Abstract
Objective
There is some evidence about the short-term effects of air pollutants on adverse pregnancy outcomes. The aim of this study was to determine the association between air pollutants and spontaneous abortion, stillbirth, gestational hypertension, preeclampsia, gestational diabetes and macrosomia in Ahvaz, which is one of the most polluted cities in the Middle East.
Methods
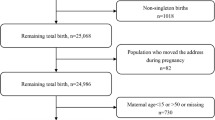
Data on adverse pregnancy outcomes and air pollutants including ozone (O3), nitric oxide (NO), nitrogen dioxide (NO2), sulfur dioxide (SO2), carbon monoxide (CO), particles with a diameter of less than 10 µm (PM10) and particles with a diameter less than 2.5 µm (PM2.5) were inquired from the Health Department of Ahvaz Jundishapur University of Medical Sciences and the Environmental Protection Agency of Khuzestan Province for the years 2008–2018. A time series analysis using the generalized additive model (GAM) with up to 6-day lags was used.
Results
The results showed that the SO2 pollutant on 0, 1, 3, 4, and 6-day lags and PM10 on lag 0 had direct and significant associations with spontaneous abortion. NO, NO2 and CO on 0–6-day lags, and O3 on 6-day lags showed direct and significant associations with preeclampsia. NO and NO2 pollutants showed significant and direct associations with gestational diabetes, during 0- and 6-day lags. NO on 0-, 3- and 4-day lags, CO in all 0–6-day lags and PM2.5 on 1-, 3-, 5-, and 6-day lags showed direct and significant associations with macrosomia. None of the pollutants showed significant associations with stillbirth or gestational hypertension.
Conclusions
The results of this study suggest that some air pollutants are associated with spontaneous abortion, preeclampsia, gestational diabetes and macrosomia. This study further emphasizes the need to control ambient air pollution.






Similar content being viewed by others

Availability of data and materials
Data sharing: participant level data are available from the corresponding author.
Change history
02 August 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00420-022-01899-9
Abbreviations
- O3 :
-
Ozone
- NO:
-
Nitric oxide
- NO2 :
-
Nitrogen dioxide
- NOx :
-
Nitrogen oxides
- SO2 :
-
Sulfur dioxide
- CO:
-
Carbon monoxide
- PM10 :
-
Particles with a diameter of less than 10 µm
- PM2.5 :
-
Particles with a diameter less than 2.5 µm
- PM:
-
Particulate matter
- WHO:
-
World Health Organization
- GAM:
-
Generalized additive model
- EM:
-
Expectation maximization
- RR:
-
Relative risk
- AIC:
-
Akaike Information Criteria
- DOW:
-
Day of the week
- CI:
-
Confidence interval
- SE:
-
Standard error
- TNF:
-
Tumor necrosis factor
References
Abdolahnejad A, Jafari N, Mohammadi A, Miri M, Hajizadeh Y, Nikoonahad A (2017) Cardiovascular, respiratory, and total mortality ascribed to PM10 and PM2. 5 exposure in Isfahan, Iran. J Educ Health Promot 6:1–6
Abramowicz JS, Ahn JT (2018) Fetal macrosomia. UptoDate, literature review current through
Achilleos S, Kioumourtzoglou M-A, Wu C-D, Schwartz JD, Koutrakis P, Papatheodorou SI (2017) Acute effects of fine particulate matter constituents on mortality: A systematic review and meta-regression analysis. Environ Int 109:89–100
Alimadad A, Salibian-Barrera M (2011) An outlier-robust fit for generalized additive models with applications to disease outbreak detection. J Am Stat Assoc 106(494):719–731
Allen RW et al (2013) An assessment of air pollution and its attributable mortality in Ulaanbaatar, Mongolia. Air Qual Atmos Health 6(1):137–150
Alsammani MA, Ahmed SR (2012) Fetal and maternal outcomes in pregnancies complicated with fetal macrosomia. N Am J Med Sci 4(6):283
Ananth CV, Basso O (2010) Impact of pregnancy-induced hypertension on stillbirth and neonatal mortality in first and higher order births: a population-based study. Epidemiology (Cambridge, Mass) 21(1):118
Arroyo V, Díaz J, Carmona R, Ortiz C, Linares C (2016) Impact of air pollution and temperature on adverse birth outcomes: Madrid, 2001–2009. Environ Pollut 218:1154–1161
Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B (2013) Time series regression studies in environmental epidemiology. Int J Epidemiol 42(4):1187–1195
Bonzini M, Carugno M, Grillo P, Mensi C, Bertazzi P, Pesatori AC (2010) Impact of ambient air pollution on birth outcomes: systematic review of the current evidences. La Medicina del lavoro 101(5):341–363
Breitner S, Wolf K, Peters A, Schneider A (2014) Short-term effects of air temperature on cause-specific cardiovascular mortality in Bavaria, Germany. Heart 100(16):1272–1280
Cai Y et al (2016) Associations of short-term and long-term exposure to ambient air pollutants with hypertension: a systematic review and meta-analysis. Hypertension 68(1):62–70
Calderon-Garciduenas L et al (2008) Systemic inflammation, endothelial dysfunction, and activation in clinically healthy children exposed to air pollutants. Inhalation Toxicol 20(5):499–506
Chen H et al (2013) Risk of incident diabetes in relation to long-term exposure to fine particulate matter in Ontario, Canada. Environ Health Perspec 121(7):804–810
Choe S-A, Jun Y-B, Kim S-Y (2018) Exposure to air pollution during preconceptional and prenatal periods and risk of hypertensive disorders of pregnancy: a retrospective cohort study in Seoul, Korea. BMC Pregnancy Childb 18(1):340
Dadvand P et al (2014) Particulate air pollution and preeclampsia: a source-based analysis. Occup Environ Med 71(8):570–577
Dastoorpoor M, Idani E, Goudarzi G, Khanjani N (2018) Acute effects of air pollution on spontaneous abortion, premature delivery, and stillbirth in Ahvaz, Iran: a time-series study. Environ Sci Pollut Res 25(6):5447–5458
Dastoorpoor M, Sekhavatpour Z, Masoumi K et al (2019) Air pollution and hospital admissions for cardiovascular diseases in Ahvaz, Iran. Sci Total Environ 652:1318–1330
DeFranco E et al (2015) Air pollution and stillbirth risk: exposure to airborne particulate matter during pregnancy is associated with fetal death. PLoS ONE 10(3):e0120594
Dehghan A, Khanjani N, Bahrampour A, Goudarzi G, Yunesian M (2018) The relation between air pollution and respiratory deaths in Tehran, Iran-using generalized additive models. BMC Pulm Med 18(1):49
Dollberg S, Fainaru O, Mimouni FB, Shenhav M, Lessing JB, Kupferminc M (2000) Effect of passive smoking in pregnancy on neonatal nucleated red blood cells. Pediatrics 106(3):E34
Dominici F, McDermott A, Zeger SL, Samet JM (2002) On the use of generalized additive models in time-series studies of air pollution and health. Am J Epidemiol 156(3):193–203
Elshahidi MH (2019) Outdoor air pollution and gestational diabetes mellitus: a systematic review and meta-analysis. Iran J Public health 48(1):9
Endeshaw G, Berhan Y (2015) Perinatal outcome in women with hypertensive disorders of pregnancy: a retrospective cohort study. Int Scholarly Res Notices 2015:1–8
Enkhmaa D et al (2014) Seasonal ambient air pollution correlates strongly with spontaneous abortion in Mongolia. BMC Pregnancy Childb 14(1):146
Evenson DP, Wixon R (2005) Environmental toxicants cause sperm DNA fragmentation as detected by the Sperm Chromatin Structure Assay (SCSA®). Toxicol Appl Pharmacol 207(2):532–537
Faiz AS, Rhoads GG, Demissie K, Kruse L, Lin Y, Rich DQ (2012) Ambient air pollution and the risk of stillbirth. Am J Epidemiol 176(4):308–316
Faiz AS, Rhoads GG, Demissie K, Lin Y, Kruse L, Rich DQ (2013) Does ambient air pollution trigger stillbirth? Epidemiology 24(4):538–544
Fleisch AF et al (2014) Air pollution exposure and abnormal glucose tolerance during pregnancy: the project Viva cohort. Environ Health Perspect 122(4):378–383
Fleisch AF, Kloog I, Luttmann-Gibson H, Gold DR, Oken E, Schwartz JD (2016) Air pollution exposure and gestational diabetes mellitus among pregnant women in Massachusetts: a cohort study. Environmental Health 15(1):40
Ghorbani M, Firouz Zare A (2010) Valuation of different characteristics of air pollution in Mashhad. J Econ Res 44(89):215–241
Green R, Sarovar V, Malig B, Basu R (2015) Association of stillbirth with ambient air pollution in a California cohort study. Am J Epidemiol 181(11):874–882
