Abstract
Purpose
To assess whether night-time increases in mechanical loading negatively impact respiratory muscle function in COPD and whether compensatory increases in inspiratory neural drive (IND) are adequate to stabilize ventilatory output and arterial oxygen saturation, especially during sleep when wakefulness drive is withdrawn.
Methods
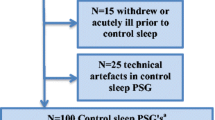
21 patients with moderate-to-severe COPD and 20 age-/sex-matched healthy controls (CTRL) participated in a prospective, cross-sectional, one-night study to assess the impact of COPD on serial awake, supine inspiratory capacity (IC) measurements and continuous dynamic respiratory muscle function (esophageal manometry) and IND (diaphragm electromyography, EMGdi) in supine sleep.
Results
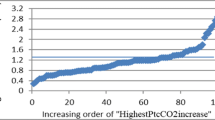
Supine inspiratory effort and EMGdi were consistently twice as high in COPD versus CTRL (p < 0.05). Despite overnight increases in awake total airways resistance and dynamic lung hyperinflation in COPD (p < 0.05; not in CTRL), elevated awake EMGdi and respiratory effort were unaltered in COPD overnight. At sleep onset (non-rapid eye movement sleep, N2), EMGdi was decreased versus wakefulness in COPD (− 43 ± 36%; p < 0.05) while unaffected in CTRL (p = 0.11); however, respiratory effort and arterial oxygen saturation (SpO2) were unchanged. Similarly, in rapid eye movement (stage R), sleep EMGdi was decreased (− 38 ± 32%, p < 0.05) versus wakefulness in COPD, with preserved respiratory effort and minor (2%) reduction in SpO2.
Conclusions
Despite progressive mechanical loading overnight and marked decreases in wakefulness drive, inspiratory effort and SpO2 were well maintained during sleep in COPD. Preserved high inspiratory effort during sleep, despite reduced EMGdi, suggests continued (or increased) efferent activation of extra-diaphragmatic muscles, even in stage R sleep.
Clinical trial information
The COPD data reported herein were secondary data (Placebo arm only) obtained through the following Clinical Trial: “Effect of Aclidinium/Formoterol on Nighttime Lung Function and Morning Symptoms in Chronic Obstructive Pulmonary Disease” (https://clinicaltrials.gov/ct2/show/NCT02429765; NCT02429765).




Similar content being viewed by others
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Abbreviations
- R AW :
-
Airway resistance
- CO2 :
-
Carbon dioxide
- COPD:
-
Chronic obstructive pulmonary disease
- ECG:
-
Electrocardiography
- EELV:
-
End-expiratory lung volume
- EMG:
-
Electromyography
- EMGdi:
-
Diaphragmatic electromyography
- EOG:
-
Electrooculography
- EELV:
-
End-expiratory lung volume
- F B :
-
Breathing frequency
- FEV1 :
-
Forced expired volume in 1 s
- FRC:
-
Functional residual capacity
- FVC:
-
Forced vital capacity
- IC:
-
Inspiratory capacity
- ICS:
-
Inhaled corticosteroids
- IND:
-
Inspiratory neural drive
- N2:
-
Stage 2 non-rapid eye movement sleep
- NMD:
-
Neuro-mechanical dissociation
- O2 :
-
Oxygen
- Pdi:
-
Transdiaphragmatic pressure
- Pes:
-
Esophageal pressure
- P ETCO2 :
-
End-tidal partial pressure of carbon dioxide
- Pga:
-
Gastric pressure
- PFT(s):
-
Pulmonary function test(s)
- PL:
-
Placebo
- PSG:
-
Polysomnography
- Stage R Sleep:
-
Rapid eye movement stage sleep
- RV:
-
Residual volume
- TLC:
-
Total lung capacity
- VC:
-
Vital capacity
- \(\dot{V}{\text{CO}}_{2}\) :
-
Carbon dioxide production
- \(\dot{V}_{{\text{E}}}\) :
-
Minute ventilation
- \(\dot{V}{\text{O}}_{2}\) :
-
Oxygen consumption
- V T :
-
Tidal volume
References
Agusti A, Hedner J, Marin JM, Barbe F, Cazzola M, Rennard S (2011) Night-time symptoms: a forgotten dimension of COPD. Eur Respir Rev 20(121):183–194. https://doi.org/10.1183/09059180.00004311
Ballard RD, Clover CW, Suh BY (1995) Influence of sleep on respiratory function in emphysema. Am J Respir Crit Care Med 151(4):945–951. https://doi.org/10.1164/ajrccm/151.4.945
