Abstract
Purpose
The aims of the present study were to assess whether planned secondary wound closure at the insertion site of the circular stapler reduces wound infection rate and postoperative morbidity after laparoscopic Roux-en-Y gastric bypass (RYGB) and to identify independent predictive factors increasing the risk for wound infections after RYGB.
Methods
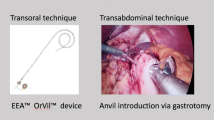
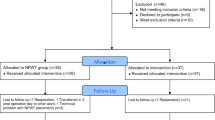
This paper is a retrospective single-center analysis of a prospectively collected database of 1400 patients undergoing RYGB surgery in circular technique between June 2000 and June 2016. Planned secondary wound closure at the circular stapler introduction site was performed at postoperative day 3 in 291 (20.8%) consecutive patients and compared to a historical control of 1109 (79.2%) consecutive patients with primary wound closure. Independent predictive factors for wound infection were assessed by multivariable analysis.
Results
Secondary wound closure significantly decreased wound infection rate from 9.3% (103/1109) to 1% (3/291) (p < 0.001) leading to a shorter hospital stay (mean 9 (SD8) vs. 7 days (SD2), p < 0.001), lower costs (p = 0.039), and reduced postoperative morbidity (mean 90-day Comprehensive Complication Index (CCI) 7.4 (SD14.0) vs. 5.1 (SD11.1) p = 0.008) when compared to primary wound closure. Primary wound closure, dyslipidemia, and preoperative gastritis were independent predictive risk factors for developing wound infections both in the univariate (p < 0.001; p = 0.048; p = 0.003) and multivariable analysis (p < 0.001; p = 0.040; p = 0.012). Further, on multivariable analysis, the female gender was a predictive factor (p = 0.034) for wound infection development.
Conclusions
Secondary wound closure at the circular stapler introduction site in laparoscopic RYGB significantly reduces the overall wound infection rate as well as postoperative morbidity, costs, and hospital stay when compared to primary wound closure.


Similar content being viewed by others
References
Shabanzadeh DM, Sorensen LT (2012) Laparoscopic surgery compared with open surgery decreases surgical site infection in obese patients: a systematic review and meta-analysis. Ann Surg 256(6):934–945. https://doi.org/10.1097/SLA.0b013e318269a46b
Leaper DJ, van Goor H, Reilly J, Petrosillo N, Geiss HK, Torres AJ, Berger A (2004) Surgical site infection—a European perspective of incidence and economic burden. Int Wound J 1(4):247–273. https://doi.org/10.1111/j.1742-4801.2004.00067.x
Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ (1999) The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol 20(11):725–730. https://doi.org/10.1086/501572
Arabshahi KS, Koohpayezade J (2006) Investigation of risk factors for surgical wound infection among teaching hospitals in Tehran. Int Wound J 3(1):59–62. https://doi.org/10.1111/j.1742-4801.2006.00176.x
Benoist S, Panis Y, Alves A, Valleur P (2000) Impact of obesity on surgical outcomes after colorectal resection. Am J Surg 179(4):275–281
Postlethwait RW, Johnson WD (1972) Complications following surgery for duodenal ulcer in obese patients. Arch Surg 105(3):438–440
Smith RL, Bohl JK, McElearney ST, Friel CM, Barclay MM, Sawyer RG, Foley EF (2004) Wound infection after elective colorectal resection. Ann Surg 239(5):599–605 discussion 605–597
Waisbren E, Rosen H, Bader AM, Lipsitz SR, Rogers SO Jr, Eriksson E (2010) Percent body fat and prediction of surgical site infection. J Am Coll Surg 210(4):381–389. https://doi.org/10.1016/j.jamcollsurg.2010.01.004
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 27(2):97–132 quiz 133–134; discussion 196
Kurz A, Sessler DI, Lenhardt R (1996) Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med 334(19):1209–1215. https://doi.org/10.1056/NEJM199605093341901
Latham R, Lancaster AD, Covington JF, Pirolo JS, Thomas CS Jr (2001) The association of diabetes and glucose control with surgical-site infections among cardiothoracic surgery patients. Infect Control Hosp Epidemiol 22(10):607–612. https://doi.org/10.1086/501830
