Abstract
Background
Multifocal papillary thyroid carcinoma (MPTC) has been reported in literature in 18–87 % of cases. This paper aims to review controversies in the molecular pathogenesis, prognosis, and management of MPTC.
Methods
A review of English-language literature focusing on MPTC was carried out, and analyzed in an evidence-based perspective. Results were discussed at the 2013 Workshop of the European Society of Endocrine Surgeons devoted to surgery of thyroid carcinoma.
Results
Literature reports no prospective randomized studies; thus, a relatively low level of evidence may be achieved.
Conclusions
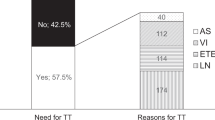
MPTC could be the result of either true multicentricity or intrathyroidal metastasis from a single malignant focus. Radiation and familial nonmedullary thyroid carcinoma are conditions at risk of MPTC development. The prognostic importance of multifocal tumor growth in PTC remains controversial. Prognosis might be impaired in clinical MPTC but less or none in MPTC <1 cm. MPTC can be diagnosed preoperatively by FNAB and US, with low sensitivity for MPTC <1 cm. Total or near-total thyroidectomy is indicated to reduce the risk of local recurrence. Prophylactic central node dissection should be considered in patients with total tumor diameter >1 cm, or in cases with high number of cancer foci. Completion thyroidectomy might be necessary when MPTC is diagnosed after less than near-total thyroidectomy. Radioactive iodine ablation should be considered in selected patients with MPTC at increased risk of recurrence or metastatic spread.
Similar content being viewed by others
References
Hundahl SA, Fleming ID, Fremgen AM, Menck HR (1998) A National Cancer Data Base report on 53 856 cases of thyroid carcinoma treated in the US, 1985–1995. Cancer 83:2638–2648
Leenhardt L, Bernier MO, Boin-Pineau MH et al (2004) Advances in diagnostic practices affect thyroid cancer incidence in France. Eur J Endocrinol 150:133–139
Kuhn E, Teller L, Piana S et al (2012) Different clonal origin of bilateral papillary thyroid carcinoma, with a review of the literature. Endocr Pathol 23:101–107
Carcangiu ML, Zampi G, Pupi A et al (1985) Papillary carcinoma of the thyroid—A clinicopathologic study of 247 cases treated at the University of Florence, Italy. Cancer 55:805–828
Katoh R, Sasaki J, Kurihara H et al (1992) Multiple thyroid involvement (intraglandular metastasis) in papillary thyroid carcinoma: a clinicopathologic study of 105 consecutive patients. Cancer 70:1585–1590
Mazzaferri EL, Jhiang SM (1994) Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 97:418–428
Mazeh H, Samet Y, Hochstein D et al (2011) Multifocality in well-differentiated thyroid carcinomas calls for total thyroidectomy. Am J Surg 201:770–775
Bogdanova TI, Zurnadzhy LY, Greenebaum E et al (2006) A cohort study of thyroid cancer and other thyroid diseases after the Chernobyl accident. Cancer 107:2559–2566
Ron E, Lubin JH, Shore RE et al (1995) Thyroid cancer after exposure to external radiation: a pooled analysis of seven studies. Radiat Res 141:259–277
Nikiforov YE (2006) Radiation-induced thyroid cancer: what we have learned from Chernobyl. Endocr Pathol 17:307–317
Fridman MV, Savva NN, Krasko OV et al (2012) Clinical and pathologic features of “sporadic” papillary thyroid carcinoma registered in the years 2005 to 2008 in children and adolescents of Belarus. Thyroid 22:1016–1024
Lee KJ, Cho YJ, Kim JG et al (2013) How many contralateral papillary thyroid carcinomas can be missed? World J Surg 4:780–785
Kim HJ, Sohn SY, Jang HW et al (2013) Multifocality, but not bilaterality, is a predictor of disease recurrence/persistence of papillary thyroid carcinoma. World J Surg 37:376–384
Schonberger J, Marienhagen J, Agha A et al (2007) Papillary microcarcinoma and papillary cancer of the thyroid < or = 1 cm: modified definition of the WHO and the therapeutic dilemma. Nuklearmedizin 46:115–120
Pasieka JL, Thompson NW, McLeod MK et al (1992) The incidence of bilateral well-differentiated thyroid cancer found at completion thyroidectomy. World J Surg 16:711–716
Agency for Health Care Policy and Research (1992) Acute pain management: operative or medical procedures and trauma. Clinical practice guideline number 1. AHCPR, Rockville, p 107.
