Abstract
Purpose
Perioperative management of oral anticoagulation (OAC) is a constant challenge in interventional and surgical procedures. When deciding to discontinue OAC, the risk of thromboembolic events must be balanced against the risk of bleeding during and after the planned procedure. These risks differ across patients and must be considered individually.
Methods
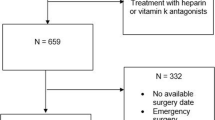
POPACTApp, an application for the perioperative or peri-interventional management of oral anticoagulants, was developed using a human-centered design process (ISO 9241-210:2010). The treatment concept developed here can be adapted to a patient’s individual risk profile. POPACTApp provides recommendations based on guidelines, consensus statements, and study data. After entering patient-specific risk factors, the attending physician using POPACTApp receives a clear and direct presentation of a periprocedural treatment concept, which should enable the efficient use of the program in everyday clinical practice. The perioperative treatment concept is presented via a timeline, including (1) the decision on whether to interrupt OAC, (2) the timing of the last preoperative administration of OAC in cases of interruption, (3) the decision on whether and how to bridge with heparins, and (4) the decision about when to reinitiate anticoagulation.
Results
A task-based survey to evaluate POPACTApp’s usability conducted with 20 surgeons showed that all clinicians correctly interpreted the recommendations provided by the app. Further, a questionnaire using a 7-point Likert scale from − 3 (negative) to + 3 (positive) revealed the following results to three specific questions: (1) satisfaction with the current standard procedure in the respective unit of the participant (0.15; SD = 1.57), (2) individual satisfaction with the POPACTApp application (2.7; SD = 0.47), and (3) estimation of the usefulness of POPACTApp for clinical practice (2.7; SD = 0.47).
Conclusions
POPACTApp provides clinicians with an individual risk-optimized treatment concept for the perioperative or peri-interventional management of OAC based on current guidelines, consensus statements, and study data, enabling the standardized perioperative handling of OAC in daily clinical practice.




Similar content being viewed by others
Abbreviations
- OAC :
-
Oral anticoagulation
- App :
-
Application
- AF :
-
Atrial fibrillation
- DOAC :
-
Direct-acting anticoagulant
- INR :
-
International normalized ratio
- LMWH :
-
Low molecular weight heparins
- POPACTApp :
-
Application for perioperative anticoagulant therapy
- MHV :
-
Mechanical heart valve
- Mobile app :
-
Application for mobile devices
- SD :
-
Standard deviation
- VTE :
-
Venous thromboembolism
References
Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, Seward JB, Tsang TS (2006) Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation 114(2):119–125. https://doi.org/10.1161/CIRCULATIONAHA.105.595140
Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, Dunn AS, Kunz R (2012) Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e326S–e350S. https://doi.org/10.1378/chest.11-2298
Spyropoulos AC, Douketis JD (2012) How I treat anticoagulated patients undergoing an elective procedure or surgery. Blood 120(15):2954–2962. https://doi.org/10.1182/blood-2012-06-415943
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, JH MA Jr, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA, Ezzati M, Murray CJ (2014) Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 129(8):837–847. https://doi.org/10.1161/CIRCULATIONAHA.113.005119
Gage BF, van Walraven C, Pearce L, Hart RG, Koudstaal PJ, Boode BS, Petersen P (2004) Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin. Circulation 110(16):2287–2292. https://doi.org/10.1161/01.CIR.0000145172.55640.93
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ (2001) Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 285(22):2864–2870
