Abstract
Purpose
To evaluate the visual field after anti-vascular endothelial growth factor (VEGF) therapy and laser treatment for retinopathy of prematurity.
Method
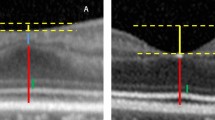
Retrospective cohort study. Infants with retinopathy of prematurity treated by anti-VEGF therapy or laser treatment were included in the study. Degrees of visual field in eight directions examined by Goldmann perimeter (intensity, 1000 apostilb; size, V4e = 64 mm2) were compared between the anti-VEGF therapy and laser treatment groups. The visual acuity (VA) and spherical equivalent refraction were also compared between the two groups.
Results
Nine eyes with anti-VEGF therapy and 12 eyes with laser treatment were enrolled in the analysis. The total, upper, nasal upper, nasal, nasal lower, temporal lower, and temporal upper visual fields were significantly wider in the eyes with anti-VEGF therapy than in those with laser treatment (496 vs 416, P = .002; 53 vs 45, P = .008; 56 vs 43, P = .003; 58 vs 39, P < .001; 55 vs 44, P = .01; 72 vs 65, P = .01; and 62 vs 56, P = .03, respectively). The logarithm of the minimum angle of resolution VA tended to be better in the eyes with anti-VEGF therapy than in those with laser treatment (0.01 vs 0.15, P = .06). Eyes with anti-VEGF therapy had significantly lower myopia than those with laser treatment (spherical equivalent refraction: -0.72 vs -5.7, P = .001).
Conclusion
Anti-VEGF therapy may provide a wider visual field, better VA, and less myopia compared with laser treatment.


Similar content being viewed by others
References
Gilbert C (2008) Retinopathy of prematurity: a global perspective of the epidemics, population of babies at risk and implications for control. Early Hum Dev 84:77–82. https://doi.org/10.1016/j.earlhumdev.2007.11.009
Quinn GE, Dobson V, Davitt BV, Hardy RJ, Tung B, Pedroza C, Good WV, Early Treatment for Retinopathy of Prematurity Cooperative G (2008) Progression of myopia and high myopia in the early treatment for retinopathy of prematurity study: findings to 3 years of age. Ophthalmology 115:1058-1064 e1051. https://doi.org/10.1016/j.ophtha.2007.07.028
Quinn GE, Dobson V, Davitt BV, Wallace DK, Hardy RJ, Tung B, Lai D, Good WV, Early Treatment for Retinopathy of Prematurity Cooperative G (2013) Progression of myopia and high myopia in the early treatment for retinopathy of prematurity study: findings at 4 to 6 years of age. J AAPOS 17:124–128. https://doi.org/10.1016/j.jaapos.2012.10.025
McLoone E, O’Keefe M, McLoone S, Lanigan B (2007) Effect of diode laser retinal ablative therapy for threshold retinopathy of prematurity on the visual field: results of Goldmann perimetry at a mean age of 11 years. J Pediatr Ophthalmol Strabismus 44:170–173. https://doi.org/10.3928/0191-3913-20070301-10
Early Treatment For Retinopathy Of Prematurity Cooperative G (2003) Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol 121:1684–1694. https://doi.org/10.1001/archopht.121.12.1684
Mintz-Hittner HA, Kennedy KA, Chuang AZ, Group B-RC (2011) Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med 364:603–615. https://doi.org/10.1056/NEJMoa1007374
Geloneck MM, Chuang AZ, Clark WL, Hunt MG, Norman AA, Packwood EA, Tawansy KA, Mintz-Hittner HA, Group B-RC (2014) Refractive outcomes following bevacizumab monotherapy compared with conventional laser treatment: a randomized clinical trial. JAMA Ophthalmol 132(1327):1333. https://doi.org/10.1001/jamaophthalmol.2014.2772
Pertl L, Steinwender G, Mayer C, Hausberger S, Poschl EM, Wackernagel W, Wedrich A, El-Shabrawi Y, Haas A (2015) A systematic review and meta-analysis on the safety of vascular endothelial growth factor (VEGF) inhibitors for the treatment of retinopathy of prematurity. PLoS One 10:e0129383. https://doi.org/10.1371/journal.pone.0129383
Tahija SG, Hersetyati R, Lam GC, Kusaka S, McMenamin PG (2014) Fluorescein angiographic observations of peripheral retinal vessel growth in infants after intravitreal injection of bevacizumab as sole therapy for zone I and posterior zone II retinopathy of prematurity. Br J Ophthalmol 98:507–512. https://doi.org/10.1136/bjophthalmol-2013-304109
Roohipoor R, Karkhaneh R, Riazi-Esfahani M, Dastjani Farahani A, Khodabandeh A, Ebrahimi Adib N, Imani M, Khojasteh Jafari H, Riazi-Esfahani H, Hosseinpour J, Zarei M, Ghasemi H, Mirghorbani M, Yaseri M, Davoudi S, Modjtahedi BS (2018) Comparison of intravitreal bevacizumab and laser photocoagulation in the treatment of retinopathy of prematurity. Ophthalmol Retin 2:942–948. https://doi.org/10.1016/j.oret.2018.01.017
