH, Lee DJ, Lee JW, Jun ES, Shin SH, Kim HE, Lee YJ (2015) Laparoscopic central pancreatectomy for benign or low-grade malignant lesions in the pancreatic neck and proximal body. Surg Endosc 29:937–946
Xiang GM, Tan CL, Zhang H, Ran X, Mai G, Liu XB (2012) Central pancreatectomy for benign or borderline lesions of the pancreatic neck: a single centre experience and literature review. Hepatogastroenterology 59:1286–1289
Chen S, Zhan Q, Jin JB, Wu ZC, Shi Y, Cheng DF, Chen H, Deng XX, Shen BY, Peng CH, Li HW (2017) Robot-assisted laparoscopic versus open middle pancreatectomy: short-term results of a randomized controlled trial. Surg Endosc 31:962–971
Kang CM, Lee JH, Lee WJ (2014) Minimally invasive central pancreatectomy: current status and future directions. J Hepatobiliary Pancreat Sci 21:831–840
Zhang RC, Zhang B, Mou YP, Xu XW, Zhou YC, Huang CJ, Zhou JY, Jin WW, Lu C (2017) Comparison of clinical outcomes and quality of life between laparoscopic and open central pancreatectomy with pancreaticojejunostomy. Surg Endosc 31:4756–4763
Falconi M, Mantovani W, Frigerio I, Mascetta G, Sargenti M, Tardivo S, Salvia R, Bassi C, Pederzoli P (2001) Intermediate resection and distal pancreatectomy for benign neoplasms of the pancreas: comparison of postoperative complications and costs. Chir Ital 53:467–474
Pratt W, Maithel SK, Vanounou T, Callery MP, Vollmer CM Jr (2006) Postoperative pancreatic fistulas are not equivalent after proximal, distal, and central pancreatectomy. J Gastrointest Surg 10:1264–1278
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Cook DA, Reed DA (2015) Appraising the quality of medical education research methods: the medical education research study quality instrument and the Newcastle-Ottawa scale-education. Acad Med 90:1067–1076
Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hrobjartsson A, Kirkham J, Juni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schunemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Balzano G, Zerbi A, Veronesi P, Cristallo M, Di Carlo V (2003) Surgical treatment of benign and borderline neoplasms of the pancreatic body. Dig Surg 20:506–510
Cataldegirmen G, Schneider CG, Bogoevski D, Koenig A, Kaifi JT, Bockhorn M, Deutsch LS, Vashist Y, Izbicki JR, Yekebas EF (2010) Extended central pancreatic resection as an alternative for extended left or extended right resection for appropriate pancreatic neoplasms. Surgery 147:331–338
DiNorcia J, Ahmed L, Lee MK, Reavey PL, Yakaitis EA, Lee JA, Schrope BA, Chabot JA, Allendorf JD (2010) Better preservation of endocrine function after central versus distal pancreatectomy for mid-gland lesions. Surgery 148:1247–1254
Hirono S, Tani M, Kawai M, Ina S, Nishioka R, Miyazawa M, Shimizu A, Uchiyama K, Yamaue H (2009) A central pancreatectomy for benign or low-grade malignant neoplasms. J Gastrointest Surg 13:1659–1665
Kang CM, Lee JM, Kim MW, Yoon DS, Park JS, Lee WJ (2011) Experiences in central pancreatectomy. Dig Surg 28:57–62
Lee SE, Jang JY, Hwang DW, Lee KU, Kim SW (2010) Clinical efficacy of organ-preserving pancreatectomy for benign or low-grade malignant potential lesion. J Korean Med Sci 25:97–103
Muller MW, Friess H, Kleeff J, Hinz U, Wente MN, Paramythiotis D, Berberat PO, Ceyhan GO, Buchler MW (2006) Middle segmental pancreatic resection: an option to treat benign pancreatic body lesions. Ann Surg 244:909–918
Ocuin LM, Sarmiento JM, Staley CA, Galloway JR, Johnson CD, Wood WC, Kooby DA (2008) Comparison of central and extended left pancreatectomy for lesions of the pancreatic neck. Ann Surg Oncol 15:2096–2103
Shibata S, Sato T, Andoh H, Yasui O, Yoshioka M, Kurokawa T, Watanabe G, Ise N, Kotanagi H, Asanuma Y, Koyama K (2004) Outcomes and indications of segmental pancreatectomy. Comparison with distal pancreatectomy. Dig Surg 21:48–53
Shikano T, Nakao A, Kodera Y, Yamada S, Fujii T, Sugimoto H, Kanazumi N, Nomoto S, Takeda S (2010) Middle pancreatectomy: safety and long-term results. Surgery 147:21–29
Su CH, Shyr YM, Lui WY, P'eng FK (2004) Surgical treatment for serous cystadenoma of pancreas--segmental pancreatectomy or conventional resection? Hepatogastroenterology 51:595–598
Yamaguchi K, Yokohata K, Ohkido M, Watanabe M, Ogawa Y, Chijiiwa K, Tanaka M (2000) Which is less invasive--distal pancreatectomy or segmental resection? Int Surg 85:297–302
