Abstract
Background and aims
Surgical resection is the treatment of choice for carotid body tumors. The aim of this study was to assess not only the perioperative, but also the long-term outcome after surgical treatment.
Patients/methods
All patients that were operated on a carotid body tumor at our institution between 1986 and 2006 were reviewed. Data collection included patient profile, intraoperative findings and postoperative outcome.
Results
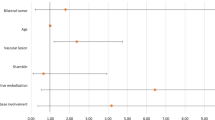
Seventeen patients (11 female, six male) with 17 carotid body tumors (12 right, five left sided) were identified. Mean patient age at treatment was 49 years (range 19 to 76 years). Eight patients (47.1%) had large Shamblin type III tumors. Complete tumor resection was achieved in 16 of 17 cases (94.1%). Malignacy could not be proven in any patient. The 30-day mortality and stroke rates were 0. The incidence of temporary and permanent cranial nerve deficit was 41.2% and 11.8%, respectively. Patients with type III tumors had significantly higher risk of neurologic complications than patients with smaller tumors (p = 0.0152). The median postoperative follow-up was 6.4 years (range 1.5 to 20 years). The overall survival rate was 82.4%; the disease-specific survival rate was 94.1% (16 of 17 patients). One patient (5.6%) died of local tumor recurrence 3 years after a R1 resection. All the other patients showed no signs of local recurrence or metastases.
Conclusions
The surgical therapy of carotid body tumors shows low long-term morbidity, mortality, and recurrence rates. Cranial nerve injury is mostly temporary but a relevant procedure-related complication. Surgical resection is indicated also for small, asympomatic tumors, because of the uncomplicated resectability of these tumors.





Similar content being viewed by others
References
Sajid MS, Hamilton G, Baker DM (2007) A multicenter review of carotid body tumour management. Eur J Vasc Endovasc Surg 34:127–130 doi:10.1016/j.ejvs.2007.01.015
Shamblin WR, ReMine WH, Sheps SG, Harrison EG Jr (1971) Carotid body tumor (chemodectoma): clinicopathologic analysis of ninety cases. Am J Surg 122:732–739 doi:10.1016/0002-9610(71)90436-3
Linder F, Wagner M, Allenberg JR, Koffler M (1984) Tumoren des Glomus caroticum. Chirurg 55:19–24
Westerband A, Hunter GC, Cintora I, Gentile AT, Devine J, Mills JL (1998) Current trends in the detection and management of carotid body tumour. J Vasc Surg 1:84–92 doi:10.1016/S0741-5214(98)70203-4
Chambers RG, Mahoney WD (1968) Carotid body tumors. Am J Surg 116:554–558 doi:10.1016/0002-9610(68)90392-9
Gaylis H, Mieny CJ (1977) The incidence of malignancy in carotid body tumours. Br J Surg 64:885–889 doi:10.1002/bjs.1800641214
Parry DM, Li FP, Strong LC, Carney JA, Schoffenfeld D, Reimer RR et al (1982) Carotid body tumours in humans: genetics and epidemiology. J Natl Cancer Inst 68:573–578
Staats EF, Brown RL, Smith RR (1966) Carotid body tumors, benign and malignant. Laryngoscope 76:907–916 doi:10.1288/00005537-196605000-00008
Lees CD, Levine HL, Beven EG, Tucker HM (1981) Tumors of the carotid body: experience with 41 operative cases. Am J Surg 142:362–365 doi:10.1016/0002-9610(81)90349-4
Rangwala AF, Sylvia LC, Becker SM (1978) Soft tissue metastases of a chemodectoma: a case report and review of the literature. Cancer 42:2865–2869 doi:10.1002/1097-0142(197812)42:6<2865::AID-CNCR2820420648>3.0.CO;2-Y
Romanski R (1954) Chemodectoma (non-chromaffinic paraganglioma) of the carotid body with distant metastases with illustrative case. Am J Pathol 30:1–13
Irons GB, Weiland LH, Brown WL (1977) Paragangliomas of the neck: clinical and pathologic analysis of 116 cases. Surg Clin North Am 57:575–583
Grufferman S, Gillman AB, Pasternak LR, Peterson CL, Young WG Jr (1980) Familial carotid body tumors: case report and epidemiologic review. Cancer 46:2116–2122 doi:10.1002/1097-0142(19801101)46:9<2116::AID-CNCR2820460934>3.0.CO;2-S
Lawson W (1980) Glomus bodies and tumors. N Y State J Med 80:1567–1575
Hallett JW Jr, Nora JD, Hollier LH, Cherry KJ Jr, Pairolero PC (1988) Trends in neurovascular complications of surgical management for carotid body and cervical paragangliomas: a 50-year experience with 153 tumors. J Vasc Surg 7:284–291 doi:10.1067/mva.1988.avs0070284