Agency for Health Care Policy and Research (1994) Management of cancer pain: adults. Clinical practice guideline number 9. AHCPR, Rockville.
Iida F, Yonekura M, Miyakawa M (1969) Study of intraglandular dissemination of thyroid cancer. Cancer 24:764–771
Shattuck TM, Westra WH, Ladenson et al (2005) Independent clonal origins of distinct tumor foci in multifocal
McCarthy RP, Wang M, Jones TD, Strate RW, Cheng L (2006) Molecular evidence for the same clonal origin of multifocal papillary thyroid carcinomas. Clin Cancer Res 12:2414–2418
Wang W, Wang H, Teng X et al (2010) Clonal analysis of bilateral, recurrent, and metastatic papillary thyroid carcinomas. Hum Pathol 41:1299–1309
Jovanovic L, Delahunt B, McIver B et al (2008) Most multifocal papillary thyroid carcinomas acquire genetic and morphotype diversity through subclonal evolution following the intraglandular spread of the initial neoplastic clone. J Pathol 215:145–154
Sugg SL, Ezzat S, Rosen IB et al (1998) Distinct multiple RET/PTC gene rearrangements in multifocal papillary thyroid neoplasia. J Clin Endocrinol Metab 83:4116–4122
Moniz S, Catarino AL, Marques AR et al (2002) Clonal origin of nonmedullary thyroid tumors assessed by nonrandom X-chromosome inactivation. Eur J Endocrinol 146:27–33
Park SY, Park YJ, Lee YJ et al (2006) Analysis of differential BRAFV600E mutational status in multifocal papillary thyroid carcinoma: evidence of independent clonal origin in distinct tumor foci. Cancer 107:1831–1838
Lin X, Finkelstein SD, Zhu B et al (2008) Molecular analysis of multifocal papillary thyroid carcinoma. J Mol Endocrinol 41:195–203
Wang W, Zhao W, Whang H et al (2012) Poorer prognosis and higher prevalence of BRAFV600Emutation in synchronous bilateral papillary thyroid carcinoma. Ann Surg Oncol 19:31–36
De Vries JH (2005) Multifocal papillary thyroid carcinoma. N Engl J Med 353:1067
Lin JD, Chao TC, Hsueh C et al (2009) High recurrent rate of multicentric papillary thyroid carcinoma. Ann Surg Oncol 16:2609–2616
Mazzaferri EL, Kloos RT (2001) Clinical review 128: current approaches to primary therapy for papillary thyroid cancer. J Clin Endocrinol Metab 86:1447–1463
Kirath PÖ, Volkan- Salanci B, Günay EC et al (2011) Thyroid cancer in pediatric age group: an institutional experience and review of the literature. J Pediatr Hematol Oncol 35:93–97
Enomoto Y, Enomoto K, Uchino S et al (2012) Clinical features, treatment, and long-term outcome of papillary thyroid cancer in children and adolescents without radiation exposure. World J Surg 36:1241–1246
Welch Dinauer CA, Tuttle RM, Robie DK et al (1997) Clinical features associated with metastasis and recurrence of differentiated thyroid cancer in children, adolescents, and young adults. Clin Endocrinol 49:619–628
Pacini F, Elisei R, Capezzone M et al (2001) Contralateral papillary thyroid cancer is frequent at completion thyroidectomy with no difference in low- and high-risk patients. Thyroid 11:877–881
Moses W, Weng J, Khanafshar E et al (2010) Multiple genetic alterations in papillary thyroid cancer are associated with younger age at presentation. J Surg Res 160:179–183
Yamamoto Y, Maeda T, Izumi K et al (1990) Occult papillary carcinoma of the thyroid. A study of 408 autopsy cases. Cancer 65:1173–1179
Harach HR, Franssila KO, Wasenius VM (1985) Occult papillary carcinoma of the thyroid. A “normal” finding in Finland. A systematic autopsy study. Cancer 56:531–538
Robinson DW, Orr TG (1955) Carcinoma of the thyroid and other diseases of the thyroid in identical twins. Arch Surg 70:923–928
Nosé V (2011) Familial thyroid cancer: a review. Mod Pathol 24:19–33
Uchino S, Noguchi S, Kawamoto H et al (2002) Familial nonmedullary thyroid carcinoma characterized by multifocality and high recurrence rate in a large population. World J Surg 26:897–902
Capezzone M, Marchisotta S, Cantara S et al (2008) Familial nonmedullary thyroid carcinoma displays the features of clinical anticipation suggestive of a distinct biological entity. Endocr-Relat Cancer 15:1075–1081
