Abstract
Introduction
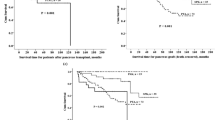
Simultaneous pancreas–kidney (SPK) transplantation is state-of-the-art therapy for patients with type-1 diabetes mellitus and end-stage renal failure. Improvement of long-term organ function and long-term survival after transplantation is the main focus of current research, but improvement of the early postoperative course is very important for the patient. Pancreas transplantation is associated with postoperative complications. We defined and identified donor- and recipient-specific factors related to postoperative complications.
Patients and methods
We carried out 210 SPKs from April 1995 to December 2007. The early postoperative course until first discharge from hospital was analyzed. Complications (pancreas-specific and surgical) were revisited. Donor-specific factors such as sex, age, body mass index (BMI), laboratory values, catecholamine administration, time in the intensive care unit, preprocurement blood substitution, and asystolic periods, as well as factors related to the organ donation procedure, were assessed. Recipient-specific factors such as age, sex, BMI, and blood group were correlated with the prevalence of complications and postoperative outcome.
Donor-specific risk factors correlating with postoperative complications included donor age, BMI, and blood transfusion in the donor before organ donation.
Results
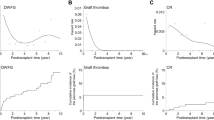
Graft preservation with histidine–tryptophan–ketoglutarate perfusion solution was related to a significantly higher number of surgical complications.When analyzing recipient-specific factors, pre-existing cardiac diseases influenced the prevalence of postoperative complications.
The duration of the transplantation procedure was associated with significantly more complications. The anastomosis time was not significantly related to an increased prevalence of complications.
The choice of immunosuppression had a significant effect on pancreas-specific complications, demonstrating that antithymocyte globulin instead of daclizumab had a negative effect. Initial immunosuppression with tacrolimus combined with mycophenolate mofetil (MMF) caused significantly fewer pancreas-related complications in comparison with tacrolimus combined with rapamycin as well as compared with cyclosporine combined with MMF. A high level of C-reactive protein within the first 7 days after transplantation was significantly related to an increased prevalence of complications.
Conclusions
Early postoperative complications after combined pancreas–kidney transplantation have a considerable effect on short- and long-term outcomes. Several statistically relevant factors related to pancreas- or surgery-associated complications could be identified. These data may help to improve early outcome after SPK by consideration of relevant risk factors when choosing an organ and a recipient for transplantation.
Similar content being viewed by others
References
Szmidt J, Grochowiecki T, Galazka Z et al (2006) Influence of pancreas and kidney transplant function on recipient survival. Transplant Proc 38(1):263
Gruessner AC, Sutherland DE (2005) Pancreas transplant outcomes for United States (US) and non-US cases as reported to the United Network for Organ Sharing (UNOS) and the International Pancreas Transplant Registry (IPTR) as of June 2004. Clin Transplant 19(4):433
Leichtman AB, Cohen D, Keith D et al (2008) Kidney and pancreas transplantation in the United States, 1997–2006: the HRSA breakthrough collaboratives and the 58 DSA challenge. Am J Transplant 8(4p2):946
Fioretto P, Steffes MW, Sutherland DE, Goetz FC, Mauer M (1998) Reversal of lesions of diabetic nephropathy after pancreas transplantation. N Engl J Med 339(2):69
Humar A, Kandaswamy R, Granger D, Gruessner RW, Gruessner AC, Sutherland DE (2000) Decreased surgical risks of pancreas transplantation in the modern era. Ann Surg 231(2):269
Navarro A, Castro MJ, Cabello M et al (2006) Outcome and morbidity of pancreas transplantation in a single Spanish institution. Transplant Proc 38(5):1543
Sureshkumar KK, Patel BM, Markatos A, Nghiem DD, Marcus RJ (2006) Quality of life after organ transplantation in type 1 diabetics with end-stage renal disease. Clin Transplant 20(1):19
