Abstract
Purpose
Resident participation in operative procedures is mandatory in educational residency programs but remains controversial, especially in the context of patient safety. This study compared the surgical quality and outcomes of thyroidectomies performed by surgical residents (RESs) and board-certified surgeons (BCSs).
Methods
This retrospective matched-pair study included patients undergoing thyroidectomies for multinodular goiter, Grave’s disease and early-stage thyroid cancer that were performed by a RES with BCS supervision between 2006 and 2014. The intraoperative and postoperative course, complication rates and handling of the recurrent laryngeal nerve (RLN) and parathyroid glands were analyzed.
Results
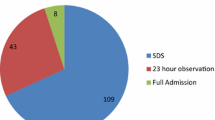
In total, 112 thyroidectomies that were performed by a RES fulfilled the inclusion criteria and were matched 1:1 with BCS patients. We included 88 hemithyroidectomies, 80 subtotal thyroidectomies and 56 total thyroidectomies. No significant differences in the handling of the RLN or parathyroid glands, the rates of postoperative RLN palsies or the rates of hypocalcaemia were found. No intraoperative complications led to the replacement of the RES as the surgeon-in-charge. Three RES and two BCS patients experienced postoperative haemorrhages (p = 0.205), and three surgical site infections (p = 1.000) occurred in each group. The mean operative time and the length of stay did not differ significantly between the two groups.
Conclusions
Major aspects of patient safety in thyroid surgery are not affected by resident participation. Thyroidectomies performed by RES are not significantly longer and reveal no differences in length of stay or complication rates. The economic burden of resident involvement is modest.


Similar content being viewed by others
References
Porta CR, Sebesta JA, Brown TA, Steele SR, Martin MJ (2012) Training surgeons and the informed consent process: routine disclosure of trainee participation and its effect on patient willingness and consent rates. Arch Surg 147:57–62
Kasotakis G, Lakha A, Sarkar B, Kunitake H, Kissane-Lee N, Dechert T, McAneny D, Burke P, Doherty G (2014) Trainee participation is associated with adverse outcomes in emergency general surgery: an analysis of the National Surgical Quality Improvement Program database. Ann Surg 260:483–490
Davis SS, Husain FA, Lin E, Nandipati KC, Perez S, Sweeney JF (2013) Resident participation in index laparoscopic general surgical cases: impact of the learning environment on surgical outcomes. J Am Coll Surg 216:96–104
Sakran JV, Hoffman RL, Ko C, Kelz RR (2013) The ACS NSQIP quality in-training initiative: educating residents to ensure the future of optimal surgical care. Bull Am Coll Surg 98:30–35
Relles DM, Burkhart RA, Pucci MJ, Sendecki J, Tholey R, Drueding R, Sauter PK, Kennedy EP, Winter JM, Lavu H, Yeo CJ (2014) Does resident experience affect outcomes in complex abdominal surgery? Pancreaticoduodenectomy as an example. J Gastrointest Surg 18:279–285
Hernández-Irizarry R, Zendejas B, Ali SM, Lohse CM, Farley DR (2012) Impact of resident participation on laparoscopic inguinal hernia repairs: are residents slowing us down? J Surg Educ 69:746–752. doi:10.1016/j.jsurg.2012.08.013
de Santibañes M, Alvarez FA, Sieling E, Vaccarezza H, de Santibañes E, Vaccaro CA (2015) Postoperative complications at a university hospital: is there a difference between patients operated by supervised residents vs. trained surgeons? Langenbeck’s Arch Surg 400:77–82. doi:10.1007/s00423-014-1261-z
Schreckenbach T, El Yourouri H, Bechstein EO, Habbe N (2015) Proctologic surgery done by residents—complications pre-programmed? J Visc Surg. doi:10.1016/j.jviscsurg.2015.11.013