Hackley B, Feinstein A, Dixon J (2007) Air pollution: impact on maternal and perinatal health. J Midwifery Women's Health 52(5):435–443
Hafez A, Fahim H, Badawy H (2001) Socioenvironmental predictors of abortion and stillbirths in an industrial community in Egypt. J Egypt Public Health Assoc 76(1–2):1–16
Hampel R et al (2011) Short-term impact of ambient air pollution and air temperature on blood pressure among pregnant women. Epidemiology 22(5):671–679
He X-J, Qin F-y, Hu C-L, Zhu M, Tian C-Q, Li L (2015) Is gestational diabetes mellitus an independent risk factor for macrosomia: a meta-analysis? Arch Gynecol Obstet 291(4):729–735
Hernandez TL, Friedman JE, Van Pelt RE, Barbour LA (2011) Patterns of Glycemia in Normal Pregnancy: Should the current therapeutic targets be challenged? Diabetes Care 34(7):1660–1668
Hosseini V, Shahbazi H (2016) Urban air pollution in Iran. Iran Stud 49(6):1029–1046
Hou HY, Wang D, Zou XP, Yang ZH, Li T-C, Chen YQ (2014) Does ambient air pollutants increase the risk of fetal loss? A case–control study. Arch Gynecol Obstet 289(2):285–291
Hu H, Ha S, Roth J, Kearney G, Talbott EO, Xu X (2014) Ambient air pollution and hypertensive disorders of pregnancy: a systematic review and meta-analysis. Atmos Environ 97:336–345
Hu H et al (2015) Association of atmospheric particulate matter and ozone with gestational diabetes mellitus. Environ Health Perspect 123(9):853–859
Hwang B-F, Lee YL, Jaakkola JJ (2011) Air pollution and stillbirth: a population-based case–control study in Taiwan. Environ Health Perspect 119(9):1345–1349
Jin L et al (2015) Ambient air pollution and congenital heart defects in Lanzhou, China. Environ Res Lett 10(7):074005
Kioumourtzoglou M-A, Raz R, Wilson A, Fluss R, Nirel R, Broday DM (2019) Traffic-related air pollution and pregnancy loss. Epidemiology (Cambridge, Mass) 30(1):4
Koyanagi A et al (2013) Macrosomia in 23 developing countries: an analysis of a multicountry, facility-based, cross-sectional survey. The Lancet 381(9865):476–483
Lee P-C et al (2012) Ambient air pollution exposure and blood pressure changes during pregnancy. Environ Res 117:46–53
Lee P-C, Roberts JM, Catov JM, Talbott EO, Ritz B (2013) First trimester exposure to ambient air pollution, pregnancy complications and adverse birth outcomes in Allegheny County, PA. Mater Child Health J 17(3):545–555
Leiser CL et al (2019) Acute effects of air pollutants on spontaneous pregnancy loss: a case-crossover study. Fertil Steril 111(2):341–347
Lu M-C, Wang P, Cheng T-J, Yang C-P, Yan Y-H (2017) Association of temporal distribution of fine particulate matter with glucose homeostasis during pregnancy in women of Chiayi City, Taiwan. Taiwan Environ Res 152:81–87
Lucchesi M, Shochat G (2001) Toxicity, carbon monoxide. Eur Med J 10(10):1–16
Makri A, Stilianakis NI (2008) Vulnerability to air pollution health effects. Int J Hyg Environ Health 211(3–4):326–336
Malmqvist E, Jakobsson K, Tinnerberg H, Rignell-Hydbom A, Rylander L (2013) Gestational diabetes and preeclampsia in association with air pollution at levels below current air quality guidelines. Environ Health Perspect 121(4):488–493
Männistö T, Mendola P, Liu D, Leishear K, Sherman S, Laughon SK (2014) Acute air pollution exposure and blood pressure at delivery among women with and without hypertension. Am J Hypertens 28(1):58–72
Moradi Y et al (2019) Complications of type 2 diabetes in Iranian population: an updated systematic review and meta-analysis. Diabetes Metab Syndr Clin Res Rev 13(3):2300–2312
Olsson D, Mogren I, Forsberg B (2013) Air pollution exposure in early pregnancy and adverse pregnancy outcomes: a register-based cohort study. BMJ open 3(2):e001955
Pan S-C, Huang C-C, Lin S-J, Chen B-Y, Chan C-C, Guo Y-LL (2017) Gestational diabetes mellitus was related to ambient air pollutant nitric oxide during early gestation. Environ Res 158:318–323
Pedersen M et al (2014) Ambient air pollution and pregnancy-induced hypertensive disorders: a systematic review and meta-analysis. Hypertension 64(3):494–500