Olesen JB, Torp-Pedersen C, Hansen ML, Lip GY (2012) The value of the CHA2DS2-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS2 score 0-1: a nationwide cohort study. Thromb Haemost 107(6):1172–1179. https://doi.org/10.1160/TH12-03-0175
Olesen JB, Lip GY, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, Selmer C, Ahlehoff O, Olsen AM, Gislason GH, Torp-Pedersen C (2011) Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ 342:d124. https://doi.org/10.1136/bmj.d124
Omran H, Bauersachs R, Rubenacker S, Goss F, Hammerstingl C (2012) The HAS-BLED score predicts bleedings during bridging of chronic oral anticoagulation. Results from the national multicentre BNK Online bRiDging REgistRy (BORDER). Thromb Haemost 108(1):65–73. https://doi.org/10.1160/TH11-12-0827
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY (2010) A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 138(5):1093–1100. https://doi.org/10.1378/chest.10-0134
Tafur AJ, McBane R, 2nd, Wysokinski WE, Litin S, Daniels P, Slusser J, Hodge D, Beckman MG, Heit JA (2012) Predictors of major bleeding in peri-procedural anticoagulation management. J Thromb Haemost 10 (2):261–267. https://doi.org/10.1111/j.1538-7836.2011.04572.x
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW, American College of Cardiology/American Heart Association Task Force on Practice G (2014) 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 64 (21):e1–76. https://doi.org/10.1016/j.jacc.2014.03.022
Doherty JU, Gluckman TJ, Hucker WJ, Januzzi JL Jr, Ortel TL, Saxonhouse SJ, Spinler SA (2017) 2017 ACC expert consensus decision pathway for periprocedural management of anticoagulation in patients with nonvalvular atrial fibrillation: A report of the American College of Cardiology Clinical Expert Consensus Document Task Force. J Am Coll Cardiol 69(7):871–898. https://doi.org/10.1016/j.jacc.2016.11.024
van Veen JJ, Makris M (2015) Management of peri-operative anti-thrombotic therapy. Anaesthesia 70(Suppl 1):58–67, e21-53. https://doi.org/10.1111/anae.12900
Steinhubl SR, Muse ED, Topol EJ (2013) Can mobile health technologies transform health care? JAMA 310(22):2395–2396. https://doi.org/10.1001/jama.2013.281078
Ergonomics of human-system interaction—part 210: human-centred design for interactive systems (ISO 9241-210:2010)
Keeling D, Baglin T, Tait C, Watson H, Perry D, Baglin C, Kitchen S, Makris M, British Committee for Standards in H (2011) Guidelines on oral anticoagulation with warfarin—fourth edition. Br J Haematol 154(3):311–324. https://doi.org/10.1111/j.1365-2141.2011.08753.x
Douketis JD, Spyropoulos AC, Kaatz S, Becker RC, Caprini JA, Dunn AS, Garcia DA, Jacobson A, Jaffer AK, Kong DF, Schulman S, Turpie AG, Hasselblad V, Ortel TL, Investigators B (2015) Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med 373(9):823–833. https://doi.org/10.1056/NEJMoa1501035
Birnie DH, Healey JS, Wells GA, Verma A, Tang AS, Krahn AD, Simpson CS, Ayala-Paredes F, Coutu B, Leiria TL, Essebag V, Investigators BC (2013) Pacemaker or defibrillator surgery without interruption of anticoagulation. N Engl J Med 368(22):2084–2093. https://doi.org/10.1056/NEJMoa1302946
Di Biase L, Burkhardt JD, Santangeli P, Mohanty P, Sanchez JE, Horton R, Gallinghouse GJ, Themistoclakis S, Rossillo A, Lakkireddy D, Reddy M, Hao S, Hongo R, Beheiry S, Zagrodzky J, Rong B, Mohanty S, Elayi CS, Forleo G, Pelargonio G, Narducci ML, Dello Russo A, Casella M, Fassini G, Tondo C, Schweikert RA, Natale A (2014) Periprocedural stroke and bleeding complications in patients undergoing catheter ablation of atrial fibrillation with different anticoagulation management: results from the Role of Coumadin in Preventing Thromboembolism in Atrial Fibrillation (AF) Patients Undergoing Catheter Ablation (COMPARE) randomized trial. Circulation 129(25):2638–2644. https://doi.org/10.1161/CIRCULATIONAHA.113.006426
