Abstract
Purpose
With accelerometry, the utility to detect changes in physical activity are predicated on the assumption that walking energetics and gait mechanics do not change. The present work examined associations between changes (∆) in walking energetics, exercise self-efficacy, and several accelerometer-derived metrics.
Methods
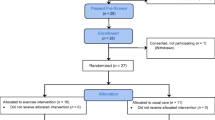
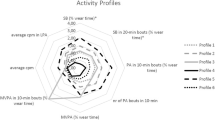
Secondary analyses were performed among a sub-sample (n = 29) of breast cancer survivors participating in a larger randomized trial. During 4 min of treadmill walking (0.89 m s−1, 0% grade), indirect calorimetry quantified steady-state energy expenditure (EE), wherein, participants were fitted with a heart rate monitor and hip-worn triaxial accelerometer. Exercise self-efficacy was measured using a 9-item questionnaire, while vector magnitude (VM) and individual planes (e.g., mediolateral, vertical, and anteroposterior) of the movement were extracted for data analyses. Evaluations were made at baseline and after 3 months.
Results
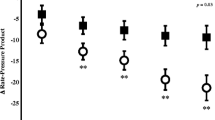
From baseline to 3 months, the energetic cost of walking (kcals min−1) significantly decreased by an average of − 5.1% (p = 0.001; d = 0.46). Conversely, VM significantly increased (p = 0.007; d = 0.53), exclusively due to greater vertical accelerations (acc) (+ 5.7 ± 7.8 acc; p = 0.001; d = 0.69). Changes in vertical accelerations were inversely and positively associated with ∆walking EE (r = − 0.37; p = 0.047) and ∆exercise self-efficacy (r = 0.39; p = 0.034), respectively.
Conclusion
Hip-worn accelerometers do not appear well-suited to correctly detect changes in ease of walking as evidenced by reduced energetic cost. Further research should determine if a divergence between measured EE and vertical accelerations could contribute to erroneous inferences in free-living physical activity.


Similar content being viewed by others
References
American College of Sports Medicine (2010) ACSM's Guidelines for Exercise Testing and Prescription. Lippincott, Williams, and Wilkins, Baltimore
Bandura A (1977) Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 84:191–215
Browning RC, Kram R (2005) Energetic cost and preferred speed of walking in obese vs. normal weight women. Obes Res 13:891–899
Browning RC, Baker EA, Herron JA, Kram R (2006) Effects of obesity and sex on the energetic cost and preferred speed of walking. J Appl Physiol 100:390–398
Carter SJ, Herron RL, Rogers LQ, Hunter GR (2016) Is 'high-intensity' a bad word? J Physiother 62:175. https://doi.org/10.1016/j.jphys.2016.05.017
Carter SJ, Hunter GR, Norian LA, Turan B, Rogers LQ (2018) Ease of walking associates with greater free-living physical activity and reduced depressive symptomology in breast cancer survivors: pilot randomized trial. Support Care Cancer 26:1675–1683. https://doi.org/10.1007/s00520-017-4015-y
Cavagna GA, Heglund NC, Taylor CR (1977) Mechanical work in terrestrial locomotion: two basic mechanisms for minimizing energy expenditure. Am J Physiol 233:R243–R261. https://doi.org/10.1152/ajpregu.1977.233.5.R243
Deimling GT, Arendt JA, Kypriotakis G, Bowman KF (2009) Functioning of older, long-term cancer survivors: the role of cancer and comorbidities. J Am Geriatr Soc 57(Suppl 2):S289–S292. https://doi.org/10.1111/j.1532-5415.2009.02515.x
Elme A, Utriainen M, Kellokumpu-Lehtinen P et al (2013) Obesity and physical inactivity are related to impaired physical health of breast cancer survivors. Anticancer Res 33:1595–1602
Goran MI, Carpenter WH, McGloin A, Johnson R, Hardin JM, Weinsier RL (1995) Energy expenditure in children of lean and obese parents. Am J Physiol 268:E917–E924. https://doi.org/10.1152/ajpendo.1995.268.5.E917
Gross AL, May BJ, Axilbund JE, Armstrong DK, Roden RB, Visvanathan K (2015) Weight change in breast cancer survivors compared to cancer-free women: a prospective study in women at familial risk of breast cancer. Cancer Epidemiol Biomarkers Prev 24:1262–1269. https://doi.org/10.1158/1055-9965.EPI-15-0212
Hall KS, Howe CA, Rana SR, Martin CL, Morey MC (2013) METs and accelerometry of walking in older adults: standard versus measured energy cost. Med Sci Sports Exerc 45:574–582. https://doi.org/10.1249/MSS.0b013e318276c73c
Hunter GR, McCarthy JP, Bamman MM, Larson-Meyer DE, Fisher G, Newcomer BR (2011) Exercise economy in African American and European American women. Eur J Appl Physiol 111:1863–1869. https://doi.org/10.1007/s00421-010-1816-9