Bennett JR, Dunroy HMA, Corfield DR, Hart N, Simonds AK, Polkey MI, Morrell MJ (2004) Respiratory muscle activity during REM sleep in patients with diaphragm paralysis. Neurology 62:134–137. https://doi.org/10.1212/01.wnl.0000101719.84675.e0
Brooks SMc (1982) Surveillance for respiratory hazards in the occupational setting [American Thoracic Society]. Am Rev Respir Dis 126(5):952–956
Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Calverley PM, Lee A, Towse L, van Noord J, Witek TJ, Kelsen S (2003) Effect of tiotropium bromide on circadian variation in airflow limitation in chronic obstructive pulmonary disease. Thorax 58(10):855–860. https://doi.org/10.1136/thorax.58.10.855
Chou K-T, Chang Y-T, Chen Y-M, Su K-C, Perng D-W, Chang S-C, Shiao G-M (2011) The minimum period of polysomnography required to confirm a diagnosis of severe obstructive sleep apnoea. Respirology 16(7):1096–1102. https://doi.org/10.1111/j.1440-1843.2011.02022.x
Chuang M-L, Lin IF, Vintch JRE, Liao Y-F (2008) Predicting continuous positive airway pressure from a modified split-night protocol in moderate to severe obstructive sleep apnea-hypopnea syndrome. Intern Med 47(18):1585–1592. https://doi.org/10.2169/internalmedicine.47.1107
Collop N (2010) Sleep and sleep disorders in chronic obstructive pulmonary disease. Respiration 80(1):78–86. https://doi.org/10.1159/000258676
Crinion SJ, McNicholas WT (2014) Sleep-related disorders in chronic obstructive pulmonary disease. Expert Rev Respir Med 8(1):79–88. https://doi.org/10.1586/17476348.2014.860357
Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP (2010) Pathophysiology of sleep apnea. Physiol Rev 90(1):47–112. https://doi.org/10.1152/physrev.00043.2008
Domnik NJ, Walsted ES, Langer D (2020) Clinical utility of measuring inspiratory neural drive during cardiopulmonary exercise testing (CPET). Front Med (lausanne) 7:483. https://doi.org/10.3389/fmed.2020.00483
Domnik NJ, James MD, Scheeren RE, Ayoo GA, Taylor SM, Di Luch AT, Milne KM, Vincent SG, Phillips DB, Elbehairy AF, Crinion SJ, Driver HS, Neder JA, O’Donnell DE (2021) Deterioration of nighttime respiratory mechanics in COPD: impact of bronchodilator therapy. Chest 159(1):116–127. https://doi.org/10.1016/j.chest.2020.06.033
Engel LA, Prefaut C (1981) Cranio-caudal distribution of inspired gas and perfusion in supine man. Respir Physiol 45(1):43–53. https://doi.org/10.1016/0034-5687(81)90048-7
Eremenco S, Palsgrove A, Mocarski M, O’Donohoe P, Hareendran A (2012) Evaluating the usability of an ePRO diary for measuring COPD symptoms at night and early morning. Value Health 15(4):A73. https://doi.org/10.1016/j.jval.2012.03.401
Erwin WS, Zolov D, Bickerman HA (1966) The effect of posture on respiratory function in patients with obstructive pulmonary emphysema. Am Rev Respir Dis 94(6):865–872. https://doi.org/10.1164/arrd.1966.94.6.865
Faisal A, Alghamdi BJ, Ciavaglia CE, Elbehairy AF, Webb KA, Ora J, Neder JA, O’Donnell DE (2016) Common mechanisms of dyspnea in chronic interstitial and obstructive lung disorders. Am J Respir Crit Care Med 193(3):299–309. https://doi.org/10.1164/rccm.201504-0841OC
Fletcher EC, Gray BA, Levin DC (1983) Nonapneic mechanisms of arterial oxygen desaturation during rapid-eye-movement sleep. J Appl Physiol 54(3):632–639. https://doi.org/10.1152/jappl.1983.54.3.632
Fuhr R, Magnussen H, Sarem K, Llovera AR, Kirsten AM, Falques M, Caracta CF, Garcia GE (2012) Efficacy of aclidinium bromide 400 mug twice daily compared with placebo and tiotropium in patients with moderate to severe COPD. Chest 141(3):745–752. https://doi.org/10.1378/chest.11-0406
Geiger-Brown J, Lindberg S, Krachman S, McEvoy CE, Criner GJ, Connett JE, Albert RK, Scharf SM (2015) Self-reported sleep quality and acute exacerbations of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 10:389–397. https://doi.org/10.2147/COPD.S75840
Hareendran A, Palsgrove AC, Mocarski M, Schaefer ML, Setyawan J, Carson R, Make B (2013) The development of a patient-reported outcome measure for assessing nighttime symptoms of chronic obstructive pulmonary disease. Health Qual Life Outcomes 11:104. https://doi.org/10.1186/1477-7525-11-104
