Abstract
Purpose
Despite exhaustive research and improvement of techniques, anastomotic leakage remains a frequent complication in gastrointestinal surgery. As leakage is associated with poor perfusion, reliable objective methods to assess anastomotic perfusion are highly demanded. In addition, such methods enable evaluation of interventions that may improve anastomotic perfusion. Glucagon-like peptide 2 (GLP-2) is an enteroendocrine hormone that regulates mid-gut perfusion. In the present study, we aimed to explore if quantitative perfusion assessment with indocyanine green (q-ICG) could detect an increase in porcine anastomotic perfusion after treatment with GLP-2.
Methods
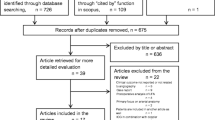
Nineteen pigs had two small bowel resections followed by anastomosis. Blinded to all investigators, animals were randomized to receive GLP-2 or placebo. Anastomotic perfusion was assessed at baseline, 30 min after injection of GLP-2/placebo, and after 5 days of treatment. Anastomotic strength and healing were evaluated by bursting pressure and histology.
Results
Q-ICG detected a significantly higher increase in anastomotic perfusion (p < 0.05) in animals treated with GLP-2, compared with placebo. No significant differences in anastomotic strength or healing were found.
Conclusions
Q-ICG is a promising tool for perfusion assessment in gastrointestinal surgery and opens new opportunities in research of factors that may influence anastomotic healing, but further research is warranted to evaluate the effects of GLP-2 on anastomotic healing.



Similar content being viewed by others
References
Markar S, Gronnier C, Duhamel A, Mabrut JY, Bail JP, Carrere N, Lefevre JH, Brigand C, Vaillant JC, Adham M, Msika S, Demartines N, Nakadi IE, Meunier B, Collet D, Mariette C, FREGAT (French Eso-Gastric Tumors) working group, FRENCH (Fédération de Recherche EN CHirurgie), and AFC (Association Française de Chirurgie) (2015) The impact of severe anastomotic leak on long-term survival and Cancer recurrence after surgical resection for esophageal malignancy. Ann Surg 262:972–980
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 253:890–899
Krarup PM, Jorgensen LN, Andreasen AH, Harling H, Danish Colorectal Cancer G (2012) A nationwide study on anastomotic leakage after colonic cancer surgery. Color Dis 14:e661–e667
Chadi SA, Fingerhut A, Berho M, DeMeester SR, Fleshman JW, Hyman NH, Margolin DA, Martz JE, McLemore EC, Molena D, Newman MI, Rafferty JF, Safar B, Senagore AJ, Zmora O, Wexner SD (2016) Emerging trends in the etiology, prevention, and treatment of gastrointestinal anastomotic leakage. J Gastrointest Surg 20:2035–2051
Hammond J, Lim S, Wan Y, Gao X, Patkar A (2014) The burden of gastrointestinal anastomotic leaks: an evaluation of clinical and economic outcomes. J Gastrointest Surg 18:1176–1185
Trencheva K, Morrissey KP, Wells M, Mancuso CA, Lee SW, Sonoda T, Michelassi F, Charlson ME, Milsom JW (2013) Identifying important predictors for anastomotic leak after colon and rectal resection: prospective study on 616 patients. Ann Surg 257:108–113
Vignali A, Gianotti L, Braga M, Radaelli G, Malvezzi L, Carlo VD (2000) Altered microperfusion at the rectal stump is predictive for rectal anastomotic leak. Dis Colon Rectum 43:76–82
Thompson SK, Chang EY, Jobe BA (2006) Clinical review: healing in gastrointestinal anastomoses, part I. Microsurgery 26:131–136
Karliczek A, Harlaar NJ, Zeebregts CJ, Wiggers T, Baas PC, van Dam GM (2009) Surgeons lack predictive accuracy for anastomotic leakage in gastrointestinal surgery. Int J Color Dis 24:569–576
Jafari MD, Wexner SD, Martz JE et al (2015) Perfusion assessment in laparoscopic left-sided/anterior resection (PILLAR II): a multi-institutional study. J Am Coll Surg 220:82–92 e81
Degett TH, Andersen HS, Gogenur I (2016) Indocyanine green fluorescence angiography for intraoperative assessment of gastrointestinal anastomotic perfusion: a systematic review of clinical trials. Langenbeck's Arch Surg 401:767–775