Malaise J, Steurer W, Koenigsrainer A et al (2005) Simultaneous pancreas–kidney transplantation in a large multicenter study: surgical complications. Transplant Proc 37(6):2859
Salvalaggio PR, Schnitzler MA, Abbott KC et al (2007) Patient and graft survival implications of simultaneous pancreas kidney transplantation from old donors. Am J Transplant 7(6):1561
Schenker P, Wunsch A, Ertas N et al (2008) Long-term results after simultaneous pancreas–kidney transplantation using donors aged 45 years or older. Transplant Proc 40(4):923
Vinkers MT, Rahmel AO, Slot MC, Smits JM, Schareck WD (2008) How to recognize a suitable pancreas donor: a Eurotransplant study of preprocurement factors. Transplant Proc 40(5):1275
Kwiatkowski A, Michalak G, Czerwinski J et al (2005) Quality of life after simultaneous pancreas–kidney transplantation. Transplant Proc 37(8):3558
Sansalone CV, Maione G, Aseni P et al (2005) Surgical complications are the main cause of pancreatic allograft loss in pancreas–kidney transplant recipients. Transplant Proc 37(6):2651
Schäffer M, Bartmann V, Wunsch A et al (2007) Kombinierte nieren-pankreas-transplantation. Der Chirurg 78(10):928
Wullstein C, Woeste G, de Vries E, Persijn GG, Bechstein WO (2005) Acceptance criteria of pancreas grafts: how do surgeons decide in Europe? Transplant Proc 37(2):1259
Stratta RJ (2005) Surgical nuances in pancreas transplantation. Transplant Proc 37(2):1291
Krieger NR, Odorico JS, Heisey DM et al (2003) Underutilization of pancreas donors. Transplantation 75(8):1271
Waanders MM, Roelen DL, de Fijter JW et al (2008) Protocolled blood transfusions in recipients of a simultaneous pancreas–kidney transplant reduce severe acute graft rejection. Transplantation 85(11):1668
Schulz T, Flecken M, Schenker P, Schäffer M, Viebahn R, Kapischke M (2005) Pankreasorganentnahme durch externe teams. Der Chirurg 76(6):581
Baertschiger RM, Berney T, Morel P (2008) Organ preservation in pancreas and islet transplantation. Curr Opin Organ Transpl 13(1):59
Becker T, Ringe B, Nyibata M et al (2007) Pancreas transplantation with histidine–tryptophan–ketoglutarate (HTK) solution and University of Wisconsin (UW) solution: is there a difference? Jop 8(3):304
Fellmer P, Lanzenberger K, Ulrich F et al (2007) Complication rate of pancreas retransplantation after simultaneous pancreas–kidney transplantation compared with pancreas after kidney transplantation. Transplant Proc 39(2):563
Gruessner RW, Dunn DL, Gruessner AC, Matas AJ, Najarian JS, Sutherland DE (1994) Recipient risk factors have an impact on technical failure and patient and graft survival rates in bladder-drained pancreas transplants. Transplantation 57(11):1598
Schaffer M, Wunsch A, Michalski S, Traska T, Schenker P, Viebahn R (2007) Morbidity and mortality of kidney and pancreas transplantation. Analysis of 810 transplantations at one center. Dtsch Med Wochenschr 132(44):2318
Berger N, Wirmsberger R, Kafka R et al (2006) Infectious complications following 72 consecutive enteric-drained pancreas transplants. Transpl Int 19(7):549
van de Linde P, van der Boog PJM, Baranski AG, de Fijter JW, Ringers J, Schaapherder AFM (2006) Pancreas transplantation: advantages of both enteric and bladder drainage combined in a two-step approach. Clin Transpl 20(2):253
Ming CS, Chen ZH (2007) Progress in pancreas transplantation and combined pancreas–kidney transplantation. Hepatobiliary Pancreat Dis Int 6(1):17
Gallon LG, Winoto J, Chhabra D, Parker MA, Leventhal JR, Kaufman DB (2007) Long-term renal transplant function in recipient of simultaneous kidney and pancreas transplant maintained with two prednisone-free maintenance immunosuppressive combinations: tacrolimus/mycophenolate mofetil versus tacrolimus/sirolimus. Transplantation 83(10):1324
Wullstein C, Drognitz O, Woeste G et al (2004) High levels of C-reactive protein after simultaneous pancreas–kidney transplantation predict pancreas graft-related complications and graft survival. Transplantation 77(1):60
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fellmer, P.T., Pascher, A., Kahl, A. et al. Influence of donor- and recipient-specific factors on the postoperative course after combined pancreas–kidney transplantation. Langenbecks Arch Surg 395, 19–25 (2010). https://doi.org/10.1007/s00423-009-0552-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-009-0552-2