Abstract
Background
Based on the AJCC seventh TNM classification, T1 intraglandular tumors are subdivided into T1a (≤10 mm) and T1b (11–20 mm), but the differences in prognosis remain controversial. The present study aimed to determine the clinicopathological features and outcomes of T1a and T1b patients.
Methods
A retrospective study of 2518 T1 patients, including 1840 T1a (73 %) and 678 (27 %) T1b patients who underwent surgery for PTC from 1978 to 2014, was conducted. In patients with a preoperative or operative diagnosis of PTC, a total thyroidectomy (TT) with prophylactic (macroscopically N0) or therapeutic (evident N1) lymph node dissection (LND) was performed. Other patients had a TT or partial thyroidectomy without LND. The mean follow-up time was 8.9 ± 8.8 years (median, 6.5 years; range, 1–36.4 years).
Results
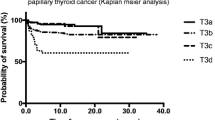
A TT was performed in 2273 patients (90 %), including 1184 (52 %) with LND. Other patients (n = 245) had a single lobectomy with isthmectomy. Multifocality, bilaterality, number of tumors, sum of the largest size of all foci, vascular invasion, and (in patients with LND) LN metastases were significantly more frequent in T1b than in T1a patients. Of the 1184 patients with LND, 278 had LN metastases (N1, 23 %), including 136/680 T1a (20 %) and 142/504 (28 %) T1b patients (p = 0.002). These LN metastases were diagnosed after a prophylactic LND in 86/609 T1a (14 %) and 93/440 T1b (21 %) patients (p = 0.001). Recurrences were more frequent in T1b (n = 26, 3.8 %) than in T1a patients (n = 35, 1.9 %, p = 0.005). In the multivariate analysis, independent prognostic factors for recurrence in both groups were the number of tumors, the sum of the largest size of all foci and, in patients who had LND, LN metastases and extranodal extension. For N0-x patients, the recurrence rate was significantly higher in the T1b than in the T1a group (2.4 vs. 0.9 %, respectively, p = 0.005), although this rate was similar in N1 patients (16.2 % for T1a and 9.2 % for T1b patients, p = 0.1). The 5-year disease-free survival rates for T1a and T1b patients were 98.3 and 96.6 %, respectively (p = 0.01).
Conclusion
For PTC patients, T1b had poorer clinicopathological features and increased risk of recurrence than T1a.

Similar content being viewed by others
References
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295(18):2164–7
Bilimoria KY, Bentrem DJ, Linn JG, Freel A, Yeh JJ, Stewart AK, Winchester DP, Ko CY, Talamonti MS, Sturgeon C (2007) Utilization of total thyroidectomy for papillary thyroid cancer in the United States. Surgery 142(6):906–13
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–4
(2015) American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid
Ito Y, Fukushima M, Higashiyama T, Kihara M, Takamura Y, Kobayashi K, Miya A, Miyauchi A (2013) Tumor size is the strongest predictor of microscopic lymph node metastasis and lymph node recurrence of N0 papillary thyroid carcinoma. Endocr J 60(1):113–7
Pellegriti G, Scollo C, Lumera G, Regalbuto C, Vigneri R, Belfiore A (2004) Clinical behavior and outcome of papillary thyroid cancers smaller than 1.5 cm in diameter: study of 299 cases. J Clin Endocrinol Metab 89(8):3713–20
Wang LY, Nixon IJ, Palmer FL, Thomas D, Tuttle RM, Shaha AR, Patel SG, Shah JP, Ganly I (2014) Comparable outcomes for patients with pT1a and pT1b differentiated thyroid cancer: is there a need for change in the AJCC classification system? Surgery 156(6):1484–9, discussion 1489-90