Cappato R, Marchlinski FE, Hohnloser SH, Naccarelli GV, Xiang J, Wilber DJ, Ma CS, Hess S, Wells DS, Juang G, Vijgen J, Hugl BJ, Balasubramaniam R, De Chillou C, Davies DW, Fields LE, Natale A, Investigators V-A (2015) Uninterrupted rivaroxaban vs. uninterrupted vitamin K antagonists for catheter ablation in non-valvular atrial fibrillation. Eur Heart J 36(28):1805–1811. https://doi.org/10.1093/eurheartj/ehv177
Siegal D, Yudin J, Kaatz S, Douketis JD, Lim W, Spyropoulos AC (2012) Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation 126(13):1630–1639. https://doi.org/10.1161/CIRCULATIONAHA.112.105221
Amorosi SL, Tsilimingras K, Thompson D, Fanikos J, Weinstein MC, Goldhaber SZ (2004) Cost analysis of "bridging therapy" with low-molecular-weight heparin versus unfractionated heparin during temporary interruption of chronic anticoagulation. Am J Cardiol 93(4):509–511. https://doi.org/10.1016/j.amjcard.2003.10.060
Beyer-Westendorf J, Gelbricht V, Forster K, Ebertz F, Kohler C, Werth S, Kuhlisch E, Stange T, Thieme C, Daschkow K, Weiss N (2014) Peri-interventional management of novel oral anticoagulants in daily care: results from the prospective Dresden NOAC registry. Eur Heart J 35(28):1888–1896. https://doi.org/10.1093/eurheartj/eht557
Heidbuchel H, Verhamme P, Alings M, Antz M, Diener HC, Hacke W, Oldgren J, Sinnaeve P, Camm AJ, Kirchhof P (2015) Updated European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace 17(10):1467–1507. https://doi.org/10.1093/europace/euv309
Albaladejo P, Pernod G, Godier A, de Maistre E, Rosencher N, Mas JL, Fontana P, Samama CM, Steib A, Schlumberger S, Marret E, Roullet S, Susen S, Madi-Jebara S, Nguyen P, Schved JF, Bonhomme F, Sie P, members of the French Working Group on Perioperative H (2018) Management of bleeding and emergency invasive procedures in patients on dabigatran: updated guidelines from the French Working Group on Perioperative Haemostasis (GIHP)—September 2016. Anaesth Crit Care Pain Med 37(4):391–399. https://doi.org/10.1016/j.accpm.2018.04.009
Dunn AS, Spyropoulos AC, Turpie AG (2007) Bridging therapy in patients on long-term oral anticoagulants who require surgery: the Prospective Peri-operative Enoxaparin Cohort Trial (PROSPECT). J Thromb Haemost 5(11):2211–2218. https://doi.org/10.1111/j.1538-7836.2007.02729.x
Friberg L, Rosenqvist M, Lip GY (2012) Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J 33(12):1500–1510. https://doi.org/10.1093/eurheartj/ehr488
Baron TH, Kamath PS, McBane RD (2013) Management of antithrombotic therapy in patients undergoing invasive procedures. N Engl J Med 368(22):2113–2124. https://doi.org/10.1056/NEJMra1206531
Spyropoulos AC, Turpie AG, Dunn AS, Spandorfer J, Douketis J, Jacobson A, Frost FJ, Investigators R (2006) Clinical outcomes with unfractionated heparin or low-molecular-weight heparin as bridging therapy in patients on long-term oral anticoagulants: the REGIMEN registry. J Thromb Haemost 4(6):1246–1252. https://doi.org/10.1111/j.1538-7836.2006.01908.x
Falk V, Baumgartner H, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Muñoz DR, Rosenhek R, Sjögren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL; ESC Scientific Document Group (2017) 2017 ESC/EACTS Guidelines for the management of valvular heart disease Eur J Cardiothorac Surg 1;52(4):616–664. https://doi.org/10.1093/ejcts/ezx324
Indolfi C, Sabatino J, De Rosa S, Mongiardo A, Ricci P, Spaccarotella C (2017) Description and validation of TAVIApp: a novel mobile application for support of physicians in the management of aortic stenosis—management of aortic stenosis with TAVIApp. Biomed Res Int 2017:9027597–9027598. https://doi.org/10.1155/2017/9027597
van der Pligt P, Ball K, Hesketh KD, Teychenne M, Crawford D, Morgan PJ, Collins CE, Campbell KJ (2017) A pilot intervention to reduce postpartum weight retention and central adiposity in first-time mothers: results from the mums OnLiNE (Online, Lifestyle, Nutrition & Exercise) study. J Hum Nutr Diet 31:314–328. https://doi.org/10.1111/jhn.12521