Hartman JE, Prinzen J, van Lummel RC, Ten Hacken NH (2015) Frequent sputum production is associated with disturbed night’s rest and impaired sleep quality in patients with COPD. Sleep Breath 19(4):1125–1133. https://doi.org/10.1007/s11325-014-1111-9
He BT, Lu G, Xiao SC, Chen R, Steier J, Moxham J, Polkey MI, Luo YM (2017) Coexistence of OSA may compensate for sleep related reduction in neural respiratory drive in patients with COPD. Thorax 72(3):256–262. https://doi.org/10.1136/thoraxjnl-2016-208467
Hendricks JC, Kline LR (1991) Differential activation within costal diaphragm during rapid-eye-movement sleep in cats. J Appl Physiol (1985) 70(3):1194–1200. https://doi.org/10.1152/jappl.1991.70.3.1194
Henke KG, Badr MS, Skatrud JB, Dempsey JA (1992) Load compensation and respiratory muscle function during sleep. J Appl Physiol (1985) 72(4):1221–1234. https://doi.org/10.1152/jappl.1992.72.4.1221
Hogg JC, Chu F, Utokaparch S, Woods R, Elliott WM, Buzatu L, Cherniack RM, Rogers RM, Sciurba FC, Coxson HO, Pare PD (2004) The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med 350(26):2645–2653. https://doi.org/10.1056/NEJMoa032158
Hudgel DW, Martin RJ, Capehart M, Johnson B, Hill P (1983) Contribution of hypoventilation to sleep oxygen desaturation in chronic obstructive pulmonary disease. J Appl Physiol Respir Environ Exerc Physiol 55(3):669–677. https://doi.org/10.1152/jappl.1983.55.3.669
Jensen D, O’Donnell DE, Li R, Luo YM (2011) Effects of dead space loading on neuro-muscular and neuro-ventilatory coupling of the respiratory system during exercise in healthy adults: implications for dyspnea and exercise tolerance. Respir Physiol Neurobiol 179(2–3):219–226. https://doi.org/10.1016/j.resp.2011.08.009
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545. https://doi.org/10.1093/sleep/14.6.540
Johnson MW, Remmers JE (1984) Accessory muscle activity during sleep in chronic obstructive pulmonary disease. J Appl Physiol Respir Environ Exerc Physiol 57(4):1011–1017. https://doi.org/10.1152/jappl.1984.57.4.1011
Jolley CJ, Luo YM, Steier J, Rafferty GF, Polkey MI, Moxham J (2015) Neural respiratory drive and breathlessness in COPD. Eur Respir J 45(2):355–364. https://doi.org/10.1183/09031936.00063014
Jones PW, Quirk FH, Baveystock CM, Littlejohns P (1992) A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. Am Rev Respir Dis 145(6):1321–1327. https://doi.org/10.1164/ajrccm/145.6.1321
Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N (2009) Development and first validation of the COPD assessment test. Eur Respir J 34(3):648–654. https://doi.org/10.1183/09031936.00102509
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American academy of sleep medicine clinical practice guideline. J Clin Sleep Med 13(3):479–504. https://doi.org/10.5664/jcsm.6506
Lacasse Y, Series F, Vujovic-Zotovic N, Goldstein R, Bourbeau J, Lecours R, Aaron SD, Maltais F (2011) Evaluating nocturnal oxygen desaturation in COPD–revised. Respir Med 105(9):1331–1337. https://doi.org/10.1016/j.rmed.2011.04.003
Launois C, Attali V, Georges M, Raux M, Morawiec E, Rivals I, Arnulf I, Similowski T (2015) Cortical drive to breathe during wakefulness in patients with obstructive sleep apnea syndrome. Sleep 38(11):1743–1749. https://doi.org/10.5665/sleep.5156
Luo YM, He BT, Wu YX, Yuan H, Xu J, Moxham J, Polkey M (2014) Neural respiratory drive and ventilation in patients with chronic obstructive pulmonary disease during sleep. Am J Respir Crit Care Med 190(2):227–229. https://doi.org/10.1164/rccm.201402-0302LE
Mahler DA, Weinberg DH, Wells CK, Feinstein AR (1984) The measurement of dyspnea. Contents, interobserver agreement, and physiologic correlates of two new clinical indexes. Chest 85(6):751–758. https://doi.org/10.1378/chest.85.6.751