Ito Y, Masuoka H, Fukushima M, Inoue H, Kihara M, Tomoda C, Higashiyama T, Takamura Y, Kobayashi K, Miya A, Miyauchi A (2010) Excellent prognosis of patients with solitary T1N0M0 papillary thyroid carcinoma who underwent thyroidectomy and elective lymph node dissection without radioiodine therapy. World J Surg 34(6):1285–90
Ducoudray R, Trésallet C, Godiris-Petit G, Tissier F, Leenhardt L, Menegaux F (2013) Prophylactic lymph node dissection in papillary thyroid carcinoma: is there a place for lateral neck dissection? World J Surg 37:1584–91
Ito Y, Miyauchi A, Kihara M, Kobayashi K, Miya A (2014) Prognostic values of clinical lymph node metastasis and macroscopic extrathyroid extension in papillary thyroid carcinoma. Endocr J 61(8):745–50
Reddy RM, Grigsby PW, Moley JF, Hall BL (2006) Lymph node metastases in differentiated thyroid cancer under 2 cm. Surgery 140(6):1050–4, discussion 1054-5
Rossi R, Roti E, Trasforini G, Pansini G, Cavazzini L, Zatelli MC, Pearce EN, Braverman LE, Uberti EC (2008) Differentiated thyroid cancers 11–20 mm in diameter have clinical and histopathologic characteristics suggesting higher aggressiveness than those < or =10 mm. Thyroid 18(3):309–15
Nilubol N, Kebebew E (2015) Reply to most patients with a small papillary thyroid carcinoma enjoy an excellent prognosis and may be managed with minimally invasive therapy or active surveillance. Cancer 121(18):3365–6
Machens A, Holzhausen HJ, Dralle H (2005) The prognostic value of primary tumor size in papillary and follicular thyroid carcinoma. Cancer 103:2269–2273
Bonnet S, Hartl D, Leboulleux S, Baudin E, Lumbroso JD, Al Ghuzlan A, Chami L, Schlumberger M, Travagli JP (2009) Prophylactic lymph node dissection for papillary thyroid cancer less than 2 cm: implications for radioiodine treatment. J Clin Endocrinol Metab 94(4):1162–7
Hartl DM, Leboulleux S, Al GA, Baudin E, Chami L, Schlumberger M, Travagli JP (2012) Optimization of staging of the neck with prophylactic central and lateral neck dissection for papillary thyroid carcinoma. Ann Surg 255:777–783
Sancho JJ, Lennard TW, Paunovic I, Triponez F, Sitges-Serra A (2014) Prophylactic central neck dissection in papillary thyroid cancer: a consensus report of the European Society of Endocrine Surgeons (ESES). Langenbecks Arch Surg 399:155–163
Dralle H et al (2013) German Societies of General and Visceral Surgery; Endocrinology; Nuclear Medicine; Pathology; Radiooncology; Oncological Hematology; and the German Thyroid Cancer Patient Support Organization Ohne Schilddrüse leben e.V. German Association of Endocrine Surgeons practice guideline for the surgical management of malignant thyroid tumors. Langenbecks Arch Surg 398(3):347–75
Qu N, Zhang L, Ji QH, Chen JY, Zhu XY, Cao YM, Shen Q (2015) Risks factors for central lymph node metastasis in papillary thyroid microcarcinoma: a meta-analysis. World J Surg 39(10):2459–70
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Author contributions
Study conception and design were performed by Chereau, Trésallet, Godiris Petit, Noullet, Tissier, Leenhardt, and Menegaux.
Data acquisition was performed by Chereau, Trésallet, Godiris Petit, Noullet, Tissier, Leenhardt, and Menegaux.
Data analysis and interpretation were performed by Chereau and Menegaux.
Drafting of manuscript was performed by Chereau, Trésallet, and Menegaux.
Critical revision of manuscript was performed by Chereau, Trésallet, Tissier, Leenhardt, and Menegaux.
Rights and permissions
About this article
Cite this article
Chereau, N., Trésallet, C., Noullet, S. et al. Does the T1 subdivision correlate with the risk of recurrence of papillary thyroid cancer?. Langenbecks Arch Surg 401, 223–230 (2016). https://doi.org/10.1007/s00423-016-1399-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1399-y