Perente I, Eris E, Seymen Z, Cevik SG, Bekmez S (2019) Aggressive posterior retinopathy of prematurity treated with intravitreal bevacizumab: late period fluorescein angiographic findings. Graefes Arch Clin Exp Ophthalmol 257:1141–1146. https://doi.org/10.1007/s00417-019-04292-4
Lepore D, Quinn GE, Molle F, Orazi L, Baldascino A, Ji MH, Sammartino M, Sbaraglia F, Ricci D, Mercuri E (2018) Follow-up to age 4 years of treatment of type 1 retinopathy of prematurity intravitreal bevacizumab injection versus laser: fluorescein angiographic findings. Ophthalmology 125:218–226. https://doi.org/10.1016/j.ophtha.2017.08.005
Lorenz B, Stieger K, Jager M, Mais C, Stieger S, Andrassi-Darida M (2017) Retinal vascular development with 0.312 mg intravitreal bevacizumab to treat severe posterior retinopathy of prematurity: a longitudinal fluorescein angiographic study. Retina 37:97–111. https://doi.org/10.1097/IAE.0000000000001126
International Committee for the Classification of Retinopathy of P (2005) The international classification of retinopathy of prematurity revisited. Arch Ophthalmol 123:991–999. https://doi.org/10.1001/archopht.123.7.991
Hajrasouliha AR, Garcia-Gonzales JM, Shapiro MJ, Yoon H, Blair MP (2017) Reactivation of retinopathy of prematurity three years after treatment with bevacizumab. Ophthalmic Surg Lasers Imaging Retina 48:255–259. https://doi.org/10.3928/23258160-20170301-10
Snyder LL, Garcia-Gonzalez JM, Shapiro MJ, Blair MP (2016) Very late reactivation of retinopathy of prematurity after monotherapy with intravitreal bevacizumab. Ophthalmic Surg Lasers Imaging Retina 47:280–283. https://doi.org/10.3928/23258160-20160229-12
Ittiara S, Blair MP, Shapiro MJ, Lichtenstein SJ (2013) Exudative retinopathy and detachment: a late reactivation of retinopathy of prematurity after intravitreal bevacizumab. J AAPOS 17:323–325. https://doi.org/10.1016/j.jaapos.2013.01.004
Gundlach BS, Kokhanov A, Altendahl M, Suh SY, Fung S, Demer J, Pineles S, Khitri M, Chu A, Tsui I (2022) Real-world visual outcomes of laser and anti-VEGF treatments for retinopathy of prematurity. Am J Ophthalmol 238:86–96. https://doi.org/10.1016/j.ajo.2021.11.015
Lee YS, See LC, Chang SH, Wang NK, Hwang YS, Lai CC, Chen KJ, Wu WC (2018) Macular structures, optical components, and visual acuity in preschool children after intravitreal bevacizumab or laser treatment. Am J Ophthalmol 192:20–30. https://doi.org/10.1016/j.ajo.2018.05.002
Chen YC, Chen SN (2020) Foveal microvasculature, refractive errors, optical biometry and their correlations in school-aged children with retinopathy of prematurity after intravitreal antivascular endothelial growth factors or laser photocoagulation. Br J Ophthalmol 104:691–696. https://doi.org/10.1136/bjophthalmol-2019-314610
Zhao J, Wu Z, Lam W, Yang M, Chen L, Zheng L, Zhang F, Zeng J, Wang J, Zhang G (2020) Comparison of OCT angiography in children with a history of intravitreal injection of ranibizumab versus laser photocoagulation for retinopathy of prematurity. Br J Ophthalmol 104:1556–1560. https://doi.org/10.1136/bjophthalmol-2019-315520
Inoue T, Asaoka R, Hashimoto Y, Kitamoto K, Kitano M, Fujita A, Azuma K, Yamamoto K, Nagahara M, Kadonosono K, Obata R (2021) Does the number of laser applications for ROP treatment influence the degree of myopia? Graefes Arch Clin Exp Ophthalmol 259:317–322. https://doi.org/10.1007/s00417-020-04946-8
Matsumura S, Matsumoto T, Katayama Y, Tomita M, Morikawa H, Itokawa T, Kawakami M, Hori Y (2022) Risk factors for early-onset high myopia after treatment for retinopathy of prematurity. Jpn J Ophthalmol 66:386–393. https://doi.org/10.1007/s10384-022-00921-4
Quinn GE, Fea AM, Minguini N (1991) Visual fields in 4- to 10-year-old children using Goldmann and double-arc perimeters. J Pediatr Ophthalmol Strabismus 28:314–319. https://doi.org/10.3928/0191-3913-19911101-07
Acknowledgements
We thank Robert Blakytny, D. Phil., from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was approved by the Institutional Review Board/Ethics Committee of Shiga University of Medical Science (Otsu, Japan).
Consent to participate
For this study, an opt-out consent process was used at Shiga University of Medical Science Hospital after approval by the Institutional Review Board.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Obata, S., Matsumoto, R., Iwasa, M. et al. Visual field after anti-vascular endothelial growth factor therapy and laser treatment for retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol 261, 3207–3213 (2023). https://doi.org/10.1007/s00417-023-06227-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06227-6