McDonald TJ, Driedger AA, Garcia BM et al (2011) Familial papillary thyroid carcinoma: a retrospective analysis. J Oncol 10:1–8
Musholt TJ, Musholt PB, Petrich T et al (2000) Familial papillary thyroid carcinoma: genetics, criteria for diagnosis, clinical features, and surgical treatment. World J Surg 24:1409–1417
Loh KC (1997) Familial nonmedullary thyroid carcinoma: a meta-review of case series. Thyroid 7:107–113
Alsanea O, Wada N, Ain K et al (2000) Is familial nonmedullary thyroid carcinoma more aggressive than sporadic thyroid cancer? A multicenter series. Surgery 128:1043–1050
Sippel RS, Caron NR, Clark OH (2007) An evidence-based approach to familial nonmedullary thyroid cancer: screening, clinical management, and follow-up. World J Surg 31:924–933
Hildebrand A, Varhaug JE, Brauckhoff M et al (2010) Familial nonmedullary thyroid carcinoma—clinical relevance and prognosis. A European multicenter study. Langenbeck’s Arch Surg 395:851–858
Pitt SC, Sippel RS, Chen H (2009) Contralateral papillary thyroid cancer: does size matter? Am J Surg 197:342–347
Cooper DS, Doherty GM, Haugen BR et al (2006) Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16:1–33
Pacini F, Schlumberger M, Dralle H et al (2006) European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol 154:787–803
Baudin E, Travagli JP, Ropers J et al (1998) Microcarcinoma of the thyroid gland. Cancer 83:553–559
Davies L, Welsh HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295:2164–2167
Piersanti M, Ezzat S, Asa S (2003) Controversies in papillary microcarcinoma of the thyroid. Endocr Pathol 14:183–191
Hay ID, Hutchinson ME, Gonzalez-Losada T et al (2008) Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery 144:980–988
Ricci JA, Alfonso AE (2012) Multifocal micropapillary thyroid cancer: a new indication for total thyroidectomy? Am Surg 78:1211–1214
He Q, Zhuang D, Zheng L et al (2012) The surgical management of papillary thyroid microcarcinoma: a 162-month single-center experience of 273 cases. Am Surg 78:1215–1218
Pellegriti G, Scollo C, Lumera G et al (2004) Clinical behavior and outcome of papillary thyroid cancers smaller than 1.5 cm in diameter: study of 299 cases. J Clin Endocrinol Metab 89:3713–3720
Lombardi CP, Bellantone R, De Crea C et al (2010) Papillary thyroid microcarcinoma: extrathyroidal extension, lymph node metastases, and risk factors for recurrence in a high prevalence of goiter area. World J Surg 34:1214–1221
Vasileiadis I, Karakostas E, Charitoudis G et al (2012) Papillary thyroid microcarcinoma: clinicopathological characteristics and implications for treatment in 276 patients. Eur J Clin Investig 42:657–664
Zhou YL, Gao EL, Zhang W et al (2012) Factors predictive of papillary thyroid microcarcinoma with bilateral involvement and central lymph node metastasis: a retrospective study. World J Surg Oncol 10:67–72
Zhang L, Wei W-J, Ji Q-H et al (2012) Risk factors for neck nodal metastasis in papillary thyroid microcarcinoma: a study of 1,066 patients. J Clin Endocrinol Metab 97:1250–1257
Ross DS, Litofsky D, Ain KB et al (2009) Recurrence after treatment of micropapillary thyroid cancer. Thyroid 19:1043–1048
Neuhold N, Schultheis A, Hermann M et al (2011) Incidental papillary microcarcinoma of the thyroid—further evidence of very low malignant potential: a retrospective clinicopathological study with up to 30 years of follow-up. Ann Surg Oncol 18:3430–3436
Zhao Q, Ming J, Liu C et al (2013) Multifocality and total tumor diameter predict central neck lymph node metastases in papillary thyroid microcarcinoma. Ann Surg Oncol 20:746–752
Chow SM, Law SC, Chan JK et al (2003) Papillary microcarcinoma of the thyroid - prognostic significance of lymph node metastasis and multifocality. Cancer 98:31–40
Schlumberger M, Travagli JP, Lemerle J et al (1987) Differentiated thyroid carcinoma in childhood. Experience at Institut Gustave-Roussy, Villejuif. Acta Otorhinolaryngol Belg 41:804–808
Leboulleux S, Rubino C, Baudin E et al (2005) Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. J Clin Endocrinol Metab 90:5723–5729