Davidge-Pitts KJ, Pantanowitz D (1984) Carotid body tumors. Surg Annu 16:203–227
Padberg FT Jr, Cady B, Persson AV (1983) Carotid body tumor: the Lahey Clinic experience. Am J Surg 145:526–528 doi:10.1016/0002-9610(83)90052-1
Dockerty MB, Love JG, Patton MM (1951) Non-chromaffin paraganglioma of the middle ear: report of a case in which the clinical aspects were those of a brain tumor. Proc Staff Meet Mayo Clin 26:25–32
Crowell WT, Grizzle WE, Siegel AL (1982) Functional carotid paragangliomas: biomedical, ultrastructural, and histochemical correlation with clinical symptoms. Arch Pathol Lab Med 106:599–603
Glenner GG, Crout JR, Roberts WC (1962) A functional carotid body-like tumor secreting levarterenol. Arch Pathol 73:230–240
Worsey MJ, Laborde AL, Bower T, Miller E, Kresowik TF, Sharp WJ et al (1992) A evaluation of color duplex scanning in the primary diagnosis and management of carotid body tumors. Ann Vasc Surg 6:90–94 doi:10.1007/BF02000675
Olsen WL, Dillon WP, Kelly WM, Norman D, Brant-Zawadzki M, Newton TH (1987) MR imaging of paragangliomas. AJR Am J Roentgenol 148:201–204
Martinez SA, Oller DW, Gee W, deFries HO (1975) Elective carotid artery resection. Arch Otolaryngol 101:744–747
Krupski WC (2006) Carotid body tumors. In: Rutherford RB (ed) Vascular surgery. 6th edn. WB Saunders, Philadelphia, pp 2066–2073
Luna-Ortiz K, Rascon-Ortiz M, Granados-Garcia M, Herrera-Gomez A (2005) Carotid body tumours: review of a 20 years experience. Oral Oncol 1:56–61 doi:10.1016/j.oraloncology.2004.06.006
Patetsios P, Gable GR, Garrett WV, Talkington CM, Thompson JE (2002) Management of carotid body paragangliomas and review of a 30-year experience. Ann Vasc Surg 3:331–338 doi:10.1007/s10016-001-0106-8
Dardik A, Eisele DW, Williams GM, Perler BA (2002) A contemporary assessment of carotid body tumour surgery. Vasc Endovascular Surg 4:277–283 doi:10.1177/153857440203600405
Plukker JT, Brongers EP, Vermey A, Krikke A, Van Den Dungen JJ (2001) Outcome of surgical treatment for carotid body paraganglioma. Br J Surg 10:1382–1386 doi:10.1046/j.0007-1323.2001.01878.x
Wang SJ, Wang MB, Barauskas TM, Calcaterra TC (2000) Surgical management of carotid body tumours. Otolaryngol Head Neck Surg 3:202–206 doi:10.1067/mhn.2000.106709
Torres Patiño F, Gómez Acosta F, Guzmán Patraca C, Mendoza Parada J, Labastida Almedaro S (1991) Carotid body tumour. Analysis of 96 cases. Rev Invest Clin 43:119–123
Dickinson PH, Griffin SM, Guy AJ, McNeill IF (1986) Carotid body tumour: 30 years experience. Br J Surg 1:14–16 doi:10.1002/bjs.1800730107
Effeney DJ, Ehrenfeld WK, Stoney RJ (1982) Cervical chemodectoma: technical considerations and management options. Am J Surg 144:215–220 doi:10.1016/0002-9610(82)90511-6
Litle VR, Reilly LM, Ramos TK (1996) Preoperative embolization of carotid body tumors: when is it appropriate. Ann Vasc Surg 10:464–468 doi:10.1007/BF02000594
Martin CE, Rosenfeld L, McSwain B (1973) Carotid body tumors: a 16-year follow-up of seven malignant cases. South Med J 66:1236–1243
Monro RS (1950) Natural history of carotid body tumors and their diagnosis and treatment. Br J Surg 37:445–453 doi:10.1002/bjs.18003714805
Schild SE, Foote RL, Buskirk S, Robinow JS, Bock FF, Cupps RE et al (1992) Results of radiotherapy for chemodectomas. Mayo Clin Proc 67:537–540
Zabel A, Milker-Zabel S, Huber P, Schulz-Ertner D, Schlegel W, Wannenmacher M et al (2004) Fractionated stereotactic conformal radiotherapy in the management of large chemodectomas of the skull base. Int J Radiat Oncol Biol Phys 58:1445–1450 doi:10.1016/j.ijrobp.2003.09.070
Acknowledgements
The authors thank Mrs. S. Schwab for her assistance in data collection, Mr. D. Fischer for the drawings, and Mr. U. Hinz for his help with the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented at the Annual Scientific Congress of the German, Swiss and Austrian Societies for Vascular Surgery, Basel Switzerland, September 2007.
Rights and permissions
About this article
Cite this article
Kotelis, D., Rizos, T., Geisbüsch, P. et al. Late outcome after surgical management of carotid body tumors from a 20-year single-center experience. Langenbecks Arch Surg 394, 339–344 (2009). https://doi.org/10.1007/s00423-008-0378-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-008-0378-3