Trivedi D (2015) Cochrane review summary: smartphone and tablet self-management apps for asthma. Prim Health Care Res Dev 16(2):111–113. https://doi.org/10.1017/S1463423615000018
Pais S, Parry D, Petrova K, Rowan J (2017) Acceptance of using an ecosystem of mobile apps for use in diabetes clinic for self-management of gestational diabetes mellitus. Stud Health Technol Inform 245:188–192
Muralidharan S, Mohan V, Anjana RM, Jena S, Tandon N, Allender S, Ranjani H (2017) Mobile health technology (mDiab) for the prevention of type 2 diabetes: protocol for a randomized controlled trial. JMIR Res Protoc 6(12):e242. https://doi.org/10.2196/resprot.8644
McManus DD, Lee J, Maitas O, Esa N, Pidikiti R, Carlucci A, Harrington J, Mick E, Chon KH (2013) A novel application for the detection of an irregular pulse using an iPhone 4S in patients with atrial fibrillation. Heart Rhythm 10(3):315–319. https://doi.org/10.1016/j.hrthm.2012.12.001
Matsumura K, Yamakoshi T (2013) iPhysioMeter: a new approach for measuring heart rate and normalized pulse volume using only a smartphone. Behav Res Methods 45(4):1272–1278. https://doi.org/10.3758/s13428-012-0312-z
Heo J, Chun M, Lee KY, Oh YT, Noh OK, Park RW (2013) Effects of a smartphone application on breast self-examination: a feasibility study. Healthc Inform Res 19(4):250–260. https://doi.org/10.4258/hir.2013.19.4.250
Chandrasekaran V, Dantu R, Jonnada S, Thiyagaraja S, Subbu KP (2013) Cuffless differential blood pressure estimation using smart phones. IEEE Trans Biomed Eng 60(4):1080–1089. https://doi.org/10.1109/TBME.2012.2211078
Curcio A, DER S, Sabatino J, DEL S, Bochicchio A, Polimeni A, Santarpia G, Ricci P, Indolfi C (2016) Clinical usefulness of a mobile application for the appropriate selection of the antiarrhythmic device in heart failure. Pacing Clin Electrophysiol 39(7):696–702. https://doi.org/10.1111/pace.12872
Douketis JD, Healey JS, Brueckmann M, Eikelboom JW, Ezekowitz MD, Fraessdorf M, Noack H, Oldgren J, Reilly P, Spyropoulos AC, Wallentin L, Connolly SJ (2015) Perioperative bridging anticoagulation during dabigatran or warfarin interruption among patients who had an elective surgery or procedure. Substudy of the RE-LY trial. Thromb Haemost 113(3):625–632. https://doi.org/10.1160/TH14-04-0305
Garcia DA, Regan S, Henault LE, Upadhyay A, Baker J, Othman M, Hylek EM (2008) Risk of thromboembolism with short-term interruption of warfarin therapy. Arch Intern Med 168(1):63–69. https://doi.org/10.1001/archinternmed.2007.23
Dunn AS, Turple AS (2003) Perioperative management of patients receiving oral anticoagulants: a systematic review. Arch Intern Med 163(8):901–908. https://doi.org/10.1001/archinte.163.8.901
Acknowledgments
We thank Jennifer Barrett, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
Study conception and design: MT, MT, FB, TM, RH. Acquisition of data: FB. Analysis and interpretation of data: MT, FB, TM, RH. Drafting the manuscript: MT, RH. Critical revision of the manuscript: DE, MJ, MS, TK, TM.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Ethik-Kommission Universität zu Lübeck, Aktenzeichen 19-105A) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Table 1
Sample procedures for different procedural risk categories for bleeding. Note: interv.: intervention (PPTX 52 kb)
Supplementary Table 2
20 hypothetical patients with AF, VTE, MHV and OAC requiring surgery. Note: OAC: oral anticoagulant, CrCl: creatinine clearance (DOCX 24 kb)
Supplementary Table 3
Demographics of study participants (DOCX 18 kb)
Supplementary Figure 1
Items of the task-based survey (PPTX 230 kb)
Rights and permissions
About this article
Cite this article
Thomaschewski, M., Beyer, F., Thomaschewski, M. et al. Application-based management of perioperative anticoagulant therapy: description of POPACTApp. Langenbecks Arch Surg 404, 633–645 (2019). https://doi.org/10.1007/s00423-019-01796-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-019-01796-9