Nerup N, Andersen HS, Ambrus R, Strandby RB, Svendsen MBS, Madsen MH, Svendsen LB, Achiam MP (2017) Quantification of fluorescence angiography in a porcine model. Langenbeck's Arch Surg 402:655–662
Nerup N, Knudsen KBK, Ambrus R, Svendsen MBS, Thymann T, Ifaoui IBR, Svendsen LB, Achiam MP (2017) Reproducibility and reliability of repeated quantitative fluorescence angiography. Surg Technol Int 31:35–39
Nerup N, Ambrus R, Lindhe J, Achiam MP, Jeppesen PB, Svendsen LB (2017) The effect of glucagon-like peptide-1 and glucagon-like peptide-2 on microcirculation: a systematic review. Microcirculation. https://doi.org/10.1111/micc.12367
Guan X, Karpen HE, Stephens J, Bukowski JT, Niu S, Zhang G, Stoll B, Finegold MJ, Holst JJ, Hadsell DL, Nichols BL, Burrin DG (2006) GLP-2 receptor localizes to enteric neurons and endocrine cells expressing vasoactive peptides and mediates increased blood flow. Gastroenterology 130:150–164
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG (2010) Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol 8:e1000412
Sealed Envelope (2016) [Cited 2016 28.10]; Available from: https://www.sealedenvelope.com/
Renz BW, Leitner K, Odermatt E, Worthley DL, Angele MK, Jauch KW, Lang RA (2014) PVA gel as a potential adhesion barrier: a safety study in a large animal model of intestinal surgery. Langenbeck's Arch Surg 399:349–357
Zuhlke HV, Lorenz EM, Straub EM, Savvas V (1990) Pathophysiology and classification of adhesions. Langenbecks Arch Chir Suppl II Verh Dtsch Ges Chir 1990:1009–16
Goto T, Kawasaki K, Fujino Y, Kanemitsu K, Kamigaki T, Kuroda D, Suzuki Y, Kuroda Y (2007) Evaluation of the mechanical strength and patency of functional end-to-end anastomoses. Surg Endosc 21:1508–1511
Hartmann B, Johnsen AH, Orskov C et al (2000) Structure, measurement, and secretion of human glucagon-like peptide-2. Peptides 21:73–80
Attard JA, Raval MJ, Martin GR et al (2005) The effects of systemic hypoxia on colon anastomotic healing: an animal model. Dis Colon Rectum 48:1460–1470
Diana M, Halvax P, Dallemagne B, Nagao Y, Diemunsch P, Charles AL, Agnus V, Soler L, Demartines N, Lindner V, Geny B, Marescaux J (2014) Real-time navigation by fluorescence-based enhanced reality for precise estimation of future anastomotic site in digestive surgery. Surg Endosc 28:3108–3118
Diana M, Noll E, Diemunsch P, Dallemagne B, Benahmed MA, Agnus V, Soler L, Barry B, Namer IJ, Demartines N, Charles AL, Geny B, Marescaux J (2014) Enhanced-reality video fluorescence: a real-time assessment of intestinal viability. Ann Surg 259:700–707
Diana M, Agnus V, Halvax P, Liu YY, Dallemagne B, Schlagowski AI, Geny B, Diemunsch P, Lindner V, Marescaux J (2015) Intraoperative fluorescence-based enhanced reality laparoscopic real-time imaging to assess bowel perfusion at the anastomotic site in an experimental model. Br J Surg 102:e169–e176
Kudszus S, Roesel C, Schachtrupp A, Hoer JJ (2010) Intraoperative laser fluorescence angiography in colorectal surgery: a noninvasive analysis to reduce the rate of anastomotic leakage. Langenbeck's Arch Surg 395:1025–1030
Matsui A, Winer JH, Laurence RG, Frangioni JV (2011) Predicting the survival of experimental ischaemic small bowel using intraoperative near-infrared fluorescence angiography. Br J Surg 98:1725–1734
Mucke T, Reeps C, Wolff KD et al (2013) Objective qualitative and quantitative assessment of blood flow with near-infrared angiography in microvascular anastomoses in the rat model. Microsurgery 33:287–296
Jansen SM, de Bruin DM, van Berge Henegouwen MI et al (2018) Optical techniques for perfusion monitoring of the gastric tube after esophagectomy: a review of technologies and thresholds. Dis Esophagus 31(6). https://doi.org/10.1093/dote/dox161
Ambrus R, Strandby RB, Svendsen LB, Achiam MP, Steffensen JF, Søndergaard Svendsen MB (2016) Laser speckle contrast imaging for monitoring changes in microvascular blood flow. Eur Surg Res 56:87–96
Kaska M, Blazej S, Turek Z, Ryska A, Jegorov B, Radochova V, Bezouska J, Paral J (2018) The effect of three different surgical techniques for colon anastomosis on regional postoperative microperfusion: laser Doppler Flowmetry study in pigs. Clin Hemorheol Microcirc 68:61–70
