Abstract
Introduction
The Sequential Organ Failure Assessment (SOFA) score has been applied for the prediction of survival in critically ill patients. We analysed the value of the SOFA score for the prediction of short-term survival after liver transplantation in high-risk liver transplant recipients with a labMELD score ≥30.
Patients and methods
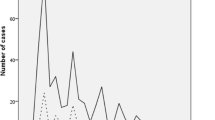
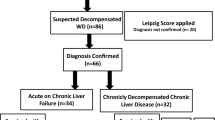
We conducted a retrospective single-centre analysis including 88 consecutive liver transplants in adults between January 1, 2007 and December 31, 2010 with a pre-transplant labMELD score ≥30. The SOFA score was assessed preoperatively, directly after transplantation and on post-operative days (PODs) 1–10. Combined and living-related liver transplants were excluded. Receiver operating characteristic (ROC) curve analysis with the Hosmer–Lemeshow test and application of the Brier score were used to calculate sensitivity, specificity, overall model correctness and calibration. Cutoff values were selected with the best Youden index.
Results
ROC curve analysis showed areas under the curve (AUROCs) >0.8 for the SOFA score on PODs 1–10 for the prediction of hospital mortality, 30-day mortality and 3-month mortality with Hosmer–Lemeshow test results that confirmed good model calibration (p > 0.05). The Brier score demonstrated an accuracy of prediction (<0.25) of hospital mortality, 30-day mortality and 3-month mortality for the SOFA scores on PODs 4–9 indicating superior accuracy on PODs 7 and 8 with cutoff values for the SOFA score between 16.5 and 18.5. The pre-transplant SOFA score failed to reach AUROCs >0.7 (0.603–0.663) for the prediction of short-term survival.
Conclusions
Our results confirm the usefulness of the SOFA score in high-risk liver recipients during the early post-operative course, especially on PODs 7–8 for the prediction of hospital mortality, 30-day mortality and 3-month mortality and may be useful to predict futile early acute retransplantation.

Similar content being viewed by others
References
Adam R, Hoti E (2009) Liver transplantation: the current situation. Semin Liver Dis 29(1):3–18, Epub 2009 Feb 23
Bahra M, Neuhaus P (2011) Liver transplantation in the high MELD era: a fair chance for everyone? Langenbecks Arch Surg 396:461–465
Schlitt HJ, Loss M, Scherer MN, Becker T, Jauch KW, Nashan B, Schmidt H et al (2011) Current developments in liver transplantation in Germany: MELD-based organ allocation and incentives for transplant centres. Z Gastroenterol 49(1):30–38, Epub 2011 Jan 10. German
Foxton MR, Al-Freah MA, Portal AJ, Sizer E, Bernal W, Auzinger G, Rela M et al (2010) Increased model for end-stage liver disease score at the time of liver transplant results in prolonged hospitalization and overall intensive care unit costs. Liver Transpl 16(5):668–677
Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC (2000) A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31(4):864–871
Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, Kremers W, United Network for Organ Sharing Liver Disease Severity Score Committee et al (2003) Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 124(1):91–96
Asrani SK, Kim WR (2010) Organ allocation for chronic liver disease: model for end-stage liver disease and beyond. Curr Opin Gastroenterol 26(3):209–213, Review
Washburn K, Edwards E, Harper A, Freeman R (2010) Hepatocellular carcinoma patients are advantaged in the current liver transplant allocation system. Am J Transplant 10(7):1643–1648, Epub 2010 May 10
Jung GE, Encke J, Schmidt J, Rahmel A (2008) Model for end-stage liver disease. New basis of allocation for liver transplantations. Chirurg 79(2):157–163, Article in German
Weismüller TJ, Negm A, Becker T, Barg-Hock H, Klempnauer J, Manns MP, Strassburg CP (2009) The introduction of MELD-based organ allocation impacts 3-month survival after liver transplantation by influencing pretransplant patient characteristics. Transpl Int 22(10):970–978
Onaca NN, Levy MF, Sanchez EQ, Chinnakotla S, Fasola CG, Thomas MJ, Weinstein JS et al (2003) A correlation between the pretransplantation MELD score and mortality in the first two years after liver transplantation. Liver Transpl 9(2):117–123
Jacob M, Copley LP, Lewsey JD, Gimson A, Toogood GJ, Rela M, van der Meulen JH, UK and Ireland Liver Transplant Audit (2004) Pretransplant MELD score and post liver transplantation survival in the UK and Ireland. Liver Transpl 10(7):903–907