Hunter GR, McCarthy JP, Carter SJ et al (2015) Muscle fiber type, Achilles tendon length, potentiation, and running economy. J Strength Cond Res 29:1302–1309. https://doi.org/10.1519/JSC.0000000000000760
Irwin ML, Crumley D, McTiernan A et al (2003) Physical activity levels before and after a diagnosis of breast carcinoma: the Health, Eating, Activity, and Lifestyle (HEAL) study. Cancer 97:1746–1757. https://doi.org/10.1002/cncr.11227
Ishikawa M, Komi PV (2008) Muscle fascicle and tendon behavior during human locomotion revisited. Exerc Sport Sci Rev 36:193–199. https://doi.org/10.1097/JES.0b013e3181878417
Lawler JP, White RG (2003) Temporal responses in energy expenditure and respiratory quotient following feeding in the muskox: influence of season on energy costs of eating and standing and an endogenous heat increment. Can J Zool 81:1524–1538
Lee IM, Shiroma EJ (2014) Using accelerometers to measure physical activity in large-scale epidemiological studies: issues and challenges. Br J Sports Med 48:197–201. https://doi.org/10.1136/bjsports-2013-093154
Mason C, Alfano CM, Smith AW et al (2013) Long-term physical activity trends in breast cancer survivors. Cancer Epidemiol Biomarkers Prev 22:1153–1161. https://doi.org/10.1158/1055-9965.EPI-13-0141
Middleton A, Fritz SL, Lusardi M (2015) Walking speed: the functional vital sign. J Aging Phys Act 23:314–322. https://doi.org/10.1123/japa.2013-0236
Miller KD, Siegel RL, Lin CC et al (2016) Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 66:271–289. https://doi.org/10.3322/caac.21349
Pedisic Z, Bauman A (2015) Accelerometer-based measures in physical activity surveillance: current practices and issues. Br J Sports Med 49:219–223. https://doi.org/10.1136/bjsports-2013-093407
Pinto BM, Trunzo JJ, Reiss P, Shiu SY (2002) Exercise participation after diagnosis of breast cancer: trends and effects on mood and quality of life. Psychooncology 11:389–400. https://doi.org/10.1002/pon.594
Rogers LQ, Courneya KS, Verhulst S, Markwell S, Lanzotti V, Shah P (2006) Exercise barrier and task self-efficacy in breast cancer patients during treatment. Support Care Cancer 14:84–90. https://doi.org/10.1007/s00520-005-0851-2
Rogers LQ, McAuley E, Anton PM et al (2012) Better exercise adherence after treatment for cancer (BEAT Cancer) study: rationale, design, and methods. Contemp Clin Trials 33:124–137. https://doi.org/10.1016/j.cct.2011.09.004
Rowland JH (2008) Cancer survivorship: rethinking the cancer control continuum. Semin Oncol Nurs 24:145–152. https://doi.org/10.1016/j.soncn.2008.05.002
Sawicki GS, Lewis CL, Ferris DP (2009) It pays to have a spring in your step. Exerc Sport Sci Rev 37:130–138. https://doi.org/10.1097/JES.0b013e31819c2df6
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68:7–30. https://doi.org/10.3322/caac.21442
Speck RM, Courneya KS, Masse LC, Duval S, Schmitz KH (2010) An update of controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv 4:87–100. https://doi.org/10.1007/s11764-009-0110-5
Thomas JR, Salazar W, Landers DM (1991) What is missing in p < .05? Res Q Exerc Sport 62:344–348
Troeschel AN, Leach CR, Shuval K, Stein KD, Patel AV (2018) Physical activity in cancer survivors during "re-entry" following cancer treatment. Prev Chronic Dis 15:E65. https://doi.org/10.5888/pcd15.170277
Van Remoortel H, Giavedoni S, Raste Y et al (2012) Validity of activity monitors in health and chronic disease: a systematic review. Int J Behav Nutr Phys Act 9:84. https://doi.org/10.1186/1479-5868-9-84
Acknowledgements
We would like to recognize David R. Bryan, MA, and Sara Mansfield, MS, for their commitment and respective contributions. The authors also wish to express their appreciation to the participants for their willingness to complete this investigation.
Funding
This project was supported by the following funding sources: U01CA136859, R25CA047888, and P30DK056336.
Author information
Authors and Affiliations
Contributions
SJC, LQR, HRB, LAN, and GRH participated in the execution of the study including, data analyses, drafting, review, and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Communicated by Lori Ann Vallis.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Carter, S.J., Rogers, L.Q., Bowles, H.R. et al. Inverse association between changes in energetic cost of walking and vertical accelerations in non-metastatic breast cancer survivors. Eur J Appl Physiol 119, 2457–2464 (2019). https://doi.org/10.1007/s00421-019-04227-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-019-04227-1