(Muster) Weiterbildungsordung der Bundesärztekammer von 2003 mit den Erweiterungen und Ergänzungen 2013 [(Model) Specialty Training Regulations 2003 as amended on 28/06/2013]; (Model) Specialty Training Regulations 2003 as amended on 28/06/2013. http://www.bundesaerztekammer.de/fileadmin/user_upload/downloads/MWBO_Englisch_210113_FINFI_aktualisiert171214.pdf. Accessed 12 Jan 2016
The American Board of Surgery; Training and Certification http://www.absurgery.org/xfer/curriculumoutline2014-15.pdf. Accessed 12 Jan 2016
Buerba R, Roman SA, Sosa JA (2011) Thyroidectomy and parathyroidectomy in patients with high body mass index are safe overall: analysis of 26,864 patients. Surgery 150:950–958. doi:10.1016/j.surg.2011.02.017
Ejaz A, Spolverato G, Kim Y, Wolfgang CL, Hirose K, Weiss M, Makary MA, Pawlik TM (2015) The impact of resident involvement on surgical outcomes among patients undergoing hepatic and pancreatic resections. Surgery 158:323–330. doi:10.1016/j.surg.2015.01.027
Hayward NJ, Grodski S, Yeung M, Johnson WR, Serpell J (2013) Recurrent laryngeal nerve injury in thyroid surgery: a review. ANZ J Surg 83:15–21. doi:10.1111/j.1445-2197.2012.06247.x
Dralle H, Sekulla C, Haerting J, Timmermann W, Neumann HJ, Kruse E, Grond S, Mühlig HP, Richter C, Voss J, Thomusch O, Lippert H, Gastinger I, Brauckhoff M, Gimm O (2004) Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery 136:1310–1322
Thomusch O, Machens A, Sekulla C, Ukkat J, Lippert H, Gastinger I, Dralle H (2000) Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: prospective multicenter study in Germany. World J Surg 24:1335–1341
Shaha A, Jaffe BM (1988) Complications of thyroid surgery performed by residents. Surgery 104:1109–1114
Cheng H, Soleas I, Ferko NC, Clymer JW, Amaral JF (2015) A systematic review and meta-analysis of harmonic focus in thyroidectomy compared to conventional techniques. Thyroid Res 8:15. doi:10.1186/s13044-015-0027-1
Ross SW, Oommen B, Kim M, Walters AL, Green JM, Heniford BT, Augenstein VA (2014) A little slower, but just as good: postgraduate year resident versus attending outcomes in laparoscopic ventral hernia repair. Surg Endosc 28:3092–3100. doi:10.1007/s00464-014-3586-7
Fanous M, Carlin A (2012) Surgical resident participation in laparoscopic Roux-en-Y bypass: is it safe? Surgery 152:21–25. doi:10.1016/j.surg.2012.02.014
Uecker J, Luftman K, Ali S, Brown C (2013) Comparable operative times with and without surgery resident participation. J Surg Educ 70:696–699. doi:10.1016/j.jsurg.2013.06.011
Zendejas B, Cook DA, Bingener J, Huebner M, Dunn WF, Sarr MG, Farley DR (2011) Simulation-based mastery learning improves patient outcomes in laparoscopic inguinal hernia repair: a randomized controlled trial. Ann Surg 254:502–509. doi:10.1097/SLA.0b013e31822c6994
Jolley J, Lomelin D, Simorov A, Tadaki C, Oleynikov D (2015) Resident involvement in laparoscopic procedures does not worsen clinical outcomes but may increase operative times and length of hospital stay. Surg Endosc
Authors’ contributions
Study conception and design: Alexander Reinisch and Nils Habbe
Acquisition of data: Alexander Reinisch, Patrizia Malkomes and Katharina Holzer
Analysis and interpretation of data: Alexander Reinisch, Juliane Liese and Nils Habbe
Drafting of manuscript: Alexander Reinisch
Critical revision of manuscript: Nils Habbe, Juliane Liese, Wolf Otto Bechstein, Teresa Schreckenbach and Juliane Liese
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was not funded.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the local ethical committee of Frankfurt University (IRB No. 236/14).
Rights and permissions
About this article
Cite this article
Reinisch, A., Malkomes, P., Liese, J. et al. Education in thyroid surgery: a matched-pair analysis comparing residents and board-certified surgeons. Langenbecks Arch Surg 401, 239–247 (2016). https://doi.org/10.1007/s00423-016-1390-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1390-7