Grey NJ, Perdrizet GA (2004) Reduction of nosocomial infections in the surgical intensive-care unit by strict glycemic control. Endocr Pract 10(Suppl 2):46–52. https://doi.org/10.4158/EP.10.S2.46
Hong B, Stanley E, Reinhardt S, Panther K, Garren MJ, Gould JC (2012) Factors associated with readmission after laparoscopic gastric bypass surgery. Surg Obes Relat Dis 8(6):691–695. https://doi.org/10.1016/j.soard.2011.05.019
Fujii T, Tsutsumi S, Matsumoto A, Fukasawa T, Tabe Y, Yajima R, Asao T, Kuwano H (2010) Thickness of subcutaneous fat as a strong risk factor for wound infections in elective colorectal surgery: impact of prediction using preoperative CT. Dig Surg 27(4):331–335. https://doi.org/10.1159/000297521
Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258(1):1–7. https://doi.org/10.1097/SLA.0b013e318296c732
Muller MK, Wildi S, Clavien PA, Weber M (2006) New device for the introduction of a circular stapler in laparoscopic gastric bypass surgery. Obes Surg 16(12):1559–1562. https://doi.org/10.1381/096089206779319437
rBiostatistics.com (2016) Cloud graphical user interface for R statistics and eLearning platform. Zurich, Switzerland
Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N (2015) Bariatric surgery worldwide 2013. Obes Surg 25(10):1822–1832. https://doi.org/10.1007/s11695-015-1657-z
Debergh I, Defoort B, De Visschere M, Flahou S, Van Cauwenberge S, Mulier JP, Dillemans B (2016) A one-step conversion from gastric banding to laparoscopic Roux-en-Y gastric bypass is as safe as a two-step conversion: a comparative analysis of 885 patients. Acta Chir Belg 116(5):271–277. https://doi.org/10.1080/00015458.2016.1255005
Steffen R, Guweidhi A, Metzger A, Z'Graggen K (2009) Advances in circular stapling techniques for gastric bypass: the circular stapler introducer. Obes Surg 19(4):504–507. https://doi.org/10.1007/s11695-009-9799-5
Giordano S, Salminen P, Biancari F, Victorzon M (2011) Linear stapler technique may be safer than circular in gastrojejunal anastomosis for laparoscopic Roux-en-Y gastric bypass: a meta-analysis of comparative studies. Obes Surg 21(12):1958–1964. https://doi.org/10.1007/s11695-011-0520-0
Schauer PR, Ikramuddin S, Gourash W, Ramanathan R, Luketich J (2000) Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg 232(4):515–529
Birkmeyer NJ, Dimick JB, Share D, Hawasli A, English WJ, Genaw J, Finks JF, Carlin AM, Birkmeyer JD, Michigan Bariatric Surgery C (2010) Hospital complication rates with bariatric surgery in Michigan. JAMA 304(4):435–442. https://doi.org/10.1001/jama.2010.1034
Wadhwa A, Kabon B, Fleischmann E, Kurz A, Sessler DI (2014) Supplemental postoperative oxygen does not reduce surgical site infection and major healing-related complications from bariatric surgery in morbidly obese patients: a randomized, blinded trial. Anesth Analg 119(2):357–365. https://doi.org/10.1213/ANE.0000000000000318
Zhang Y, Serrano OK, Scott Melvin W, Camacho D (2016) An intraoperative technique to reduce superficial surgical site infections in circular stapler-constructed laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 12(5):1008–1013. https://doi.org/10.1016/j.soard.2016.01.003
Kuy S, Dua A, Desai S, Dua A, Patel B, Tondravi N, Seabrook GR, Brown KR, Lewis BD, Lee CJ, Kuy S, Subbarayan R, Rossi PJ (2014) Surgical site infections after lower extremity revascularization procedures involving groin incisions. Ann Vasc Surg 28(1):53–58. https://doi.org/10.1016/j.avsg.2013.08.002
Delgado-Rodriguez M, Sillero-Arenas M, Medina-Cuadros M, Martinez-Gallego G (1997) Nosocomial infections in surgical patients: comparison of two measures of intrinsic patient risk. Infect Control Hosp Epidemiol 18(1):19–23
Isik O, Kaya E, Dundar HZ, Sarkut P (2015) Surgical site infection: re-assessment of the risk factors. Chirurgia (Bucur) 110(5):457–461
Aga E, Keinan-Boker L, Eithan A, Mais T, Rabinovich A, Nassar F (2015) Surgical site infections after abdominal surgery: incidence and risk factors. A prospective cohort study. Infect Dis (Lond) 47(11):761–767. https://doi.org/10.3109/23744235.2015.1055587
Petro CC, Posielski NM, Raigani S, Criss CN, Orenstein SB, Novitsky YW (2015) Risk factors for wound morbidity after open retromuscular (sublay) hernia repair. Surgery 158(6):1658–1668. https://doi.org/10.1016/j.surg.2015.05.003
