Abstract
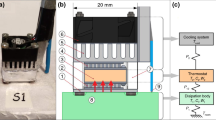
This study evaluated a zero-heat-flow (ZHF), non-invasive temperature probe for in- vivo measurement of resting muscle temperature for up to 2 cm below the skin surface. The ZHF probe works by preventing heat loss from the tissue below the probe by actively heating the tissue until no temperature gradient exists across the probe. The skin temperature under the probe is then used as an indicator of the muscle temperature below. Eight subjects sat for 130 min during exposure to 28°C air. Vastus lateralis (lateral thigh) muscle temperature was measured non-invasively using a ZHF probe which covered an invasive multicouple probe (which measured tissue temperature 0.5 cm, 1 cm, 1.5 cm, and 2 cm below the skin) located 15 cm superior to the patella (T covered). T covered was evaluated against an uncovered control multicouple probe located 20 cm superior to the patella (T uncovered). Rectal temperature and lateral thigh skin temperature were also measured. Mean T uncovered (based on average temperatures at the 0.5 cm, 1 cm, 1.5 cm, and 2 cm depths) and Mean T covered were similar from time 0 min to 60 min. However, when the ZHF was turned on at 70 min, Mean T covered increased by 2.11±0.20°C by 130 min, while T uncovered remained stable. The ZHF probe temperature was similar to T covered at 1 cm and after time 85 min, significantly higher than T covered at the 0.5 cm, 1.5 cm, and 2 cm depths; however from a physiological standpoint, the temperatures between the different depths and the ZHF probe could be considered uniform (≤0.2°C separation). Rectal and thigh skin temperatures were stable at 36.99±0.08°C and 32.82±0.23°C, respectively. In conclusion, the non-invasive ZHF probe temperature was similar to the T covered temperatures directly measured up to 2 cm beneath the surface of the thigh, but all T covered temperatures were not representative of the true muscle temperature up to 2 cm below the skin because the ZHF probe heated the muscle by 2.11±0.20°C during its operation.



Similar content being viewed by others
References
Archar S, Kundu S (2002) Principles of office anesthesia: part I. Infiltrative anesthesia. Am Fam Phys 66:91–94
Ball SG, Morgan M, Morgan AG, Solman AJ, Losowsky MS (1973) A clinical appraisal of transcutaneous deep body temperature. Biomed 18:290–294
DuBois D, DuBois EF (1916) A formula to estimate the approximate surface area if height and weight be known. Arch Intern Med 17:863–871
Ducharme MB, Frim J (1988) A multicouple probe for temperature gradient measurements in biological materials. J Appl Physiol 65:2337–2342
Fallone BG, Moran PR, Podgorsak EB (1982) Noninvasive thermometry with a clinical X-ray CT scanner. Med Phys 9:715–721
Forsyth RD, Plyley MJ, Shephard RJ (1984) Estimation of body fatness of Canadian Forces. Can J Appl Sport Sci 9:5
Fox RH, Solman AJ (1971) A new technique for monitoring the deep body temperature in man from the intact skin surface. J Physiol (Lond) 212:8P–10P
Greenleaf JF, Bahn RC (1981) Clinical imaging with transmissive ultrasonic computerized tomography. IEEE Trans Biomed Eng 28:177–185
Hand JW, Van Leeuwen GMJ, Mizushina S, Van de Kamer JB, Maruyama K, Sugiura T, Azzopardi DV, Edwards AD (2001) Monitoring of deep brain temperature in infants using multi-frequency microwave radiometry and thermal modelling. Phys Med Biol 46:1885–1903
Kenny GP, Reardon FD, Ducharme MB, Reardon ML, Zaleski W (2002a) Ultra-sound imaging for precision implantation of a multi sensor temperature probe in skeletal muscle tissue. Can J Appl Physiol 27:527–532
Kenny GP, Reardon FD, Ducharme MB, Reardon ML, Zaleski W (2002b) Tissue temperature transients in resting contra-lateral leg muscle tissue during isolated knee extension. Can J Appl Physiol 27:535–550
Kenny GP, Reardon FD, Zaleski W, Reardon ML, Haman F, Ducharme MB (2003) Muscle temperature transients before, during, and after exercise measured using an intramuscular multisensor probe. J Appl Physiol 94:2350–2357
Parker DL, Smith V, Sheldon P, Crooks LE, Fussell L (1983) Temperature distribution measurements in two-dimensional NMR imaging. Med Phys 10:321–325
Saltin B, Hermansen L (1966) Esophageal, rectal, and muscle temperature during exercise. J Appl Physiol 21:1757–1762
Saltin B, Gagge AP, Stolwijk JA (1968) Muscle temperature during submaximal exercise in man. J Appl Physiol 25:679–688
Togawa T, Nemoto T, Yamazaki T, Kobayashi T (1976) A modified internal temperature measurement device. Med Biol Eng 14:361–364
Togawa T (1979a) Deep temperature monitoring in intensive care. Resuscitation 7:53–57
Togawa T (1979b) Non-invasive deep body temperature measurement. In: Rolfe P (eds) Non-invasive pysiological measurements. Academic Press, London, pp 261–277
Tsuji T, Nakajima K, Takeuchi T, Inoue K, Shiroma K, Yamaguchi T, Koyana Y, Suma K, Togawa T (1976) Dynamic thermometry by deep body thermometer in man. Brain and Nerve 13:220–226
Yamakage M, Iwasaki S, Namiki A (2002) Evaluation of a newly developed monitor of deep body temperature. J Anesth 16:354–357
Acknowledgements
This study is a part of a U.S. Army Medical Research Acquisition Activity (USAMRAA) entitled “Body Heat Storage and Work in the Heat” under contract with the University of Ottawa. The authors would like to thank Prof. Dave T. Delpy from the Department of Medical Physics and Bioengineering at University College London, UK for supplying the zero heat flow monitoring system, and Prof. Shin-ichi Sawada from the Department of Research Planning at the National Institute of Industrial Health, Japan for allowing us to borrow his zero–heat–flow probe.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brajkovic, D., Ducharme, M.B. Confounding factors in the use of the zero-heat-flow method for non-invasive muscle temperature measurement. Eur J Appl Physiol 94, 386–391 (2005). https://doi.org/10.1007/s00421-005-1336-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-005-1336-1