Bremholm L, Hornum M, Henriksen BM, Larsen S, Holst JJ (2009) Glucagon-like peptide-2 increases mesenteric blood flow in humans. Scand J Gastroenterol 44:314–319
Ris F, Yeung T, Hompes R, Mortensen NJ (2015) Enhanced reality and intraoperative imaging in colorectal surgery. Clin Colon Rectal Surg 28:158–164
Sherwinter DA, Gallagher J, Donkar T (2013) Intra-operative transanal near infrared imaging of colorectal anastomotic perfusion: a feasibility study. Color Dis 15:91–96
Okamoto K, Muguruma N, Kimura T, Yano H, Imoto Y, Takagawa M, Kaji M, Aoki R, Sato Y, Okamura S, Kusaka Y, Ito S (2005) A novel diagnostic method for evaluation of vascular lesions in the digestive tract using infrared fluorescence endoscopy. Endoscopy 37:52–57
Redstone HA, Buie WD, Hart DA, Wallace L, Hornby PJ, Sague S, Holst JJ, Sigalet DL (2010) The effect of glucagon-like Peptide-2 receptor agonists on colonic anastomotic wound healing. Gastroenterol Res Pract 2010:1–12
He J, Ahuja N, Makary MA, Cameron JL, Eckhauser FE, Choti MA, Hruban RH, Pawlik TM, Wolfgang CL (2014) 2564 resected periampullary adenocarcinomas at a single institution: trends over three decades. HPB (Oxford) 16:83–90
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M, International Study Group on Pancreatic Fistula Definition (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Russell W, Burch R (1959) The principles of humane experimental technique. Methuen and co., London
Ohi M, Toiyama Y, Mohri Y, Saigusa S, Ichikawa T, Shimura T, Yasuda H, Okita Y, Yoshiyama S, Kobayashi M, Araki T, Inoue Y, Kusunoki M (2017) Prevalence of anastomotic leak and the impact of indocyanine green fluorescein imaging for evaluating blood flow in the gastric conduit following esophageal cancer surgery. Esophagus 14:351–359
Protyniak B, Dinallo AM, Boyan WP Jr, Dressner RM, Arvanitis ML (2015) Intraoperative indocyanine green fluorescence angiography--an objective evaluation of anastomotic perfusion in colorectal surgery. Am Surg 81:580–584
Armstrong G, Croft J, Corrigan N, Brown JM, Goh V, Quirke P, Hulme C, Tolan D, Kirby A, Cahill R, O'Connell PR, Miskovic D, Coleman M, Jayne D (2018) IntAct: intraoperative fluorescence angiography (IFA) to prevent anastomotic leak in rectal Cancer surgery: a randomised controlled trial. Color Dis 20:O226–O234
Acknowledgments
Authors sincerely thank Lars Thim, Ph.D., DMSci, Novo Nordisk, Denmark for providing the GLP-2 analog (NNCD 0103-0000-0066). Furthermore, we thank Professor Palle Bekker Jeppesen, Ph.D., DMSci, Department of Medical Gastroenterology, Rigshospitalet, Denmark for invaluable advice during the study design.
Funding
The study was sponsored by donations from private foundations: Mogens Andresen fonden, Civilingeniør Johannes Elmqvist Ormstrup og Hustru Grete Omstrups Fond, and Fabrikant Frands Køhler Nielsens og Hustrus Mindelegat. Sponsors had no role in study design, interpretation of results or any other part of the study.
Author information
Authors and Affiliations
Contributions
• Study conception and design: NN, LBS, MPA.
• Acquisition of data: NN, LLR, RBS, CE, MBS, JP, GLW, BH, LBS, MPA.
• Analysis and interpretation of data: NN, MBS, JP, GLW, BH, LBS, MPA.
• Drafting of the manuscript: NN.
• Critical revision and final approval of the manuscript: NN, LLR, RBS, CE, MBS, JP, GLW, BH, LBS, MPA.
Corresponding author
Ethics declarations
The study followed the Danish and European Union legislation on animal experimentation and was approved by the Danish Animal Experimentation Council (#2016-15-0201-01015).
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Rights and permissions
About this article
Cite this article
Nerup, N., Ring, L.L., Strandby, R.B. et al. Quantitative perfusion assessment of intestinal anastomoses in pigs treated with glucagon-like peptide 2. Langenbecks Arch Surg 403, 881–889 (2018). https://doi.org/10.1007/s00423-018-1718-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1718-6