Pedersen M et al (2017a) Impact of road traffic pollution on pre-eclampsia and pregnancy-induced hypertensive disorders. Epidemiology (Cambridge, Mass) 28(1):99
Pedersen M et al (2017b) Gestational diabetes mellitus and exposure to ambient air pollution and road traffic noise: a cohort study. Environ Int 108:253–260
Pereira LA et al (1998) Association between air pollution and intrauterine mortality in São Paulo, Brazil. Environ Health Perspect 106(6):325–329
Pereira G, Haggar F, Shand AW, Bower C, Cook A, Nassar N (2013) Association between pre-eclampsia and locally derived traffic-related air pollution: a retrospective cohort study. J Epidemiol Community Health 67(2):147–152
Phung D et al (2016) Air pollution and risk of respiratory and cardiovascular hospitalizations in the most populous city in Vietnam. Sci Total Environ 557:322–330
Pigott TD (2001) A review of methods for missing data. Educ Res Eval 7(4):353–383. https://doi.org/10.1076/edre.7.4.353.8937
Poursafa P, Mansourian M, Motlagh M-E, Ardalan G, Kelishadi R (2014) Is air quality index associated with cardiometabolic risk factors in adolescents? The CASPIAN-III study. Environ Res 134:105–109
Rajagopalan S, Brook RD (2012) Air pollution and type 2 diabetes: mechanistic insights. Diabetes 61(12):3037–3045
Rankin J, Chadwick T, Natarajan M, Howel D, Pearce MS, Pless-Mulloli T (2009) Maternal exposure to ambient air pollutants and risk of congenital anomalies. Environ Res 109(2):181–187
Roberts J, Cooper DW (2001) Pathogenesis and genetics of pre-eclampsia. The Lancet 357(9249):53–56
Robledo CA et al (2015) Preconception and early pregnancy air pollution exposures and risk of gestational diabetes mellitus. Environ Res 137:316–322
Rosa MD et al (2003) Traffic pollutants affect fertility in men. Hum Reprod 18(5):1055–1061
Rubes J et al (2005) Episodic air pollution is associated with increased DNA fragmentation in human sperm without other changes in semen quality. Hum Reprod 20(10):2776–2783
Savitz DA et al (2015) Ambient fine particulate matter, nitrogen dioxide, and hypertensive disorders of pregnancy in New York City. Epidemiology (Cambridge, Mass) 26(5):748
Schulz M, Romppel M, Grande G (2016) Built environment and health: a systematic review of studies in Germany. J Public Health 40(1):8–15
Shah PS, Balkhair T, births KSGoDoPL, (2011) Air pollution and birth outcomes: a systematic review. Environ Int 37(2):498–516
Shen H-N, Hua S-Y, Chiu C-T, Li C-Y (2017) Maternal exposure to air pollutants and risk of gestational diabetes mellitus in Taiwan. Int J Environ Res Public Health 14(12):1604
Siddika N, Balogun HA, Amegah AK, Jaakkola JJ (2016) Prenatal ambient air pollution exposure and the risk of stillbirth: systematic review and meta-analysis of the empirical evidence. Occup Environ Med 73(9):573–581
Šrám RJ, Binková B, Dejmek J, Bobak M (2005) Ambient air pollution and pregnancy outcomes: a review of the literature. Environ Health Perspect 113(4):375–382
Stieb DM, Chen L, Eshoul M, Judek S (2012) Ambient air pollution, birth weight and preterm birth: a systematic review and meta-analysis. Environ Res 117:100–111
Stieb DM et al (2015) Associations of pregnancy outcomes and PM2.5 in a national Canadian study. Environ Health Perspect 124(2):243–249
van den Hooven EH et al (2011) Air pollution, blood pressure, and the risk of hypertensive complications during pregnancy: the generation R study. Hypertension 57(3):406–412
Ver Hoef JM, Boveng PL (2007) Quasi-Poisson vs. negative binomial regression: how should we model overdispersed count data? Ecology 88(11):2766–2772. https://doi.org/10.1890/07-0043.1
Veras MM et al (2008) Particulate urban air pollution affects the functional morphology of mouse placenta. Biol Reprod 79(3):578–584
Wang M et al (2018) Association between short-term exposure to air pollution and dyslipidemias among type 2 diabetic patients in northwest China: a population-based study. Int J Environ Res Public Health 15(4):631