Feng S, Goodrich NP, Bragg-Gresham JL, Dykstra DM, Punch JD, DebRoy MA, Greenstein SM et al (2006) Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant 6(4):783–790
Yoo HY, Thuluvath PJ (2005) Short-term postliver transplant survival after the introduction of MELD scores for organ allocation in the United States. Liver Int 25(3):536–541
Island E, Pomposelli J, Pomfet E, Fabry S, Simpson M (2004) Patients with MELD scores creater than 26 have higher mortality and increased resource utilization after liver transplantation. Hepatology 40:554A
Weismüller TJ, Fikatas P, Schmidt J, Barreiros AP, Otto G, Beckebaum S, Paul A et al (2011) Multicentric evaluation of model for end-stage liver disease-based allocation and survival after liver transplantation in Germany—limitations of the ‘sickest first’-concept. Transpl Int 24(1):91–99
Cholongitas E, Betrosian A, Senzolo M, Shaw S, Patch D, Manousou P, O’Beirne J et al (2008) Prognostic models in cirrhotics admitted to intensive care units better predict outcome when assessed at 48 h after admission. J Gastroenterol Hepatol 23(8 Pt 1):1223–1227, Epub 2007 Dec 13
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK et al (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22(7):707–710
Moreno R, Vincent JL, Matos R, Mendonça A, Cantraine F, Thijs L, Takala J et al (1999) The use of maximum SOFA score to quantify organ dysfunction/failure in intensive care. Results of a prospective, multicentre study. Working Group on Sepsis related Problems of the ESICM. Intensive Care Med 25(7):686–696
Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286(14):1754–1758
Peres Bota D, Melot C, Lopes Ferreira F, Nguyen Ba V, Vincent JL (2002) The Multiple Organ Dysfunction Score (MODS) versus the Sequential Organ Failure Assessment (SOFA) score in outcome prediction. Intensive Care Med 28(11):1619–1624
Chen JS, Ko WJ, Yu HY, Lai LP, Huang SC, Chi NH, Tsai CH et al (2006) Analysis of the outcome for patients experiencing myocardial infarction and cardiopulmonary resuscitation refractory to conventional therapies necessitating extracorporeal life support rescue. Crit Care Med 34(4):950–957
Pätilä T, Kukkonen S, Vento A, Pettilä V, Suojaranta-Ylinen R (2006) Relation of the Sequential Organ Failure Assessment score to morbidity and mortality after cardiac surgery. Ann Thorac Surg 82(6):2072–2078
Lee K, Hong SB, Lim CM, Koh Y (2008) Sequential organ failure assessment score and comorbidity: valuable prognostic indicators in chronically critically ill patients. Anaesth Intensive Care 36(4):528–534
Jones AE, Trzeciak S, Kline JA (2009) The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit Care Med 37(5):1649–1654
Wong CS, Lee WC, Jenq CC, Tian YC, Chang MY, Lin CY, Fang JT et al (2010) Scoring short-term mortality after liver transplantation. Liver Transpl 16(2):138–146
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36
Minne L, Abu-Hanna A, de Jonge E (2008) Evaluation of SOFA-based models for predicting mortality in the ICU: A systematic review. Crit Care 12(6):R161, Epub 2008 Dec 17
Brier GW (1950) Verification of forecasts expressed in terms of probability. Mon Weather Rev 78:1–3
Arkes HR, Dawson NV, Speroff T, Harrell FE Jr, Alzola C, Phillips R, Desbiens N et al (1995) The covariance decomposition of the probability score and its use in evaluating prognostic estimates. SUPPORT Investigators. Med Decis Making 15(2):120–131
Redelmeier DA, Bloch DA, Hickam DH (1991) Assessing predictive accuracy: how to compare Brier scores. J Clin Epidemiol 44(11):1141–1146
Youden WJ (1950) Index for rating diagnosis tests. Cancer 3:32–35
Acknowledgements
The authors would like to thank Dr. Hoy, Department of Biometry at the Medizinische Hochschule Hannover for his support and critical review of the manuscript.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Harald Schrem and Melanie Reichert contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Schrem, H., Reichert, M., Reichert, B. et al. Value of the SOFA score as a predictive model for short-term survival in high-risk liver transplant recipients with a pre-transplant labMELD score ≥30. Langenbecks Arch Surg 397, 717–726 (2012). https://doi.org/10.1007/s00423-011-0881-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-011-0881-9