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Buchler MW (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142:20–25
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Buchler MW (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142:761–768
Huttner FJ, Koessler-Ebs J, Hackert T, Ulrich A, Buchler MW, Diener MK (2015) Meta-analysis of surgical outcome after enucleation versus standard resection for pancreatic neoplasms. Br J Surg 102:1026–1036
Ratnayake CB, Biela C, Windsor JA, Pandanaboyana S (2019) Enucleation for branch duct intraductal papillary mucinous neoplasms: a systematic review and meta-analysis. HPB (Oxford) pii: S1365-182X(19)30536-2. https://doi.org/10.1016/j.hpb.2019.04.015
Zhou Y, Zhao M, Wu L, Ye F, Si X (2016) Short- and long-term outcomes after enucleation of pancreatic tumors: an evidence-based assessment. Pancreatology 16:1092–1098
Okano K, Murakami Y, Nakagawa N, Uemura K, Sudo T, Hashimoto Y, Kondo N, Takahashi S, Sueda T (2016) Remnant pancreatic parenchymal volume predicts postoperative pancreatic exocrine insufficiency after pancreatectomy. Surgery 159:885–892
Kusakabe J, Anderson B, Liu J, Williams GA, Chapman WC, Doyle MMB, Khan AS, Sanford DE, Hammill CW, Strasberg SM, Hawkins WG, Fields RC (2019) Long-term endocrine and exocrine insufficiency after pancreatectomy. J Gastrointest Surg 23:1604–1613
Atema JJ, Jilesen AP, Busch OR, van Gulik TM, Gouma DJ, Nieveen van Dijkum EJ: Pancreatic fistulae after pancreatic resections for neuroendocrine tumours compared with resections for other lesions. HPB (Oxford) 2015;17:38–45
Dumitrascu T, Eftimie M, Aiordachioae A, Stroescu C, Dima S, Ionescu M, Popescu I (2018) Male gender and increased body mass index independently predicts clinically relevant morbidity after spleen-preserving distal pancreatectomy. World J Gastrointest Surg 10:84–89
Ecker BL, McMillan MT, Allegrini V, Bassi C, Beane JD, Beckman RM, Behrman SW, Dickson EJ, Callery MP, Christein JD, Drebin JA, Hollis RH, House MG, Jamieson NB, Javed AA, Kent TS, Kluger MD, Kowalsky SJ, Maggino L, Malleo G, Valero V, III, Velu LKP, Watkins AA, Wolfgang CL, Zureikat AH, Vollmer CM, Jr.: Risk factors and mitigation strategies for pancreatic fistula after distal pancreatectomy: analysis of 2026 resections from the international, multi-institutional distal Pancreatectomy study group. Ann Surg 2019;269:143–149
Fingerhut A, Uranues S, Khatkov I, Boni L (2018) Laparoscopic distal pancreatectomy: better than open? Transl Gastroenterol Hepatol 3:49
Nakata K, Shikata S, Ohtsuka T, Ukai T, Miyasaka Y, Mori Y, Velasquez VVDM, Gotoh Y, Ban D, Nakamura Y, Nagakawa Y, Tanabe M, Sahara Y, Takaori K, Honda G, Misawa T, Kawai M, Yamaue H, Morikawa T, Kuroki T, Mou Y, Lee WJ, Shrikhande SV, Tang CN, Conrad C, Han HS, Chinnusamy P, Asbun HJ, Kooby DA, Wakabayashi G, Takada T, Yamamoto M, Nakamura M (2018) Minimally invasive preservation versus splenectomy during distal pancreatectomy: a systematic review and meta-analysis. J Hepatobiliary Pancreat Sci 25:476–488
Acknowledgments
The authors thank Mr. William Ruixian He for critically reading the manuscript.
Author information
Authors and Affiliations
Contributions
Study design: Traian Dumitrascu. Acquisition of data: Mihnea P. Dragomir, Alexandru A. Sabo, George E.D. Petrescu, Traian Dumitrascu. Analysis and interpretation of data: Mihnea P. Dragomir, Alexandru A. Sabo, George E.D. Petrescu, Yongfeng Li, Traian Dumitrascu. Drafting the manuscript: Mihnea P. Dragomir, Alexandru A. Sabo, George E.D. Petrescu, Traian Dumitrascu. Critical revision of the work for important intellectual content: Mihnea P. Dragomir, Alexandru A. Sabo, George E.D. Petrescu, Yongfeng Li, Traian Dumitrascu. Final approval of the version to be published: Mihnea P. Dragomir, Alexandru A. Sabo, George E.D. Petrescu, Yongfeng Li, Traian Dumitrascu. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: Mihnea P. Dragomir, Alexandru A. Sabo, George E.D. Petrescu, Yongfeng Li, Traian Dumitrascu.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 4020 kb)
Rights and permissions
About this article
Cite this article
Dragomir, M.P., Sabo, A.A., Petrescu, G.E.D. et al. Central pancreatectomy: a comprehensive, up-to-date meta-analysis. Langenbecks Arch Surg 404, 945–958 (2019). https://doi.org/10.1007/s00423-019-01829-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-019-01829-3