World Health Organization (2006) Occupational and Environmental Health Team. WHO Air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide: global update 2005: summary of risk assessment. World Health Organization. https://apps.who.int/iris/handle/10665/69477. Accessed Sept 2020
World Health Organization (2017) The cost of a polluted environment: 1.7 million child deaths a year, says WHO. https://www.who.int/en/news-room/detail/06-03-2017-the-cost-of-a-polluted-environment-1-7-million-child-deaths-a-year-says-who. Accessed Sept 2020
Wilhelm M, Ritz B (2005) Local variations in CO and particulate air pollution and adverse birth outcomes in Los Angeles County, California, USA. Environ Health Perspect 113(9):1212–1221
Wood SN (2006) Generalized additive models: an introduction with R, vol 66. Chapman & Hall/CRC, Boca Raton, Florida. ISBN 1-58488-474-6
Wood SN (2008) Fast stable direct fitting and smoothness selection for generalized additive models. J R Stat Soc Ser B (Statistical Methodology) 70(3):495–518
Wood S (2012) mgcv: mixed GAM computation vehicle with GCV/AIC/REML smoothness estimation. R package version 1.7-17. http://CRAN.R-project.org/package=mgcv
Wood SN (2017) Generalized additive models: an introduction. R. Chapman and Hall/CRC, Boca Roton
Xia B et al (2019) Personal exposure to PM2. 5 constituents associated with gestational blood pressure and endothelial dysfunction. Environ Pollut 250:346–356
Xiong L et al (2019) Acute effects of air pollutants on adverse birth outcomes in Changsha, China: a population data with time-series analysis from 2015 to 2017. Medicine 98(3):1–8
Xu X, Hu H, Ha S, Roth J (2014) Ambient air pollution and hypertensive disorder of pregnancy. J Epidemiol Community Health 68(1):13–20
Yang S et al (2018a) Ambient air pollution the risk of stillbirth: a prospective birth cohort study in Wuhan, China. Int J Hyg Environ Health 221(3):502–509
Yang Y-L, Yang H-L, Shiao S (2018b) Meta-prediction of MTHFR gene polymorphisms and air pollution on the risk of hypertensive disorders in pregnancy worldwide. Int J Environ Res Public Health 15(2):326
Ye X et al (2016) Acute effects of particulate air pollution on the incidence of coronary heart disease in Shanghai, China. PLoS ONE 11(3):e0151119
Yorifuji T et al (2012) Residential proximity to major roads and placenta/birth weight ratio. Sci Total Environ 414:98–102
Yorifuji T, Naruse H, Kashima S, Murakoshi T, Doni H (2015) Residential proximity to major roads and obstetrical complications. Sci Total Environ 508:188–192
Zang H et al (2019) Ambient air pollution and the risk of stillbirth: a population-based prospective birth cohort study in the coastal area of China. Environ Sci Pollut Res Int 26(7):6717–6724. https://doi.org/10.1007/s11356-019-04157-7
Acknowledgements
The authors wish to express their gratitude to Ms. Yalda Sabbaghan for her kind assistance.
Funding
This study was funded and supported by Ahvaz Jundishapur University of Medical Sciences, Grant no.: APRD-9609.
Author information
Authors and Affiliations
Contributions
MD, FE and MC conceived and designed the project. MD, GG and RS acquired the data. MD and AM analyzed and interpreted the data. FE, ZS and NK wrote the paper. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest was declared by the author.
Ethical approval
Ethics License of the present study was acquired from the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Code of ethics: IR.AJUMS.REC.1396.793). According to the national guidelines, studies such as this do not require individual consent.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original article was revised due to an error in Table 3.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dastoorpoor, M., Khanjani, N., Moradgholi, A. et al. Prenatal exposure to ambient air pollution and adverse pregnancy outcomes in Ahvaz, Iran: a generalized additive model. Int Arch Occup Environ Health 94, 309–324 (2021). https://doi.org/10.1007/s00420-020-01577-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-020-01577-8