Schindler AM, van Melle G, Evequoz B et al (1991) Prognostic factors in papillary carcinoma of the thyroid. Cancer 68:324–330
Sciuto R, Romano L, Rea S et al (2009) Natural history and clinical outcome of differentiated thyroid carcinoma: a retrospective analysis of 1,503 patients treated at a single institution. Ann Oncol 20:1728–1735
Zheng X-Q, Xia T, Lin L et al (2012) BRAFV600E status and clinical characteristics in solitary and multiple papillary thyroid carcinoma: experience of 512 cases at a clinical center in China. World J Surg Oncol 10:104–110
Grigsby PW, Reddy RM, Moley JF et al (2006) Contralateral papillary thyroid cancer at completion thyroidectomy has no impact on recurrence or survival after radioiodine treatment. Surgery 140:1043–1047
Frates MC, Benson CB, Charboneau JW et al (2005) Management of thyroid nodules detected at US: society of radiologists in ultrasound consensus conference statement1. Radiology 237:794–800
Sakorafas GH, Giotakis J, Stafyla V (2005) Papillary thyroid microcarcinoma: a surgical perspective. Cancer Treat Rev 31:423–438
Choi JS, Chung WY, Kwak JY et al (2011) Staging of papillary thyroid carcinoma with ultrasonography: performance in a large series. Ann Surg Oncol 18:3572–3578
Gharib H, Goellner JR (1993) Fine-needle aspiration biopsy of the thyroid: an appraisal. Ann Intern Med 118:282–289
Bramley MD, Harrison BJ (1996) Papillary microcarcinoma of the thyroid gland. Br J Surg 83:1674–1683
Salvatore G, Giannini R, Faviana P et al (2004) Analysis of BRAF point mutation and RET/PTC rearrangements refines the fine-needle aspiration diagnosis of papillary thyroid carcinoma. J Clin Endocrinol Metab 89:5175–5180
Xing M, Tufano RP, Tufaro AP et al (2004) Detection of BRAF mutation on fine needle aspiration biopsy specimens: a new diagnostic tool for papillary thyroid cancer. J Clin Endocrinol Metab 89:2867–2872
Sapio RM, Posca D, Raggioli A et al (2007) Detection of RET/PTC, TRK, and BRAF mutations in preoperative diagnosis of thyroid nodules with indeterminate cytological findings. Clin Endocrinol (Oxf) 66:678–683
Clark OH (1982) Total thyroidectomy: the treatment of choice for patients with differentiated thyroid cancer. Ann Surg 196:361–370
Kebebew E, Clark OH (2000) Differentiated thyroid cancer: “complete” rational approach. World J Surg 24:942–951
ATA Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, Cooper DS, Doherty GM, Haugen BR et al (2009) American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214
Carty SE, Cooper DS, Doherty GM et al (2009) Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid 19:1153–1158
Lundgren CI, Hall P, Dickman PW et al (2006) Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case–control study. Cancer 106:524–531
Tisell LE, Nilsson B, Mölne J et al (1996) Improved survival of patients with papillary thyroid cancer after surgical microdissection. World J Surg 20:854–859
So YK, Son YI, Hong SD et al (2010) Subclinical lymph node metastasis in papillary thyroid microcarcinoma: a study of 551 resections. Surgery 148:526–531
Lim YC, Choi EC, Yoon YH (2009) Central lymph node metastases in unilateral papillary thyroid microcarcinoma. Br J Surg 96:253–257
Shao Y, Cai XJ, Gao L (2009) Clinical factors related to central compartment lymph node metastasis in papillary thyroid microcarcinoma: clinical analysis of 117 cases. Zhonghua Yi Xue Za Zhi 89:403–405
Xu Y, Wang J (2007) Analysis of lymph node metastasis factors in papillary thyroid microcarcinoma. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 21:679–682
Wang Y, Ji QH, Huang CP et al (2008) Predictive factors for level VI lymph node metastasis in papillary thyroid microcarcinoma. Zhonghua Yan Ke Za Zhi 46:1899–1901
Wada N, Duh QY, Sugino K et al (2003) Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 237:399–407
Ito Y, Miyauchi A (2008) Lateral lymph node dissection guided by preoperative and intraoperative findings in differentiated thyroid carcinoma. World J Surg 32:729–739
