Abstract
Purpose
The growing pressure to rationalize costs in the healthcare system demands the development of new healthcare models aimed at allowing patients to receive the best treatment, without ignoring the rising costs.
Methods
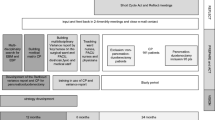
In the Healthcare Unit 2 located in the Abruzzo region in Italy, a new model of intensified care surgical department was designed in January 2013. The department was based on the selection of the degree of patient disease. Patients requiring a medium-low degree surgery were treated in the peripheral unit, in the Ortona hospital, while more complex surgical procedures, most cancer cases (including stomach, liver, pancreas, colon-rectum or multi-organ resections), were performed in the central unit in the Chieti hospital.
Results
The value of production at the peripheral unit, in Ortona, increased by 299.4% along with an increase in discharges of 112.6%, with an average DRG weight from 1.02 to 1.45. At the central unit, in Chieti, the average DRG weight produced was 3.328. In relation to quality assessment, pancreatic surgery morbidity was 27.0% and mortality was 1.7 % due to resection and 2.2% for other causes. Likewise, for colon-rectal surgery, a global morbidity of 35.0% and anastomotic leakage of 3.9% was seen.
Conclusions
The 24-month preliminary results show that new models of intensified care surgical departments can be created. In addition, results clearly show that such model significantly improves both services and surgical results. This original model allows optimal use of resources favouring both service quality and patient satisfaction.
Similar content being viewed by others
Abbreviations
- LEA:
-
Basic care levels
- ICSD:
-
Intensified care surgical department
- DRG:
-
Diagnosis-related groups,
- GICO:
-
Interdisciplinary cancer care group.
References
Welsch T, von Frankenberg M, Simon T, Weitz J, Juestel D, Buechler MW (2012) Krankenhaus-kooperationsmodelle. Chirurg 83:274–279
Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE (2002) Hospital volume and surgical mortality in the United States. N Engl J Med 346(15):1128–1137
Genovesi D, Mazzilli L, Trignani M, DI Tommaso M et al (2014) Developing a decision-making model based on an interdisciplinary oncological care group for the management of colorectal cancer. Anticancer Res 34(5):2525–2531
Balzano G, Zerbi A, Capretti G, Rocchetti S, Capitanio V, Di Carlo V (2008) Effect of hospital volume on outcome of pancreaticoduodenectomy in Italy. Br J Surg 95(3):357–362
Bassi C, Dervenis C, Butturini G, Fingerhut et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
DeOliveira ML, Winter JM, Schafer M, Cunningham SC et al (2006) Assessment of complications after pancreatic surgery: a novel grading system applied to 633 patients undergoing pancreaticoduodenectomy. Ann Surg 244(6):931–937
Liu CJ, Chou YJ, Teng CJ, Lin CC, Lee YT et al (2015) Association of surgeon volume and hospital volume with the outcome of patients receiving definitive surgery for colorectal cancer: a nationwide population-based study. Cancer 121(16):2782–2790
Fischer C, Lingsma HF, van Leersum N, Tollenaar RA et al (2015) Comparing colon cancer outcomes: the impact of low hospital case volume and case-mix adjustment. Eur J Surg Oncol 41(8):1045–1053
de Wilder RF, Besselink MG, van der Tweel I et al (2012) Impact of nationwide centralization of pancreaticoduodenectomy on hospital mortality. Brit J Surg 99:404–410
Yoshioka R, Yanusaga H, Hasegawa K et al (2014) Impact of hospital volume on hospital mortality, length of stay and total costs after duodenopancreatectomy. Br J Surg 101:523–529
Finks JF, Osborne NH, Birkmeyer JD (2011) Trends in hospital volume and operative mortality for high risk surgery. N Engl J Med 364:2128–2137
di Sebastiano P, Festa L, De Bonis A, Ciuffreda A, Valvano MR, Andriulli A, di Mola FF (2011) A modified fast-track program for pancreatic surgery: a prospective single-center experience. Langenbeck's Arch Surg 396(3):345–351
di Mola FF, Tavano F, Rago RR, De Bonis A, Valvano MR, Andriulli A, di Sebastiano P (2014) Influence of preoperative biliary drainage on surgical outcome after pancreaticoduodenectomy: single centre experience. Langenbeck's Arch Surg 399(5):649–657
Egger B, Schmid SW, Schafer M et al (2001) 2-year evaluation of a cooperation model between a surgical university clinic and a general hospital. Chirurg 72:30–36
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All authors declare no conflict of interest. For the present study, no grant were received by any of the authors. This article does not contain any studies with human participants or animals performed by any of the authors. For this type of study, formal consent is not required.
However, all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
di Sebastiano, P., Grottola, T., Maysse, A. et al. A surgical department for intensified care. Langenbecks Arch Surg 402, 475–479 (2017). https://doi.org/10.1007/s00423-016-1523-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1523-z