Summers JI, Ziembicki JA, Corcos AC, Peitzman AB, Billiar TR, Sperry JL (2014) Characterization of sex dimorphism following severe thermal injury. J Burn Care Res 35(6):484–490. https://doi.org/10.1097/BCR.0000000000000018
Bird MD, Karavitis J, Kovacs EJ (2008) Sex differences and estrogen modulation of the cellular immune response after injury. Cell Immunol 252(1–2):57–67. https://doi.org/10.1016/j.cellimm.2007.09.007
Tongyoo A, Chatthamrak P, Sriussadaporn E, Limpavitayaporn P, Mingmalairak C (2015) Risk assessment of abdominal wall thickness measured on pre-operative computerized tomography for incisional surgical site infection after abdominal surgery. J Med Assoc Thail 98(7):677–683
Kwaan MR, Sirany AM, Rothenberger DA, Madoff RD (2013) Abdominal wall thickness: is it associated with superficial and deep incisional surgical site infection after colorectal surgery? Surg Infect 14(4):363–368. https://doi.org/10.1089/sur.2012.109
Bosch TA, Chow L, Dengel DR, Melhorn SJ, Webb M, Yancey D, Callahan H, De Leon MR, Tyagi V, Schur EA (2015) In adult twins, visceral fat accumulation depends more on exceeding sex-specific adiposity thresholds than on genetics. Metabolism 64(9):991–998. https://doi.org/10.1016/j.metabol.2015.06.002
Lemieux S, Despres JP, Moorjani S, Nadeau A, Theriault G, Prud'homme D, Tremblay A, Bouchard C, Lupien PJ (1994) Are gender differences in cardiovascular disease risk factors explained by the level of visceral adipose tissue? Diabetologia 37(8):757–764
Gerig R, Ernst B, Wilms B, Thurnheer M, Schultes B (2013) Gastric Helicobacter pylori infection is associated with adverse metabolic traits in severely obese subjects. Obesity (Silver Spring) 21(3):535–537. https://doi.org/10.1002/oby.20098
Ieni A, Barresi V, Rigoli L, Fedele F, Tuccari G, Caruso RA (2016) Morphological and cellular features of innate immune reaction in Helicobacter pylori gastritis: a brief review. Int J Mol Sci 17(1). https://doi.org/10.3390/ijms17010109
Lyons T, Neff KJ, Benn J, Chuah LL, le Roux CW, Gilchrist M (2014) Body mass index and diabetes status do not affect postoperative infection rates after bariatric surgery. Surg Obes Relat Dis 10(2):291–297. https://doi.org/10.1016/j.soard.2013.10.006
Mullen JT, Moorman DW, Davenport DL (2009) The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Ann Surg 250(1):166–172. https://doi.org/10.1097/SLA.0b013e3181ad8935
Bamgbade OA, Rutter TW, Nafiu OO, Dorje P (2007) Postoperative complications in obese and nonobese patients. World J Surg 31(3):556–560; discussion 561. https://doi.org/10.1007/s00268-006-0305-0
Author information
Authors and Affiliations
Contributions
Diana Vetter contributed to the study design, interpretation and analysis of data, and writing of the manuscript; Dimitri A. Raptis, study design, statistical analysis and interpretation of the data, and revision of the manuscript; Mira Giama, data acquisition and revision of the manuscript; Hanna Hosa, data acquisition and revision of the manuscript; Markus K. Mueller, acquisition of patients and their data and critical revision of the manuscript; Antonio Nocito, acquisition of patients and their data and critical revision of the manuscript; Marc Schiesser, acquisition of patients and their data and critical revision of the manuscript; Marco Bueter, study concept and design, interpretation of data, and critical revision of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The institutional review board (IRB) of the Canton Zurich, Switzerland, approved the study (KEK-ZH-Nr.2016-00022). Informed consent was not necessary, as the analysis used anonymous, routine clinical data from our hospital. Patient data were anonymized and de-identified prior to analysis. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Vetter, D., Raptis, D.A., Giama, M. et al. Planned secondary wound closure at the circular stapler insertion site after laparoscopic gastric bypass reduces postoperative morbidity, costs, and hospital stay. Langenbecks Arch Surg 402, 1255–1262 (2017). https://doi.org/10.1007/s00423-017-1632-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-017-1632-3