Malhotra A, Schwartz AR, Schneider H, Owens RL, DeYoung P, Han MK, Wedzicha JA, Hansel NN, Zeidler MR, Wilson KC, Badr MS, Sleep ATSAo, Respiratory N (2018) Research priorities in pathophysiology for sleep-disordered breathing in patients with chronic obstructive pulmonary disease. An official American thoracic society research statement. Am J Respir Crit Care Med 197(3):289–299. https://doi.org/10.1164/rccm.201712-2510ST
McKenzie DK, Butler JE, Gandevia SC (2009) Respiratory muscle function and activation in chronic obstructive pulmonary disease. J Appl Physiol (1985) 107(2):621–629. https://doi.org/10.1152/japplphysiol.00163.2009
McNicholas WT, Hansson D, Schiza S, Grote L (2019) Sleep in chronic respiratory disease: COPD and hypoventilation disorders. Eur Respir Rev. https://doi.org/10.1183/16000617.0064-2019
Mead J, Loring SH (1982) Analysis of volume displacement and length changes of the diaphragm during breathing. J Appl Physiol Respir Environ Exerc Physiol 53(3):750–755. https://doi.org/10.1152/jappl.1982.53.3.750
Miravitlles M, Worth H, Soler Cataluna JJ, Price D, De Benedetto F, Roche N, Godtfredsen NS, van der Molen T, Lofdahl CG, Padulles L, Ribera A (2014) Observational study to characterise 24-hour COPD symptoms and their relationship with patient-reported outcomes: results from the ASSESS study. Respir Res 15:122. https://doi.org/10.1186/s12931-014-0122-1
Mocarski M, Hareendran A, Jen MH, Zaiser E, Make B (2014) Evaluation of the psychometric properties of the Early Morning Symptoms of COPD Instrument (EMSCI). Value Health 17:A179. https://doi.org/10.1016/j.jval.2014.03.1044
Morrell MJ, Harty HR, Adams L, Guz A (1995) Changes in total pulmonary resistance and PCO2 between wakefulness and sleep in normal human subjects. J Appl Physiol (1985) 78(4):1339–1349. https://doi.org/10.1152/jappl.1995.78.4.1339
Nadel JA, Barnes PJ (1984) Autonomic regulation of the airways. Annu Rev Med 35:451–467. https://doi.org/10.1146/annurev.me.35.020184.002315
O’Donnell DE, Laveneziana P (2007) Dyspnea and activity limitation in COPD: mechanical factors. COPD 4(3):225–236. https://doi.org/10.1080/15412550701480455
O’Donnell DE, Webb KA (2008) The major limitation to exercise performance in COPD is dynamic hyperinflation. J Appl Physiol 105(2):753–755. https://doi.org/10.1152/japplphysiol.90336.2008b
O’Donoghue FJ, Catcheside PG, Eckert DJ, McEvoy RD (2004) Changes in respiration in NREM sleep in hypercapnic chronic obstructive pulmonary disease. J Physiol 559(Pt 2):663–673. https://doi.org/10.1113/jphysiol.2004.066084
Osher WJ (1950) Change of vital capacity with the assumption of the supine position. Am J Physiol-Legacy Content 161(2):352–357. https://doi.org/10.1152/ajplegacy.1950.161.2.352
Phillipson EA (1978a) Control of breathing during sleep. Am Rev Respir Dis 118(5):909–939. https://doi.org/10.1164/arrd.1978.118.5.909
Phillipson EA (1978b) Respiratory adaptations in sleep. Annu Rev Physiol 40:133–156. https://doi.org/10.1146/annurev.ph.40.030178.001025
Price D, Small M, Milligan G, Higgins V, Gil EG, Estruch J (2013) Impact of night-time symptoms in COPD: a real-world study in five European countries. Int J Chron Obstruct Pulmon Dis 8:595–603. https://doi.org/10.2147/COPD.S48570
Redolfi S, Grassion L, Rivals I, Chavez M, Wattiez N, Arnulf I, Gonzalez-Bermejo J, Similowski T (2020) Abnormal activity of neck inspiratory muscles during sleep as a prognostic indicator in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 201(4):414–422. https://doi.org/10.1164/rccm.201907-1312OC
Ries AL, Kaplan RM, Chang J (1992) Effect of posture on arterial oxygenation in patients with chronic obstructive pulmonary disease. Respiration 59(6):317–321. https://doi.org/10.1159/000196080
Shorofsky M, Bourbeau J, Kimoff J, Jen R, Malhotra A, Ayas N, Tan WC, Aaron SD, Sin DD, Road J, Chapman KR, O’Donnell DE, Maltais F, Hernandez P, Walker BL, Marciniuk D, Kaminska M, Canadian Respiratory Research N, the Can CCRg (2019) Impaired sleep quality in COPD is associated with exacerbations: the CanCOLD cohort study. Chest. https://doi.org/10.1016/j.chest.2019.04.132