Lee SH, Lee SS, Jin SM et al (2008) Predictive factors for central compartment lymph node metastasis in thyroid papillary microcarcinoma. Laryngoscope 118:659–662
Barbaro D, Simi U, Meucci G et al (2005) Thyroid papillary cancers: microcarcinoma and carcinoma, incidental cancers and nonincidental cancers—are they different diseases? Clin Endocrinol (Oxf) 63:577–581
Page C, Biet A, Boute P et al (2009) “Aggressive papillary” thyroid microcarcinoma. Eur Arch Otorhinolaryngol 266:1959–1963
Barczynski M, Konturek A, Stopa M et al (2013) Prophylactic central neck dissection for papillary thyroid cancer. Br J Surg 100:410–418
Kim ES, Kim TY, Koh JM et al (2004) Completion thyroidectomy in patients with thyroid cancer who initially underwent unilateral operation. Clin Endocrinol (Oxf) 61:145–148
Kupferman ME, Mandel SJ, DiDonato L et al (2002) Safety of completion thyroidectomy following unilateral lobectomy for well-differentiated thyroid cancer. Laryngoscope 112:1209–1212
Dietlein M, Luyken WA, Schicha H et al (2005) Incidental multifocal papillary microcarcinomas of the thyroid: is subtotal thyroidectomy combined with radioiodine ablation enough? Nucl Med Commun 26:3–8
Sawka AM, Brierley JD, Tsang RW (2008) An updated systematic review and commentary examining the effectiveness of radioactive iodine remnant ablation in well-differentiated thyroid cancer. Endocrinol Metab Clin N Am 37:457–480
Edge SB, Byrd DR, Compton CC et al (2010) AJCC Cancer Staging Handbook: AJCC Cancer Staging Manual, 7th ed. Springer, New York
Rosario PW, Xavier AC, Calsolari MR (2011) Value of postoperative thyroglobulin and ultrasonography for the indication of ablation and 131-I activity in patients with thyroid cancer and low risk of recurrence. Thyroid 21:49–53
Nascimento C, Borget I, Al Ghuzlan A et al (2011) Persistent disease and recurrence in differentiated thyroid cancer patients with undetectable postoperative stimulated thyroglobulin level. Endocr-Relat Cancer 18:R29–R40
Hay ID, Thompson GB, Grant CS et al (2002) Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940-1999): temporal trends in initial therapy and long-term outcome in 2,444 consecutively treated patients. World J Surg 26:879–885
Buffet C, Golmard JL, Hoang C et al (2012) Scoring system for predicting recurrences in patients with papillary thyroid microcarcinoma. Eur J Endocrinol 167:267–275
Ardito G, Revelli L, Giustozzi E et al (2013) Aggressive papillary thyroid microcarcinoma: prognostic factors and therapeutic strategy. Clin Nucl Med 38:25–28
Gemsenjäger EW, Heitz PU, Schweizer I (2005) Multifocal papillary thyroid carcinoma. N Engl J Med 353:1067
Meas T, Vercellino L, Faugeron I et al (2013) The 2009 Revised American Thyroid Association Guidelines for Thyroid Cancer: multifocality in T1 tumors in question, for or against a more minimalist approach? Thyroid 23:1042–1043
Cailleux AF, Baudin E, Travagli JP et al (2000) Is diagnostic iodine-131 scanning useful after total thyroid ablation for differentiated thyroid cancer? J Clin Endocrinol Metab 85:175–178
Bachelot A, Cailleux AF, Klain M et al (2002) Relationship between tumor burden and serum thyroglobulin level in patients with papillary and follicular thyroid carcinoma. Thyroid 12:707–711
Mercante G, Frasoldati A, Pedroni C et al (2009) Prognostic factors affecting neck lymph node recurrence and distant metastasis in papillary microcarcinoma of the thyroid: results of a study in 445 patients. Thyroid 19:707–716
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper was partly presented and discussed at the workshop “Surgery of Thyroid Cancer” organized by the European Society of Endocrine Surgeons (Berlin, Germany, May 23–25, 2013).
Rights and permissions
About this article
Cite this article
Iacobone, M., Jansson, S., Barczyński, M. et al. Multifocal papillary thyroid carcinoma—a consensus report of the European Society of Endocrine Surgeons (ESES). Langenbecks Arch Surg 399, 141–154 (2014). https://doi.org/10.1007/s00423-013-1145-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-013-1145-7