Stephenson JJ, Cai Q, Mocarski M, Tan H, Doshi JA, Sullivan SD (2015) Impact and factors associated with nighttime and early morning symptoms among patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 10:577–586. https://doi.org/10.2147/COPD.S76157
Sullivan CE, Kozar LF, Murphy E, Phillipson EA (1979) Arousal, ventilatory, and airway responses to bronchopulmonary stimulation in sleeping dogs. J Appl Physiol Respir Environ Exerc Physiol 47(1):17–25. https://doi.org/10.1152/jappl.1979.47.1.17
Tabachnik E, Muller NL, Bryan AC, Levison H (1981) Changes in ventilation and chest wall mechanics during sleep in normal adolescents. J Appl Physiol Respir Environ Exerc Physiol 51(3):557–564. https://doi.org/10.1152/jappl.1981.51.3.557
van Noord JA, Aumann JL, Janssens E, Smeets JJ, Verhaert J, Disse B, Mueller A, Cornelissen PJ (2005) Comparison of tiotropium once daily, formoterol twice daily and both combined once daily in patients with COPD. Eur Respir J 26(2):214–222. https://doi.org/10.1183/09031936.05.00140404
van Noord JA, Aumann JL, Janssens E, Verhaert J, Smeets JJ, Mueller A, Cornelissen PJ (2006) Effects of tiotropium with and without formoterol on airflow obstruction and resting hyperinflation in patients with COPD. Chest 129(3):509–517. https://doi.org/10.1378/chest.129.3.509
White JE, Drinnan MJ, Smithson AJ, Griffiths CJ, Gibson GJ (1995) Respiratory muscle activity during rapid eye movement (REM) sleep in patients with chronic obstructive pulmonary disease. Thorax 50(4):376–382. https://doi.org/10.1136/thx.50.4.376
Yan S, Kaminski D, Sliwinski P (1997) Reliability of inspiratory capacity for estimating end-expiratory lung volume changes during exercise in patients with chronic obstructive pulmonary disease. Am J Resp Crit Care Med 156(1):55–59. https://doi.org/10.1164/ajrccm.156.1.9608113
Funding
This study was supported by a Canadian Institutes of Health Research Banting Postdoctoral Fellowship (N.J. Domnik) as well as a William M Spear Endowment Fund in Pulmonary Research from the Faculty of Health Sciences at Queen’s University and an investigator-initiated grant from AstraZeneca Canada Inc (ESR-15-10942), which included the Aclidinium Bromide/Formoterol 400/12 mcg (Duaklir) and placebo inhalers used in this study. The funders had no role in study design, data collection, analysis, or interpretation. D.B. Phillips was funded by a postdoctoral fellowship from the Natural Sciences and Engineering Research Council of Canada. A.F. Elbehairy acknowledges the support of the European Respiratory Society (Fellowship LTRF 2019).
Author information
Authors and Affiliations
Contributions
NJD, JAN, HSD, and DEO’D contributed significantly to the design of the study. NJD and HSD contributed significantly to data acquisition. NJD, DBP, MDJ, RES, GAA, SMT, and ATDL contributed significantly to data analysis. All authors contributed significantly to data interpretation. NJD and DEO’D contributed significantly to drafting the work. All authors contributed to critically revising the work. All authors approved the final version of the work submitted for publication and agree to be accountable for all aspects of the work, including ensuring that any questions related to accuracy or integrity are investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethics approval
The procedures used in this study were approved by the Queen’s University Health Sciences’ Research Ethics Board (REB # 6015908).
Consent to participate
All participants provided written informed consent prior to participation in this study.
Consent to publish
Participants were made aware of future plans to publish anonymised data resulting from the study during the informed consenting process.
Additional information
Communicated by Susan Hopkins .
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Domnik, N.J., Phillips, D.B., James, M.D. et al. Compensatory responses to increased mechanical abnormalities in COPD during sleep. Eur J Appl Physiol 122, 663–676 (2022). https://doi.org/10.1007/s00421-021-04869-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-021-04869-0